Prevention of Postoperative Pneumonia - Surgical Patient Care Series
←
→
Page content transcription
If your browser does not render page correctly, please read the page content below
Surgical Patient Care Series
Series Editor: Kamal M.F. Itani, MD
Prevention of Postoperative Pneumonia
Marin H. Kollef, MD
H
ospital-acquired pneumonia (HAP) is defined as
pneumonia that develops 48 hours or more TAKE HOME POINTS
after hospital admission, which was not in-
cubating at the time of admission (Table 1). • Postoperative pneumonia is defined as hospital-
Ventilator-associated pneumonia (VAP) refers to pneumo- acquired or ventilator-associated pneumonia in a
nia that develops more than 48 to 72 hours after endo- postsurgical patient.
tracheal intubation. Postoperative pneumonia is HAP or • Postoperative pneumonia is usually caused by bac-
VAP that occurs in a postoperative patient. teria and may be polymicrobial. Most infections are
HAP is the second most common nosocomial infec- caused by gram-negative aerobes.
tion in the United States after urinary tract infection • Three pathogenic mechanisms are responsible
but is the leading cause of mortality attributed to noso- for the development of postoperative pneumonia:
comial infection.1 Furthermore, HAP prolongs hospi- (1) colonization of the aerodigestive tract with
tal stays for an average of 7 to 9 days and adds excess pathogenic bacteria; (2) aspiration of contaminated
medical costs ranging from $12,000 to $40,000 per pa- secretions; and (3) impaired host defenses due to
tient.2–4 “Attributable mortality” from HAP is estimated critical illness and its therapy or other nonmodifi-
to be between 33% and 50%.5–7 able host factors.
There is convincing evidence that specific interven- • Prophylactic approaches may be nonpharmaco-
tions can be employed to prevent HAP/VAP and post- logic and pharmacologic. In general, nonpharma-
operative pneumonia. The higher morbidity, hospital cologic interventions are less expensive and easier
mortality, and excess hospital costs attributable to these to apply than pharmacologic interventions. Preven-
infections should make implementation of preven- tive measures should be tailored to the patient’s
tive strategies a priority among hospitals. Mandatory specific risk factors for developing pneumonia.
education programs for health care workers caring
for postoperative patients, adherence to infection-
control practices, and surveillance of local nosocomial
infection rates are all important strategies for effec- nas aeruginosa, Enterobacter species, Klebsiella pneumoniae,
tive prevention of postoperative pneumonia. This ar- Acinetobacter species, Serratia and Citrobacter species, and
ticle, which is the second in a series addressing recent Stenotrophomonas species.9,10 Methicillin-resistant Staphylo-
evidence-based recommendations for improving the coccus aureus (MRSA) is the predominant gram-positive
quality and safety of surgical care, reviews the etiology, pathogen accounting for nosocomial pneumonia in
pathogenesis, and prevention of postoperative pneu- the United States11 and is more common in patients
monia. In addition, an illustrative case is provided to with diabetes mellitus or head trauma.12 Anaerobic bac-
demonstrate the approach to evaluating and treating a teria rarely cause HAP/VAP despite being commonly
patient with postoperative pneumonia. associated with aspiration pneumonia in nonintubated
patients.13 Fungal and viral pathogens are very rare
ETIOLOGY AND PATHOGENESIS OF POSTOPERATIVE
PNEUMONIA
Etiology
Postoperative pneumonia is typically caused by bac- Dr. Itani is a professor of surgery, Boston University; an associate chief of sur-
gery, Boston Medical Center and Brigham & Women’s Hospital, and chief of
teria and may be polymicrobial, especially in patients
surgery, Boston Veteran’s Administration Health Care System, Boston, MA.
with acute respiratory distress syndrome (ARDS).8 The Dr. Kollef is a professor of medicine, Division of Pulmonary and Critical Care
majority of infections are caused by gram-negative aer- Medicine, Washington University School of Medicine, St. Louis, MO; and a
obes; organisms commonly isolated include Pseudomo- Director, Medical Critical Care, Barnes-Jewish Hospital, St. Louis, MO.
www.turner-white.com Hospital Physician September 2007 47Kollef : Prevention of Pneumonia : pp. 47–60, 64
Table 1. Clinical Definitions of Pneumonia is a prerequisite for postoperative pneumonia to de-
velop.17 The pathogens replace normal host flora for
Category Definition
several reasons, including broad-spectrum antibiotic
Community-acquired Patient with a first positive bacterial cul- use, stress ulcer prophylaxis (which modifies the stom-
pneumonia ture obtained ≤ 48 hr after hospital ad-
mission and lacking risk factors for health
ach pH and environment and predisposes to gastric
care–associated pneumonia colonization), and the presence of medical devices in
Health care–associated Patient with a first positive bacterial cul- the aerodigestive tract (eg, endotracheal and nasogas-
pneumonia ture obtained ≤ 48 hr after hospital ad- tric tubes). The host airway becomes desiccated, and
mission and any of the following: the mucociliary elevator system is bypassed or becomes
• Admission source indicates transfer ineffectual. The pathogens are able to adhere to epi-
from another health care facility
• Receiving hemodialysis, wound, or
thelial cells in the upper and lower airway and flourish
infusion therapy as an outpatient in this environment.18 They release microbial products
• Prior hospitalization for ≥ 3 days that contribute to biofilm formation and a continuous
within past 90 days source of pathogenic bacteria, which can gain access
• Immunocompromised state due to to the tracheobronchial tree via aspiration of infected
underlying disease or therapy
secretions with each cycle of the ventilator.19
Hospital-acquired Patient with a first positive bacterial culture
pneumonia (HAP) obtained > 48 hr after hospital admission
Aspiration of secretions is ubiquitous in an environ-
Ventilator-associated Mechanically ventilated patient with a first
ment where the glottis is bypassed. In addition, the
pneumonia (VAP) positive bacterial culture obtained > 48 hr supine position, gastric overdistention, and enteral
after hospital admission or tracheal intu- feedings all contribute to aspiration risk.20 Nebulization
bation, whichever occurred first devices and ventilator circuits that become contami-
Postoperative pneu- HAP or VAP occurring in a postoperative nated by purulent secretions enable pathogens to be
monia patient aerosolized into the tracheobronchial tree with the
NOTE: Clinical criteria for pneumonia include new or progressive help of positive pressure ventilation. Frequent patient
lung infiltrate and at least 2 of the following: hyper- or hypothermia, el- transportation, inadequate subglottic suctioning, and
evated white blood cell count, purulent tracheal secretions or sputum, low endotracheal tube cuff pressure may also contrib-
and worsening oxygenation. ute to VAP development.
The patient may also exhibit a number of nonmodi-
fiable risk factors that uniquely predispose to HAP/
causes of HAP/VAP in immunocompetent hosts.14 VAP by lowering host defense mechanisms. These
Multidrug-resistant pathogens are an increasing prob- include male sex, age greater than 60 years, ARDS,
lem, and prevalence varies by patient population and multisystem organ failure, coma, chronic obstructive
by hospital and type of intensive care unit (ICU), em- pulmonary disease (COPD), tracheostomy placement,
phasizing the need for local surveillance programs.15 reintubation, neurosurgery, and head trauma with
intracranial pressure monitoring.21
Pathogenesis
Postoperative pneumonia risk is influenced by a APPROACH TO SUSPECTED POSTOPERATIVE
number of risk factors that become relevant in hosts PNEUMONIA
who are exposed to a nosocomial environment. Many Case Presentation
of the risk factors are modifiable, and awareness of these A 68-year-old man with a history of adult-onset dia-
factors as well as attempts to limit their occurrence is betes, congestive heart failure (ejection fraction, 32%),
paramount to reducing HAP/VAP rates. All risk factors and hypertension is admitted to the hospital with
can be grouped into 1 of 3 pathogenetic mechanisms: abdominal pain. The patient has a 55 pack-year smok-
colonization of the aerodigestive tract with pathogenic ing history and admits to occasional alcohol ingestion.
bacteria, aspiration of contaminated secretions, and He was hospitalized 4 months earlier for pulmonary
impaired host defenses due to critical illness and its edema related to his underlying heart failure.
therapies or other nonmodifiable host factors.16 Dura- On hospital admission, the patient is found to have lab-
tion of exposure to the health care environment and oratory and radiographic evidence consistent with ische
prior antibiotic exposure also are important factors in mic colitis and subsequently undergoes a complete colec-
the development of nosocomial pneumonia, including tomy. The preoperative chest radiograph showed cardio-
postoperative pneumonia. megaly, with no acute pulmonary process. The surgical
Colonization of the aerodigestive tract by pathogens procedure was uneventful, and perioperative laboratory
48 Hospital Physician September 2007 www.turner-white.comKollef : Prevention of Pneumonia : pp. 47–60, 64
Table 2. Noninfectious Causes of Fever and Pulmonary
Infiltrates Mimicking Postoperative Pneumonia
Chemical aspiration without infection
Atelectasis
Pulmonary embolism
Acute respiratory distress syndrome
Pulmonary hemorrhage
Lung contusion
Infiltrative tumor
Radiation pneumonitis
Drug reaction
Bronchiolitis obliterans organizing pneumonia
Figure 1. Chest radiograph demonstrating a new pulmonary infil cal errors resulted in the unnecessary prescription of
trate involving the right lower and upper lobes. antibiotics, failure to diagnose VAP accurately, failure to
treat all organisms causing polymicrobial VAP, and fail-
ure to treat VAP due to antibiotic-resistant pathogens.24
evaluation showed no evidence of myocardial ischemia. Not all studies, however, have concluded that clini-
Unfortunately, the patient does not liberate from me- cal diagnosis of VAP is markedly inferior to other
chanical ventilation due to poor respiratory efforts associ- methods. For example, a study of 25 deceased me-
ated with spontaneous breathing trials. On the third hos- chanically ventilated patients found that the presence
pital day, the patient’s temperature is 38.5°C and white of radiographic infiltrates and 2 of 3 clinical criteria
blood cell count is 16,000/mL, and a chest radiograph (fever, leukocytosis, purulent secretions) had a sensitiv-
shows evidence of new pulmonary infiltrates (Figure 1). ity of 69% and a specificity of 75%, with the combina-
tion of histologic evidence of pneumonia and positive
• What is the differential diagnosis for this patient’s
postmortem cultures as the gold standard.25
new pulmonary infiltrates?
• How is the diagnosis of postoperative pneumonia in
Postoperative pneumonia usually is suspected when
a ventilated patient confirmed?
a patient develops a new or progressive pulmonary
infiltrate with fever, leukocytosis, and purulent tracheo- Lower respiratory sampling methods including
bronchial secretions.2,22 However, these clinical criteria bronchoalveolar lavage (BAL) and protected specimen
are nonspecific for the diagnosis of postoperative brush can more accurately confirm the presence or ab
pneumonia, and therefore a number of noninfectious sence of pneumonia and facilitate the modification of
causes of fever and pulmonary infiltrates also must be empirically prescribed antibiotic therapy. The airway of
considered (Table 2). mechanically ventilated patients is commonly colonized
Several studies have demonstrated the limitations with potentially pathogenic bacteria. Consequently,
of using clinical and radiographic parameters alone secretions obtained from an endotracheal or trache-
for establishing the diagnosis of HAP/VAP.23,24 Autopsy ostomy tube cannot consistently differentiate between
results in a series of patients with acute lung injury dem- upper airway colonization and lower respiratory tract
onstrated that clinical criteria alone led to an incorrect infection.2 Sampling methods that minimize contami-
diagnosis of VAP in 29% of clinically suspected cases.23 nation from the upper airway (eg, bronchoscopic or
In another study, the accuracy of clinical judgment in blind catheter BAL and brushing) offer the advantage
formulating treatment plans for patients with suspected of establishing a more precise microbiologic diagnosis
VAP was compared with quantitative lower airway cul- of VAP to guide subsequent antimicrobial choices.26
tures obtained by bronchoscopy; clinical judgments The use of BAL for the microbiologic diagnosis of
about the presence of VAP were correct only 62% of VAP appears to be associated with greater confidence
the time when compared with culture specimens, and among clinicians that the culture results actually re-
only 33% of the treatment plans based on clinical judg- flect the presence or absence of VAP and the etiologic
ment alone were deemed to be effective.24 Most clini- agents of infection.2 The main apparent advantage
www.turner-white.com Hospital Physician September 2007 49Kollef : Prevention of Pneumonia : pp. 47–60, 64
38.6 fection, or prior antibiotic exposure during the current
38.5 360 hospitalization).29 An initial combination antimicrobial
38.4 340 regimen should be prescribed in patients with suspect-
Body temperature (°C)
38.3 320 ed postoperative pneumonia having these risk factors
PaO2/FIO2 ratio
38.2 300 in order to appropriately treat potentially antibiotic-
38.1 280 resistant pathogens including MRSA and P. aeruginosa.29
38.0 260
The subsequent availability of microorganism iden-
37.9 240
tification and antibiotic susceptibility testing allows for
37.8 220
antimicrobial de-escalation to occur when appropri-
37.7 200
ate. Antimicrobial de-escalation promotes narrowing
37.6 180
of the initial antimicrobial regimen and use of the
37.5
shortest duration of antibiotic therapy that is clinically
0 1 2 3 4 5 6 7 8 9 10
Day of Diagnosis of postoperative pneumonia effective. It is important that hospitals employ their
operation own local microbiologic data in formulating appropri-
Postoperative day ate initial antibiotic regimens for HAP/VAP.
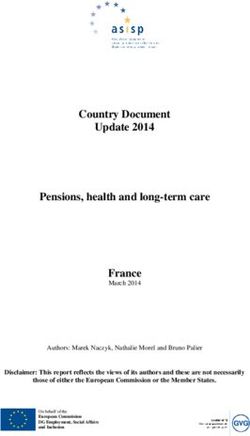
Figure 2. Graph of case patient’s body temperature (solid line)
and ratio of partial pressure of arterial oxygen to fraction of in-
Case Conclusion
spired oxygen (PaO2/FIO2 ratio; dotted line) following surgery. The patient undergoes BAL followed by administra-
tion of broad-spectrum antimicrobial agents with cov-
erage for MRSA and potentially resistant gram-negative
associated with obtaining properly collected and pro- bacteria. The Gram stain of the BAL specimen shows a
cessed lower respiratory tract samples in patients with predominance of neutrophils and gram-positive bacte-
suspected VAP is to enable more specific modification ria in clusters that subsequently are identified as MRSA.
of initial empiric antibiotic regimens. This has been The patient is treated for MRSA pneumonia (linezolid
demonstrated for both medical and surgical patients. 600 mg twice daily), and the antibiotic regimen is con-
A recent meta-analysis of 4 randomized trials compar- tinued for 8 days. The patient’s response to therapy is
ing lower respiratory tract sampling with quantitative shown in Figure 2. Two sets of blood cultures drawn
cultures to clinical criteria for the diagnosis of VAP prior to beginning antibiotic therapy return negative
found that initial antibiotic therapy was almost 3 times for bacterial or fungal growth. The patient continues
more likely to be modified among patients random- to do poorly with spontaneous breathing trials, and a
ized to the former group.27 percutaneous tracheostomy tube is placed on day 8 of
mechanical ventilation. The patient is liberated from
• What is the next step in this patient’s management?
the ventilator on day 17 of mechanical ventilation and
In patients with clinically suspected postoperative is discharged to a nursing facility 21 days following
pneumonia, respiratory specimens for microbiologic hospital admission. The patient’s prolonged need for
processing should be obtained followed by timely ad- mechanical ventilation and hospitalization following
ministration of an empiric antibiotic regimen selected surgery was attributed to postoperative pneumonia
according to the presence or absence of risk factors for due to MRSA.
infection with antibiotic-resistant bacteria. Initial admin-
istration of an appropriate antibiotic (ie, to which the PREVENTION OF POSTOPERATIVE PNEUMONIA
pathogens are sensitive based on in vitro susceptibility Grading Risk and General Preventive Strategies
testing) is one of the primary determinants of hospital Postoperative pulmonary complications are com-
outcome over which the clinician has control. Use of an mon following both thoracic and nonthoracic opera-
initial antibiotic regimen that is inappropriate for the tions. To optimize the application of preventive strate-
microorganism(s) causing nosocomial pneumonia of all gies for postoperative pneumonia, clinicians must be
types has been associated with a significantly greater risk able to identify patients at risk for this complication
of death.28 These findings strongly suggest that initial an- and its variants. Arozullah and coworkers30 developed
timicrobial therapy for postoperative pneumonia should and validated a preoperative risk index for the predic-
be selected according to the presence or absence of risk tion of postoperative pneumonia; the identified risk
factors for health care–associated infection (eg, recent factors and their designated point values are shown in
hospitalization, admission from a nursing home, current Table 3. The investigators then divided patients into
hemodialysis, immunocompromised state, late-onset in- 5 risk categories based on their cumulative risk scores
50 Hospital Physician September 2007 www.turner-white.comKollef : Prevention of Pneumonia : pp. 47–60, 64
(ie, 1 = 0–15 points, 2 = 16–25 points, 3 = 26–40 Table 3. Postoperative Pneumonia Risk Index
points, 4 = 41–55 points, 5 = > 55 points); the incidence
Preoperative Risk Factor Point Value
of postoperative pneumonia rose from 1% at a risk
score of 1 to 15.3% at a risk score of 5 (Table 4). The Type of surgery
implication of these data is that patients at higher risk Abdominal aortic aneurysm repair 15
should receive more aggressive and dedicated inter- Thoracic 14
ventions aimed at the prevention of this complication. Upper abdominal 10
In addition to the specific preventive interventions Neck 8
detailed below, a general plan for the prevention of Neurosurgery 8
postoperative pulmonary complications should be in Vascular 3
place. This is important because patients with postop- Age
erative pulmonary complications spend more time in ≥ 80 yr 17
the hospital and more time on mechanical ventilation, 70–79 yr 13
2 factors that increase their risk for postoperative pneu- 60–69 yr 9
monia. A recent systematic review identified postopera- 50–59 yr 4
tive lung expansion maneuvers, selective nasogastric de- Functional status
compression, short-acting neuromuscular blockade, and Totally dependent 10
laparoscopic (versus open) operation as interventions Partially dependent 6
supported by the available medical literature to prevent Weight loss > 10% in past 6 mo 7
postoperative pulmonary complications (Table 5).31 The History of chronic obstructive pulmonary disease 5
evidence for other interventions including smoking ces- General anesthesia 4
sation, intraoperative neuraxial blockade, postoperative Impaired sensorium 4
epidural analgesia, immunomodulating enteral nutri- History of cerebrovascular accident 4
tion, routine total parenteral or enteral nutrition, and Blood urea nitrogen level
right-heart catheterization was either conflicting or did < 2.86 mmol/L (< 8 mg/dL) 4
not support the use of these specific interventions.31 7.85–10.7 mmol/L (22–30 mg/dL) 2
> 10.7 mmol/L (> 30 mg/dL) 3
Specific Preventive Strategies Transfusion > 4 U 3
In 2005, the American Thoracic Society (ATS) and Emergency surgery 3
the Infectious Diseases Society of America (IDSA) pub- Steroid use for chronic condition 3
lished guidelines for the management of adults with Current smoker within 1 yr 3
HAP, VAP, and health care–associated pneumonia.29 Alcohol intake > 2 drinks/day in past 2 wk 2
The ATS/IDSA guidelines used an evidence-based
grading system to rank recommendations, which was Adapted with permission from Arozullah AM, Khuri SF, Henderson
WG. Development and validation of a multifactorial risk index for
defined as follows: level I (high) evidence (evidence predicting postoperative pneumonia after major noncardiac surgery.
from well-conducted, randomized clinical trials); level II Ann Intern Med 2001;135:853.
(moderate) evidence (evidence from well-designed,
controlled trials without randomization, including
cohort studies, patient series, and case-control studies; get the prevention of aspiration events. Basic infection
also, any large case series in which systematic analysis control measures, which include hand disinfection
of disease patterns and/or microbial etiology was con- and local microbiologic surveillance, are important
ducted, as well as reports of new therapies that were to this approach. Pathogens causing postoperative
not collected in a randomized fashion); and level III pneumonia are ubiquitous in health care settings, and
(low) evidence (evidence from case studies and expert transmission of these bacteria to patients often occurs
opinion). The following discussion summarizes ATS/ via health care workers, whose hands become contami-
IDSA recommendations regarding interventions that nated or transiently colonized with the bacteria. Pro-
target modifiable risk factors for HAP. cedures such as tracheal suctioning and manipulation
Nonpharmacologic interventions. Nonpharmaco- of ventilator circuits increase the opportunity for cross-
logic approaches to the prevention of postoperative contamination with these pathogens. This risk can be
pneumonia (Table 6) are generally less expensive reduced by using aseptic technique and eliminating
and easier to apply than pharmacologic interventions pathogens from the hands of personnel.32 Alcohol-
(Table 7). Most nonpharmacologic interventions tar- based foams and lotions can increase compliance with
www.turner-white.com Hospital Physician September 2007 51Kollef : Prevention of Pneumonia : pp. 47–60, 64
Table 4. Distribution of Postoperative Pneumonia Risk Index Scores in Patients in the Development and Validation Cohorts
Risk Class
Variable 1 (0–15 points) 2 (16–25 points) 3 (26–40 points) 4 (41–55 points) 5 (> 55 points)
Development cohort patients, n (%) 69,333 (43) 55,757 (35) 32,103 (20) 3517 (2) 95 (0.1)
Average predicted probability of post- 0.24 (0.24–0.25) 1.20 (1.19–1.20) 4.0 (3.98–4.01) 9.4 (9.34–9.42) 15.3 (15.1–15.5)
operative pneumonia in development
cohort patients (95% CI), %
Rate of postoperative pneumonia in 0.24 1.19 4.0 9.4 15.8
development cohort patients, %
Rate of postoperative pneumonia in 0.24 1.18 4.6 10.8 15.9
validation cohort patients, %
Adapted with permission from Arozullah AM, Khuri SF, Henderson WG. Development and validation of a multifactorial risk index for predicting
postoperative pneumonia after major noncardiac surgery. Ann Intern Med 2001;135:853.
CI = confidence interval.
hand disinfection between patient contacts and have good examples of such strategies, as they shorten the
been shown to allow hand disinfection to occur more patient’s exposure to the endotracheal tube and risk
efficiently.33,34 Surveillance of ICU infections allows for aspiration of contaminated secretions.
staff to take appropriate infection control measures Maintain appropriate ICU staff levels (level II evidence).
for multidrug-resistant pathogens and aids in selecting Adequate nursing and respiratory therapy staffing may
empiric therapy in cases of suspected postoperative influence duration of stay of patients in ICUs and the
pneumonia. development of HAP/VAP, presumably due to main-
Avoid tracheal intubation/use noninvasive positive-pressure tenance of infection control standards.47,48 Lapses in
ventilation (level I evidence). The critical roles that the en- basic infection control measures (eg, handwashing,
dotracheal tube and ventilator circuit play in the patho- patient isolation for multidrug-resistant pathogens)
genesis of HAP/VAP emphasize the need for avoiding are more likely with increased workloads for registered
unnecessary intubations. Noninvasive positive-pressure nurses and increased reliance on less-trained health
ventilation (NIPPV) using a face mask can be an effective care personnel to deliver care.49–52 The duration of me-
ventilatory mode in appropriately selected patients likely chanical ventilation can also be reduced by appropri-
to benefit from this approach. The beneficial effects of ate staffing levels.45,52 Mandatory training of ICU staff
NIPPV on the development of HAP/VAP and on sur- aimed at HAP/VAP prevention is also important in
vival have been established in randomized trials involving preventing these nosocomial infections.53,54
patients with acute exacerbations of COPD or acute lung Use orotracheal/orogastric intubation (level II evidence). Oc-
injury with hypoxic respiratory failure and in immuno- clusion of one of the nares by a nasotracheal or nasogas-
suppressed patients with pulmonary infiltrates, fever, and tric tube has been identified as a risk factor promoting
respiratory failure.35–40 All attempts to avoid reintubation sinusitis.55 The presence of the foreign device prevents
should be considered, as this is an important risk factor clearance of the secretions from the sinuses, which can
for developing VAP.41 become infected. Infected secretions are a risk factor
Shorten duration of mechanical ventilation (level II for VAP from aspiration of the secretions into the lower
evidence). The duration of mechanical ventilation is an respiratory tract.56,57 The preferred route of tracheal and
important risk factor for the development of HAP/ gastric intubation is via the oropharynx to prevent the
VAP. The risk of HAP/VAP is not constant over the development of nosocomial sinusitis and HAP/VAP.
time of ventilation and, in a large cohort study, was Control subglottic secretions (level I evidence). Secretions
estimated to be 3% per day in the first week, 2% per tend to accumulate and pool above the endotracheal
day in the second week, and 1% per day in the third tube cuff in intubated patients.58 These pooled secretions
week and beyond.42 Strategies that reduce the duration can become contaminated and leak around the cuff into
of mechanical ventilation have the potential to reduce the lower respiratory tract, precipitating HAP/VAP. A
HAP/VAP rates significantly. Sedation protocols that specially designed endotracheal tube with a separate
focus on minimizing sedative administration43,44 and dorsal lumen that allows for continuous aspiration of
protocolized weaning of mechanical ventilation45,46 are the subglottic secretions has been shown to significantly
52 Hospital Physician September 2007 www.turner-white.comKollef : Prevention of Pneumonia : pp. 47–60, 64
Table 5. Strength of Evidence for Specific Interventions to Reduce the Risk for Postoperative Pulmonary Complications
Strength of
Risk Reduction Strategy Evidence Type of Complication Studied
Postoperative lung expansion modalities A Atelectasis, pneumonia, bronchitis, severe hypoxemia
Selective postoperative nasogastric decompression B Atelectasis, pneumonia, aspiration
Short-acting neuromuscular blockade B Atelectasis, pneumonia
Laparoscopic (versus open) operation C Spirometry, atelectasis, pneumonia, overall respiratory complications
Smoking cessation I Postoperative ventilator support
Intraoperative neuraxial blockade I Pneumonia, postoperative hypoxia, respiratory failure
Postoperative epidural analgesia I Atelectasis, pneumonia, respiratory failure
Immunonutrition I Overall infectious complications, pneumonia, respiratory failure
Routine total parenteral or enteral nutrition D Atelectasis, pneumonia, empyema, respiratory failure
Right-heart catheterization D Pneumonia
Adapted with permission from Lawrence VA, Cornell JE, Smetana GW. Strategies to reduce postoperative pulmonary complications after noncar-
diothoracic surgery: systematic review for the American College of Physicians. Ann Intern Med 2006;144:605.
A = good evidence that the strategy reduces complications and benefit outweighs harm; B = at least fair evidence that the strategy reduces
complications and benefit outweighs harm; C = at least fair evidence that the strategy may reduce complications, but the balance between benefit
and harm is too close to justify a general recommendation; D = at least fair evidence that the strategy does not reduce complications or harm
outweighs benefit; I = evidence of effectiveness of the strategy to reduce complications is conflicting, of poor quality, lacking, or insufficient, or the
balance between benefit and harm cannot be determined.
reduce the incidence of early-onset VAP in randomized opposed to routine circuit changes based on duration.
controlled trials, without a corresponding beneficial ef- This recommendation may reduce the incidence of
fect on mortality, ICU length of stay, or duration of me- VAP, minimize risk to health care workers from expo-
chanical ventilation.59–61 These specialized endotracheal sure to infected aerosols, and result in cost savings.
tubes cost approximately 20% to 25% more than stan- Heat-moisture exchanger (level I evidence). Use of heat-
dard endotracheal tubes. There is also level II evidence moisture exchangers can reduce condensate accumu-
for maintaining endotracheal tube cuff pressure at great- lation significantly, which could translate into lower
er than 20 cm H2O to prevent aspiration of subglottic VAP rates.68,69 One randomized trial found a lower
secretions around the cuff and into the lungs. incidence of late-onset VAP with humidification via a
Avoid unnecessary ventilator circuit changes and manipu- heat-moisture exchanger than with conventional heat-
lation/drain ventilator circuit condensate (level II evidence). water humidification.70 However, while heat-moisture
Studies have shown that the rate of bacterial contami- exchangers do decrease ventilator circuit colonization,
nation of inspiratory phase gas is not reduced by more they have not consistently resulted in significantly re-
frequent ventilator circuit changes.62 Several prospec- duced rates of VAP in clinical trials.69, 71–74
tive randomized trials have shown that VAP incidence Keep patients in semirecumbent position (level I evidence).
is not affected by the frequency of ventilator circuit The supine position is associated with aspiration of
changes or by more frequent tubing changes.63–67 upper airway secretions, which is a particular problem
However, vigilance is required by physicians, nurses, during enteral feeding.75 Studies using radiolabeled
and respiratory therapists to prevent flushing of the enteral feeds in patients undergoing mechanical venti-
ventilator circuit condensate into the lower respira- lation have demonstrated higher endotracheal counts,
tory tract with in-line medication administration and consistent with higher aspiration rates, when patients
patient repositioning. The contaminated condensate were kept supine compared with a semirecumbent
within ventilator circuits predisposes the patient to position (45°).75,76 An important randomized trial
VAP and also serves as a reservoir for the spread of demonstrated a three-fold reduction in the incidence
nosocomial pathogens to other patients in the ICU.62 of VAP and a trend toward a reduced hospital mortal-
Proper procedures must be followed when draining ity rate in patients treated in the semirecumbent posi-
the condensate from the tubing and disposing of the tion (45°) compared with patients treated completely
condensate. Current recommendations are to change supine (0°).77 However, more recent experiences have
ventilator circuits based on visual contamination of the demonstrated that optimal patient positioning is dif-
circuit with blood, emesis, or purulent secretions as ficult to maintain, and its influence on VAP prevention
www.turner-white.com Hospital Physician September 2007 53Kollef : Prevention of Pneumonia : pp. 47–60, 64
Table 6. Nonpharmacologic Strategies to Prevent Nosocomial Table 7. Pharmacologic Strategies to Prevent Nosocomial
Pneumonia Pneumonia
Evidence Evidence
Strategy Grade References Strategy Grade References
Handwashing/disinfection Level I 32–34 Use of sucralfate for GI prophylaxis Level I 96–99
Noninvasive positive pressure ventilation Level I 35–40 Parenteral antibiotic prophylaxis* Level I 102
Avoid tracheal reintubation Level I 41 Avoid unnecessary red blood cell Level 1 103–109
Weaning/sedation protocols Level II 43–46 transfusion
Adequate nursing/therapist staffing Level II 47–52 Blood glucose control with insulin Level I 110,111
Education initiatives Level II 53,54 Antibiotic cycling/rotation Level II 113–118
Avoid nasotracheal intubation Level II 55–57 Shorter courses of antibiotics Level I 120–122
Suctioning of subglottic secretions Level I 59–61 Vaccines U/D 124–127
Routine emptying of ventilator circuit Nebulized antimicrobials U/D 128
condensate Level II 62 Oral decontamination Level I 129–131
Avoid ventilator circuit changes Level II 63–67
GI = gastrointestinal; U/D = undetermined at this time.
Use of heat-moisture exchangers Level I 69–74
Maintain semierect position Level I 75–79 *Benefit for specific high-risk patients.
Use of enteral nutrition/small bowel feeds Level I 82,83
Antibacterial coating of endotracheal tube U/D 85–89
with a decrease in gastroesophageal regurgitation, an
Kinetic therapy beds* Level I 90,91
increase in protein and calorie delivery, and a shorter
Chest physiotherapy† U/D 92,93
time to reaching feeding goals.82 In addition, when the
U/D = undetermined at this point. results of 7 randomized trials were aggregated statistical-
*Benefit limited to specific patient types.
ly, patients who received small bowel feeds as opposed
to gastric feeds had fewer episodes of pneumonia.
†Incentive spirometry/deep breathing maneuvers are more resource
However, there was no difference in mortality between
effective than chest physiotherapy.
the groups. The optimal time to initiate enteral nutri-
tion is not clear. Although early nutritional support
is questionable.78,79 Nevertheless, intubated patients intuitively makes sense, a strategy of early goal-directed
should be kept in the semierect position at all times if feeding (day 1 of intubation) compared with low-level
possible, particularly during enteral feeding. early enteral feeding followed by goal-directed feeds
Enteral nutrition is preferable to parental nutrition (level I (day 5 of intubation) showed higher VAP rates in the
evidence). The optimal approach for providing nutri- early goal-directed group.83 Delaying the administration
tion to mechanically ventilated patients and the tim- of goal-directed enteral feeds in selected patients with
ing of initiation of nutritional support is complicated. En- high aspiration risks may prevent HAP/VAP.
teral nutrition is considered a risk factor for VAP, espe- Biofilm prevention technology (level of evidence un
cially in the presence of large gastric volumes and the in- determined). Biofilms form on surfaces (eg, endotracheal
creased risk of aspiration of gastric contents.16,20,80 The al- tube lumen) and consist of mucus, water channels, and
ternative of parenteral nutrition is associated with higher slime-enclosed colonies of bacteria that settle in the
costs, complications from line insertion, intravascular biofilm and can intermittently become detached from
device-associated infections, and loss of intestinal villous it.19,84 Pseudomonas species are particularly adept at form-
structure. Atrophy of intestinal villi may be a risk factor ing biofilms, analogous to their propensity to infect
for intestinal microbial translocation. Use of enteral nutri- patients with abnormal airways (eg, patients with cystic
tion should precipitate measures to avoid gastric overdis- fibrosis). The recognition of the occurrence of biofilms
tention.81 These measures include reducing narcotic and on endotracheal tubes and their pathogenic potential
anticholinergic use, monitoring gastric residual volumes has stimulated interest in approaches to limit biofilm
prior to intermittent gastric enteral feedings, using proki- formation. These include the use of surface coatings
netic agents, and using smaller bore feeding tubes.16,20 that impair bacterial adherence, oxygen-plasma pro-
The available evidence supports small bowel or post- cessing of the polyvinyl chloride, and the administra-
pyloric feeding in critically ill patients. An analysis of tion of nebulized antibiotics.85–89 Unfortunately, none of
10 studies in critically ill patients found that, compared these approaches has yet undergone rigorous clinical
with gastric feeding, small bowel feeding was associated investigation, and it is not clear whether such technolo-
54 Hospital Physician September 2007 www.turner-white.comKollef : Prevention of Pneumonia : pp. 47–60, 64
gies will influence the adherence of airway secretions gastrointestinal bleeding occurred 4% more frequently
on the surface of the endotracheal tube. in the sucralfate group.97 A reasonable strategy is to as-
Kinetic therapy beds (level I evidence in neurosurgical/ sess the risks and benefits of stress ulcer prophylaxis on
surgical patients only). Critically ill patients tend to devel- an individual basis, taking into account each patient’s
op atelectasis and are unable to clear their secretions specific risks for VAP and gastrointestinal bleeding.
as a result of their immobility. Kinetic therapy beds, Avoid routine use of prophylactic antibiotics except in selected
which continuously rotate patients, have reduced the patients (level I evidence). Prolonged use of prophylactic
risk of pneumonia in surgical and neurosurgical pa- antibiotics in trauma patients was associated with the de-
tient populations in randomized trials; however, these layed onset of HAP/VAP but an increased incidence of
results could not be duplicated in medical patients.90,91 pneumonia caused by antibiotic-resistant gram-negative
Barriers to the use of kinetic therapy beds include cost, bacteria and an increased overall incidence of nosoco-
disconnection of intravenous catheters and other in- mial infections.100 A multivariate analysis of VAP patients
dwelling devices, and concerns about pressure ulcers. found prior administration of antibiotics to have an
However, this modality can be considered in neurosur- adjusted odds ratio of 3.1 (95% confidence interval,
gical or surgical patients.90 1.4–6.9) for the development of late-onset VAP.101 The
Chest physiotherapy (level of evidence undetermined). The greatest harm of prolonged prophylactic antibiotics is the
theoretical benefits of chest physiotherapy techniques potential for ensuing infection with antibiotic-resistant
(eg, postural drainage, manual lung hyperinflation) in- pathogens, which can be transmitted to other patients.
clude more rapid resolution of atelectasis and enhanced However, prophylactic parenteral antibiotics may play a
airway clearance. A stratified, randomized trial in patients role in the prevention of HAP/VAP among specific high-
after abdominal surgery found incentive spirometry and risk populations, including patients with head trauma or
deep breathing exercises to be more resource effective coma. In a randomized trial, cefuroxime administration
than chest physiotherapy.92 A small, prospective nonran- for 24 hours at the time of intubation in patients with
domized trial showed a reduced incidence of VAP in pa- closed head injury reduced the incidence of early-onset
tients receiving chest physiotherapy.93 Barriers to the use VAP.102 Therefore, prophylactic antibiotics should be em-
of chest physiotherapy include limited universal access, ployed in appropriate high-risk patients (trauma, severe
optimal use of physical therapist time, and associated head injury, coma, high-risk surgical procedure), gener-
risks (eg, arterial hypoxemia). Larger randomized clini- ally for less than 24 hours following intubation, surgery,
cal trials are needed to evaluate this intervention. or the initial trauma.
Pharmacologic interventions. The following inter- Follow restricted (conservative) blood transfusion policy (level I
ventions should be tailored to the patient’s specific risk evidence). The transfusion of packed red blood cells has
factors. been associated with serious nosocomial infections,
Avoid unnecessary use of stress ulcer prophylaxis (level I including VAP.30,103–106 This is thought to result from
evidence). Histamine2-receptor (H2-receptor) blockers the immunosuppressive effects of donor leukocyte-
and antacids are appropriate measures for stress ulcer containing packed red blood cell units. In 1 study, trans-
prophylaxis but also are known risk factors for the fusion of packed red blood cells was found to be an
development of VAP.94 This risk presumably results independent risk factor for the development of VAP.107
from decreased intragastric acidity creating a favorable A prospective, randomized trial using leukocyte-depleted
environment for colonization of the stomach by patho- red blood cell transfusions in a group of patients under-
gens and via the increased intragastric volumes, which going colorectal surgery resulted in a reduced incidence
increases the risk for aspiration.95 Sucralfate does not of pneumonia.108 These data suggest that the unnecessary
significantly increase gastric volume or decrease intra- transfusion of packed red blood cells should be avoided
gastric acidity. Numerous randomized trials in differ- to reduce the risk of nosocomial infections including
ent patient populations and using different dosages HAP/VAP and that conservative “triggers” to transfusion
have yielded conflicting results with respect to VAP in ICU patients in the absence of active bleeding or car-
risk.96–99 In a large randomized trial, sucralfate use was diac disease should be followed.109
associated with lower rates of late-onset VAP compared Optimize glycemic control (level I evidence). Intensive insu-
with H2-receptor blocker and antacid use.96 The Ca- lin therapy to maintain blood glucose levels between 80
nadian Critical Care Trials Group performed a large, and 110 mg/dL in randomized surgical ICU patients
double-blind, randomized trial comparing ranitidine resulted in reduced mortality, reduced bloodstream
with sucralfate and found a trend toward lower VAP infections, less antibiotic use, shorter duration of me-
rates with sucralfate use; however, clinically significant chanical ventilation, and shorter ICU stays.110 A similar
www.turner-white.com Hospital Physician September 2007 55Kollef : Prevention of Pneumonia : pp. 47–60, 64
study in critically ill medical patients failed to demon- sequent hospitalization for pneumonia, supporting the
strate a mortality benefit and found more episodes of hy- benefit of this intervention.126 Vaccines for the preven-
poglycemia in the intensive insulin therapy group.111 In- tion of antibiotic-resistant bacterial infections are not
tensive glycemic control has not been studied in patients currently available for use in the ICU setting.
with VAP, but avoidance of hyperglycemia and its adverse Nebulized antibiotics (level of evidence undetermined).
effects on neutrophil function is recommended. A study by Palmer et al128 revealed that in ventilator-
Antibiotic class rotation (level II evidence). Predominant dependent patients who were colonized with gram-
use of a single drug class to treat gram-negative bacte- negative organisms and who had tracheostomy tubes
rial infections has been associated with the emergence in place, nebulized aminoglycosides resulted in a sig-
of antibiotic-resistant infections, including HAP/VAP.112 nificant reduction in the volume of secretions and,
The practice of a scheduled antibiotic class switch that in some patients, eradication of the gram-negative
simultaneously provides adequate empiric antimicro- colonizers. This concept has not yet been studied in a
bial coverage and minimizes antimicrobial resistance is randomized manner as a strategy to prevent VAP.
an appealing strategy based on the theory that cycling Oropharyngeal decontamination (level I evidence). The
of antibiotic classes will reduce the selective pressure use of chlorhexidine solution for oropharyngeal de-
on bacteria to become resistant to a single class.113,114 contamination has also been evaluated in patients un-
This strategy has been associated with reduced oc- dergoing heart surgery.129 In these randomized clinical
currence of VAP when increasing resistance to the trials, patients receiving chlorhexidine oral rinses had
baseline antibiotic class was recognized as the stimulus significantly lower overall rates of HAP/VAP compared
for the class switch.113 However, this strategy has had with patients receiving placebo. In 1 of these studies,
inconsistent effects on antimicrobial resistance patterns the mortality rate and use of intravenous drugs were
and the development of nosocomial infections.115–118 also decreased among patients receiving chlorhexidine
A policy of antibiotic rotation can be considered only rinses without changing bacterial resistance patterns.129
in conjunction with the application of other strate- The results of 2 large multicenter trials of chlorhexi-
gies aimed at preventing the emergence of antibiotic- dine have been mixed.130,131 However, given the low
resistant infections (ie, short-course antibiotic therapy cost and lack of significant resistance, use of chlorhexi-
and adequate infection control measures). dine for oropharyngeal decontamination should be
Use short-course antibiotic therapy (level I evidence). Pro- employed in high-risk patients.
longed administration of antibiotics to ICU patients
has been shown to be an important risk factor for the Overcoming Barriers to Implementation of Preventive
emergence of colonization and infection with antibiotic- Strategies
resistant bacteria.15 Attempts have been made to shorten The prevention of hospital-associated infections is an
the duration of antibiotic treatment in order to reduce important management objective for all hospitals, but
subsequent hospital-associated infections caused by achieving effective implementation of preventive strate-
antibiotic-resistant bacteria.26,119 Several clinical trials gies is difficult. A comparison of French and Canadian
have found that 7 to 8 days of antibiotic treatment is ac- ICUs regarding the use of 7 strategies to control secre-
ceptable for most nonbacteremic patients with VAP.26,120– tions and to care for ventilator circuits revealed low over-
122
Several recently published guidelines for the antibi- all compliance with specific VAP prevention guidelines
otic management of nosocomial pneumonia and severe (64% in French ICUs versus 30% in Canadian ICUs).132
sepsis recommend the discontinuation of empiric anti- Two European surveys of physicians and nurses found
biotic therapy after 48 to 72 hours if cultures are nega- that 37% of ICU physicians and 22% of nurses were not
tive or the signs of infection have resolved.29,123 following published VAP prevention guidelines.133,134 The
Vaccines (level of evidence undetermined). Vaccination reasons for nonadherence were disagreement with inter-
programs in adults and children have been success- pretation of trial data, lack of resources, fear of potential
ful in reducing the incidence of pneumonia caused adverse events, and costs associated with the implementa-
by specific pathogens, including Hemophilus influen- tion of specific interventions. The use of standardized
zae, Streptococcus pneumoniae, and influenza virus.124–127 practices for HAP/VAP prevention along with focused
These pathogens are major causes of health care– educational modules for staff have been shown to over-
associated pulmonary infections and can predispose to come these barriers and to reduce infection rates.53,54 HP
the development of HAP/VAP. At least 1 study showed
that the use of a vaccine directed against a respira- Corresponding author: Marin H. Kollef, MD, Campus Box 8052, 660
tory pathogen in a high-risk population reduced sub- South Euclid Avenue, St. Louis, MO 63110; mkollef@im.wustl.edu.
56 Hospital Physician September 2007 www.turner-white.comKollef : Prevention of Pneumonia : pp. 47–60, 64
REFERENCES associated pneumonia caused by potentially drug-resistant
1. Tablan OC, Anderson LJ, Besser R, et al. Guidelines bacteria. Am J Respir Crit Care Med 1998;157:531–9.
for preventing health-care–associated pneumonia, 2003: 16. Kollef MH. Epidemiology and risk factors for nosocomial
recommendations of CDC and the Healthcare Infection pneumonia. Emphasis on prevention. Clin Chest Med 1999;
Control Practices Advisory Committee. MMWR Recomm 20:653–70.
Rep 2004;53:1–36. 17. Johanson WG Jr, Pierce AK, Sanford JP, Thomas GD. Nos-
2. Chastre J, Fagon JY. Ventilator-associated pneumonia. Am ocomial respiratory infections with gram-negative bacilli.
J Respir Crit Care Med 2002;165:867–903. The significance of colonization of the respiratory tract.
3. Rello J, Ollendorf DA, Oster G, et al. Epidemiology and Ann Intern Med 1972;77:701–6.
outcomes of ventilator-associated pneumonia in a large 18. Niederman MS. Bacterial adherence as a mechanism of
US database. VAP Outcomes Scientific Advisory Group. airway colonization. Eur J Clin Microbiol Infect Dis 1989;
Chest 2002;122:2115–21. 8:15–20.
4. Warren DK, Shukla SJ, Olsen MA, et al. Outcome and at- 19. Prince AS. Biofilms, antimicrobial resistance, and airway
tributable cost of ventilator-associated pneumonia among infection. N Engl J Med 2002;347:1110–1.
intensive care unit patients in a suburban medical center. 20. Kollef MH. The prevention of ventilator-associated pneu-
Crit Care Med 2003;31:1312–17. monia. N Engl J Med 1999;340:627–34.
5. Heyland DK, Cook DJ, Griffith L, et al. The attributable 21. Cook DJ, Kollef MH. Risk Factors for ICU-acquired pneu-
morbidity and mortality of ventilator-associated pneumo- monia. JAMA 1998;279:1605–6.
nia in the critically ill patient. The Canadian Critical Tri- 22. Meduri, GU. Diagnosis and differential diagnosis of
als Group. Am J Respir Crit Care Med 1999;159(4 Pt 1): ventilator-associated pneumonia. Clin Chest Med 1995;
1249–56. 16:61–93.
6. Fagon JY, Chastre J, Hance AJ, et al. Nosocomial pneu- 23. Andrews CP, Coalson JJ, Smith JD, Johanson WG Jr. Diag-
monia in ventilated patients: a cohort study evaluating nosis of nosocomial bacterial pneumonia in acute, diffuse
attributable mortality and hospital stay. Am J Med 1993;94: lung injury. Chest 1981;80:254–8.
281–8. 24. Fagon JY, Chastre J, Hance AJ, et al. Evaluation of clinical
7. Fagon JY, Chastre J, Vuagnat A, et al. Nosocomial pneumo- judgment in the identification and treatment of nosoco-
nia and mortality among patients in intensive care units. mial pneumonia in ventilated patients. Chest 1993;103:
JAMA 1996;275:866–9. 547–53.
8. Markowicz P, Wolff M, Djedaini K, et al. Multicenter pro- 25. Fabregas N, Ewig S, Torres A, et al. Clinical diagnosis of
spective study of ventilator-associated pneumonia during ventilator associated pneumonia revisited: comparative
acute respiratory distress syndrome. Incidence, prognosis validation using immediate post-mortem lung biopsies.
and risk factors. ARDS Study Group. Am J Respir Crit Thorax 1999;54:867–73.
Care Med 2000;161:1942–8. 26. Ibrahim EH, Ward S, Sherman G, et al. Experience with a
9. George DL, Falk PS, Wunderink RG, et al. Epidemiol- clinical guideline for the treatment of ventilator-associated
ogy of ventilator-acquired pneumonia based on protected pneumonia. Crit Care Med 2001;29:1109–15.
bronchoscopic sampling. Am J Respir Crit Care Med 1998; 27. Shorr AF, Sherner JH, Jackson WL, Kollef MH. Invasive
158:1839–47. approaches to the diagnosis of ventilator-associated pneu-
10. National Nosocomial Infections Surveillance (NNIS) Sys- monia: a meta-analysis. Crit Care Med 2005;33:46–53.
tem report, data summary from January 1990–May 1999, 28. Kollef MH. Inadequate antimicrobial treatment: an im-
issued June 1999. Am J Infect Control 1999;27:520–32. portant determinant of outcome for hospitalized patients.
11. Richards MJ, Edwards JR, Culver DH, Gaynes RP. Noso- Clin Infect Dis 2000;31 Suppl 4:S131–8.
comial infections in medical intensive care units in the 29. Guidelines for the management of adults with hospital-
United States. National Nosocomial Infections Surveil- acquired, ventilator-associated, and healthcare-associated
lance System. Crit Care Med 1999;27:887–92. pneumonia. American Thoracic Society; Infectious Dis-
12. Rello J, Torres A, Ricart M, et al. Ventilator-associated eases Society of America. Am J Respir Crit Care Med 2005;
pneumonia by Staphylococcus aureus. Comparison of methi- 171:388–416.
cillin-resistant and methicillin-sensitive episodes. Am J 30. Arozullah AM, Khuri SF, Henderson WG, et al. Develop-
Respir Crit Care Med 1994;150(6 Pt 1):1545–9. ment and validation of a multifactorial risk index for pre-
13. Marik PE, Careau P. The role of anaerobes in patients with dicting postoperative pneumonia after major noncardiac
ventilator-associated pneumonia and aspiration pneumo- surgery. Ann Intern Med 2001;135:847–57.
nia: a prospective study. Chest 1999;115:178–83. 31. Lawrence VA, Cornell JE, Smetana GW. Strategies to
14. el-Ebiary M, Torres A, Fabregas N, et al. Significance of reduce postoperative pulmonary complications after non-
the isolation of Candida species from respiratory samples cardiothoracic surgery: systematic review for the American
in critically ill, non-neutropenic patients. An immediate College of Physicians. American College of Physicians.
postmortem histologic study. Am J Respir Crit Care Med Ann Intern Med 2006;144:596–608.
1997;156(2 Pt 1):583–90. 32. Boyce JM, Pittet D. Guideline for Hand Hygiene in Health-
15. Trouillet JL, Chastre J, Vuagnat A, et al. Ventilator- Care Settings. Recommendations of the Healthcare
www.turner-white.com Hospital Physician September 2007 57Kollef : Prevention of Pneumonia : pp. 47–60, 64
Infection Control Practices Advisory Committee and the tor weaning protocols driven by nonphysician health-care
HIPAC/SHEA/APIC/IDSA Hand Hygiene Task Force. professionals: evidence-based clinical practice guidelines.
Healthcare Infection Control Practices Advisory Commit- Chest 2001;120(6 Suppl):454S–63S.
tee; HICPAC/SHEA/APIC/IDSA Hand Hygiene Task 47. Needleman J, Buerhaus P, Mattke S, et al. Nurse-staffing
Force. Am J Infect Control 2002;30:S1–46. levels and the quality of care in hospitals. N Engl J Med
33. Girou E, Loyeau S, Legrand P, et al. Efficacy of handrub- 2002;346:1715–22.
bing with alcohol based solution versus standard hand- 48. Cho SH, Ketefian S, Barkauskas VH, Smith DG. The ef-
washing with antiseptic soap: randomised clinical trial. fects of nurse staffing on adverse events, morbidity, mortal-
BMJ 2002;325:362. ity and medical costs. Nurs Res 2003;52:71–9.
34. Pittet D, Hugonnet S, Harbarth S, et al. Effectiveness of 49. Archibald LK, Manning ML, Bell LM, et al. Patient density,
a hospital-wide programme to improve compliance with nurse-to-patient ratio and nosocomial infection risk in a pe-
hand hygiene. Infection Control Programme [published diatric cardiac intensive care unit. Pediatr Infect Dis J 1997;
erratum appears in Lancet 2000;356:2196]. Lancet 2000; 16:1045–8.
356:1307–12. 50. Fridkin SK, Pear SM, Williamson TH, et al. The role of
35. Antonelli M, Conti G, Rocco M, et al. A comparison of understaffing in central venous catheter-associated blood-
noninvasive positive-pressure ventilation and conventional stream infections. Infect Control Hosp Epidemiol 1996;
mechanical ventilation in patients with acute respiratory 17:150–8.
failure. N Engl J Med 1998;339:429–35. 51. Pittet D, Mourouga P, Perneger TV. Compliance with hand-
36. Hilbert G, Gruson D, Vargas F, et al. Noninvasive ventila- washing in a teaching hospital. Ann Intern Med 1999;130:
tion in immunosuppressed patients with pulmonary infil- 126–30.
trates, fever and acute respiratory failure. N Engl J Med 52. Thorens JB, Kaelin RM, Jolliet P, Chevrolet JC. Influence
2001;344:481–7. of the quality of nursing on the duration of weaning from
37. Carlucci A, Richard JC, Wysocki M, et al. Noninvasive mechanical ventilation in patients with chronic obstructive
versus conventional mechanical ventilation. An epidemio- pulmonary disease. Crit Care Med 1995;23:1807–15.
logic survey. Am J Respir Crit Care Med 2001;163:874–80. 53. Zack JE, Garrison T, Trovillion E, et al. Effect of an edu-
38. Nava S, Ambrosino N, Clini E, et al. Noninvasive mechani- cation program aimed at reducing the occurrence of
cal ventilation in the weaning of patients with respira- ventilator-associated pneumonia. Crit Care Med 2002;30:
tory failure due to chronic obstructive pulmonary disease. 2407–12.
A randomized, controlled trial. Ann Intern Med 1998; 54. Babcock HM, Zack JE, Garrison T, et al. An educational
128:721–8. intervention to reduce ventilator-associated pneumonia in
39. Girou E, Schortgen F, Delclaux C, et al. Association of an integrated health system: a comparison of effects. Chest
noninvasive ventilation with nosocomial infections and 2004;125:2224–31.
survival in critically ill patients. JAMA 2000;284:2361–7. 55. Rouby JJ, Laurent P, Gosnach M, et al. Risk factors and
40. Nourdine K, Combes P, Carton MJ, et al. Does noninva- clinical relevance of nosocomial maxillary sinusitis in the
sive ventilation reduce the ICU nosocomial infection risk? critically ill. Am J Respir Crit Care Med 1994;150:776–83.
A prospective clinical survey. Intensive Care Med 1999; 56. Holzapfel L, Chastang C, Demingeon G, et al. A random-
25:567–73. ized study assessing the systematic search for maxillary
41. Torres A, Gatell JM, Aznar E, et al. Re-intubation increas- sinusitis in nasotracheally mechanically ventilated patients.
es the risk of nosocomial pneumonia in patients need- Influence of nosocomial maxillary sinusitis on the occur-
ing mechanical ventilation. Am J Respir Crit Care Med rence of ventilator-associated pneumonia. Am J Respir
1995;152:137–41. Crit Care Med 1999;159:695–701.
42. Cook DJ, Walter SD, Cook RJ, et al. Incidence of and risk 57. Bert F, Lambert-Zechovsky N. Sinusitis in mechanically
factors for ventilator-associated pneumonia in critically ill ventilated patients and its role in the pathogenesis of nos-
patients. Ann Intern Med 1998;129:433–40. ocomial pneumonia. Eur J Clin Microbiol Infect Dis 1996;
43. Brook AD, Ahrens TS, Schaiff R, et al. Effect of a nursing- 15:533–44.
implemented sedation protocol on the duration of me- 58. Greene R, Thompson S, Jantsch HS, et al. Detection of
chanical ventilation. Crit Care Med 1999;27:2609–15. pooled secretions above endotracheal-tube cuffs: value of
44. Kress JP, Pohlman AS, O’Connor MF, Hall JB. Daily in- plain radiographs in sheep cadavers and patients. AJR Am
terruption of sedative infusions in critically ill patients J Roentgenol 1994;163:1333–7.
undergoing mechanical ventilation. N Engl J Med 2000; 59. Valles J, Artigas A, Rello J, et al. Continuous aspiration of
342:1471–7. subglottic secretions in preventing ventilator-associated
45. Marelich GP, Murin S, Battistella F, et al. Protocol weaning pneumonia. Ann Intern Med 1995;122:179–86.
of mechanical ventilation in medical and surgical patients 60. Kollef MH, Skubas NJ, Sundt TM. A randomized clinical
by respiratory care practitioners and nurses: effect on trial of continuous aspiration of subglottic secretions in
weaning time and incidence of ventilator-associated pneu- cardiac surgery patients. Chest 1999;116:1339–46.
monia. Chest 2000;118:459–67. 61. Smulders K, van der Hoeven H, Weers-Pothoff I, et al. A ran-
46. Ely EW, Meade MO, Haponik EF, et al. Mechanical ventila- domized clinical trial of intermittent subglottic secretion
58 Hospital Physician September 2007 www.turner-white.comYou can also read