Would It Matter to Expose Elderly Patients Who Took Digoxin to Chinese Medications?
←
→
Page content transcription
If your browser does not render page correctly, please read the page content below
VALUE IN HEALTH REGIONAL ISSUES 3C (2014) 211–221
Available online at www.sciencedirect.com
journal homepage: www.elsevier.com/locate/vhri
Would It Matter to Expose Elderly Patients Who Took Digoxin to
Chinese Medications?
Hsiang-Wen Lin, PhD1,2,*, Hsin-Hui Tsai, PhD2,3, I-Wen Yu2, Arun Kumar, PhD student1,
Man-Pin Wu, BBA1
1
School of Pharmacy and Graduate Institute, College of Pharmacy, China Medical University, Taichung, Taiwan, ROC; 2Department of
Pharmacy, China Medical University Hospital, Taichung, Taiwan, ROC; 3Department of Cosmetic Science, Providence University,
Taichung, Taiwan, ROC
AB STR A CT
Objectives: Elderly patients seem vulnerable to digoxin toxicity concomitant CM use among digoxin elderly users were 0.43% and
because of their diminished organ functions and tendency to encoun- 0.22%, respectively. Although the other factors were not statistically
ter drug interactions. The aim of this research was to explore the significantly associated with incident CM-digoxin use, patients with
extent of the concurrent use of digoxin with Chinese medications heart diseases and with benign prostate hypertrophy had an increased
(CMs), its contributing factors, and the relevant consequences. Meth- likelihood of incident CM-digoxin use of 115% and 102%, respectively.
ods: A retrospective population-based cohort study was conducted Almost all the concerned clinical and economic outcomes were not
using Longitudinal Health Insurance databases in Taiwan. Those statistically significantly different between incident exposure or not,
elderly patients being prescribed with digoxin in outpatient settings except for the use of potassium-sparing and nonsteroidal anti-
in 2006 were evaluated for the incidence, prevalence, and duration of inflammatory drugs. Conclusions: There was a relatively low incidence
concurrent use with concentrated CMs in 2006. After 1:1 random of digoxin-CM use among the elderly in Taiwan. Although no signifi-
matching to select the corresponding digoxin-only elderly users, cant effects on clinical and economic outcomes occurred, it is neces-
univariate and multivariate logistic regression analyses were per- sary to monitor potential side effects of digoxin more aggressively for
formed to explore factors associated with concomitant incident those vulnerable elderly using digoxin with CMs, especially for those
who tended to expose to incident digoxin-CM use elderly patients.
digoxin-CM use and incident digoxin-specific CM use. The relevant
Keywords: Chinese medications, concurrent use, digoxin, drug
clinical and economic outcomes for a 3-month follow-up period from
interactions, elderly.
the initial exposure of incident digoxin-CM use were compared.
Results: Of 185,076 elderly, 6,374 were prescribed with digoxin and Copyright & 2014, International Society for Pharmacoeconomics and
789 were CM-digoxin users in 2006. The prevalence and incidence of Outcomes Research (ISPOR). Published by Elsevier Inc.
frail elderly, the use of herbal medicine with regular use of Western
Introduction
medications, especially those with narrow therapeutic indexes,
Elderly people, especially those with chronic conditions, are more might pose potential safety concerns to individuals that could be
prone to experiencing drug interactions and adverse drug reactions mitigated by health professionals to some extent.
because they often take many medications together and have Digoxin, one of the positive inotropic agents, is used for many
diminished body functions, along with multiple chronic illnesses conditions, including heart failure (HF) and atrial fibrillation, both
[1,2]. A systematic review reported that 1% to 61% of the patients, of which are very common chronic diseases among elderly
including the elderly, with cardiovascular diseases used comple- patients [8]. Digoxin has a narrow therapeutic index and tends to
mentary and alternative medicine (CAM), whereas 2% to 46% of have drug interactions with other Western and Chinese medica-
them used herbal medicine [3]. In particular, 53% to 60% of CAM tions (CMs) due to pharmacokinetic mechanisms (e.g., altered renal
users, in which older adults accounted for the majority, tended not P-glycoprotein–mediated transport), pharmacodynamic mecha-
to disclose their use to primary health care providers [4,5]. Less nisms (e.g., result in hypopotassemia), and its life-threatening
than half of nurses, physicians, and pharmacists documented the toxicities [9]. The dose of digoxin more than 0.125 mg per day is
patients’ use of natural health products in their medical records [6]. considered potentially inappropriate for older adults based upon
Therefore, the World Health Organization has recommended the the update, Beers Criteria [10]. In addition, it might be necessary to
supervision of Western medicine practices together with tradi- concern the increasing digoxin toxicity due to the occurrences of
tional, complementary, and alternative medicines [7]. For those potential interactions between digoxin and clarithromycin [11],
Conflict of interest: The authors have indicated that they have no conflicts of interest with regard to the content of this article.
* Address correspondence to: Hsiang-Wen Lin, School of Pharmacy and Graduate Institute, China Medical University, No. 91 Hsueh-Shih
Road, Taichung, Taiwan 40402, ROC.
E-mail: hsiangwl@mail.cmu.edu.tw.
2212-1099$36.00 – see front matter Copyright & 2014, International Society for Pharmacoeconomics and Outcomes Research (ISPOR).
Published by Elsevier Inc.
http://dx.doi.org/10.1016/j.vhri.2014.04.002212 VALUE IN HEALTH REGIONAL ISSUES 3C (2014) 211–221
and with some herbal medicines (e.g., chan su, lu-shen-wan, dan More specifically, we used the Longitudinal Health Insurance
shen, asian ginseng, siberian ginseng, and shan zha) [12–14]. Database 2000 and 2005 (LHID 2000 and LHID 2005) for the analyses.
Herbal medications such as digitalis, however, have been used This is one of the formal population databases containing infor-
to treat ailments since ancient times [15]. People believe that herbal mation about prescription data of Western medications and con-
medications do not cause any problems and are safe to use, even if centrated CMs under the national insurance program. This study
the active ingredients of many herbs may interact with synthetic was exempt from the institutional review board because the NHIRD
medications and result in the occurrence of adverse drug reactions database contains de-identified person data and de-identified
[16–18]. For instance, elderly patients with HF seem liable to use health care settings. The NHIRD is publicly available only through
herbal medicines to receive their benefits [19]. Although the con- the proper application process for researchers.
current use of herbal medications may show synergistic, agonistic,
or antagonistic effects on Western medications, those aforemen-
tioned studies showed the existence of significant interactions Study Population
between digoxin and CMs on pharmacokinetic and pharmacody- We focused on elderly digoxin users because elderly patients are
namic aspects. To date, information on the actual exposure of more likely to be given medication inappropriately, encounter
digoxin with CMs among older adults and its contributing factors is adverse drug reactions (i.e., electrolyte imbalance, gastrointesti-
limited, as is information about its good or bad effects on patients. nal upset), and/or experience drug interactions due to the use of
For the past decade, the use of CAM, including Traditional digoxin and other medications together [2,10]. The prevalence
Chinese Medicine (TCM), has been rising globally [20,21], as well and incidence of the concurrent use of digoxin with CMs in 2005
as in Taiwan [22]. An Australian study conducted in 2007 showed for all ages of the NHI population in Taiwan were 10.7% and 5.4%,
that Chinese medicine usage accounted for 20% of all CAM use respectively [14]. Thus, we extended these findings to conduct
among older Australian women [23]. There were 10%, 28%, and this study and further identified those elderly NHI beneficiaries
63% of National Health Insurance (NHI) beneficiaries who had who survived and were prescribed digoxin in 2006. By analyzing
reported using TCM services in Taiwan in periods of 1 month, 1 outpatient records, those elderly who were prescribed CMs with
year, and 6 years, respectively [24]. In particular, concentrated digoxin for at least 1 day were identified as digoxin-CM elderly
CMs, which are the extracts of single CMs, and combined CM users, whereas the incident digoxin-CM elderly users were those
remedy products are the most commonly used TCM therapies in digoxin-CM elderly individuals who had no prescription records
Taiwan. The use of concentrated CM has increased [25]. These about previous CM use for the 6-month period before the date of
concentrated CMs are those medications derived from the TCM first CM prescription use in 2006.
theories so that the active chemical ingredients of concentrated Furthermore, we evaluated the occurrence and consequences
CM products are the same as the crude CM products, except the of interactions between digoxin and other prespecified CM
starches as the excipients in the concentrated CM products. products, that is, da huang, hawthorn, dan shen, licorice, oyster
Almost all concentrated CMs have been covered by Taiwan’s shell, siberian ginseng, senna, and aloe vera, which were
NHI since the NHI program’s inception in 1995. The quality of obtained from one of the research team’s systematic review
concentrated CMs is important, and its processing should comply study, for which partial results were published recently [28].
with the current good manufacture practice to control the The incidence of digoxin-specific CM interactions among the
authorization and licensing for manufacture and sale of concen- incident digoxin-CM elderly users was estimated. Furthermore,
trated CM products in Taiwan [26]. Detailed registered informa- we used Greedy algorithms to match and select one counterpart
tion about the individual CM component, quantity, TCM of digoxin-only users for each incident digoxin-CM elderly user
indication, TCM efficacy, and manufacturing of the concentrated and incident digoxin-specific CM elderly user on the basis of
CMs is provided transparently on the Web site of the Department corresponding propensity scores derived from the combination of
of Chinese Medicine and Pharmacy, Ministry of Health and the following variables to reduce the selection bias: the month of
Welfare, using traditional Chinese language [27]. Regarding the the index date, the same duration of digoxin use, age, with or
use of appropriate medication and its corresponding clinical without catastrophic illness certification, outpatient clinic visits
effects among vulnerable older adults, especially for those who per year, number of prescribed distinct medications, and total
took Western medications with a narrow therapeutic index, the medical expenditure. Thus, the index date of the selected
aim of this study was to explore the extent of the concurrent use digoxin-only elderly user was the same as that of the corre-
of digoxin with concentrated CMs, its contributing factors, and sponding incident digoxin-CM elderly user.
the relevant consequences for the elderly.
Potential Factors Associated with Incident Digoxin-CM Use
and Occurrence of Interactions among the Elderly
Methods
Those listed factors relevant to incident concurrent use of high-
risk Western medications and CMs or CAM in previous studies
Study Design [4,14,25,29] were considered potential factors that were associ-
This population-based retrospective cohort study was conducted ated with incident digoxin-CM use and incident digoxin-specific
to 1) examine the prevalence and incidence of concurrent use CM interactions. In particular, those patients’ information about
and interactions of digoxin with concentrated CMs among elderly their comorbidities (based on the International Classification of
NHI beneficiaries, and describe their use patterns; 2) explore the Diseases, Ninth Revision, Clinical Modification [ICD-9-CM] codes) and
contributing factors associated with incident digoxin-CM use and health service utilizations (i.e., outpatient clinic visits, number of
incident digoxin-specific CM interactions; and 3) examine the prescribed distinct medications, ever hospitalization, total med-
relevant effects of incident digoxin-specific CM interactions. ical expenditure) was ascertained during the 6-month period
before the dates of first CM prescription, in terms of index dates.
The number of prescribed distinct medications infers all items
Data Sources of distinct medications prescribed by either Western medicine
This study used the 2 million sampling claimed data, National physicians and/or Chinese medicine physicians during the 6-
Health Research Insurance Database (NHIRD), which represents the month period before the index dates reported in the NHIRD
entire insured Taiwanese population (i.e., 23 million individuals). records.VALUE IN HEALTH REGIONAL ISSUES 3C (2014) 211–221 213
Effects Associated with Incident Occurrence of Digoxin-Specific than did digoxin-only elderly users. The other potential factors
CM Interactions among the Elderly were the same between these two groups of elderly patients, in
terms of not reaching statistical significance.
After a 3-month follow-up period from the initial exposure of
The univariate and multivariate logistic regression analyses
digoxin-specific CM use and that of corresponding digoxin-only
also indicated that crude ORs and adjusted ORs for those patients
use, the elderly patients’ relevant outcomes were further eval-
with diagnoses of heart diseases and BPH were statistically
uated for their health service utilizations (i.e., all-causes of
significantly different between incident digoxin-CM elderly users
hospitalizations, 3-month medical expenditure after the index
and digoxin-only users, as well as significantly different between
dates), clinical outcomes (i.e., digoxin intoxication-related clinical
those digoxin elderly users who encountered interactions with
outcomes [digoxin intoxication; ICD-9-CM code ¼ 971.2], occur-
prespecified CMs and their counterpart digoxin-only users
rence of arrhythmia [ventricular arrhythmia, atrioventricular
(Table 3). Although the other factors were not statistically
block, bradycardia], electrolyte imbalance [hyperpotassemia,
significantly associated with incident CM-digoxin use, patients
hypopotassemia, acid-based disorders], acute renal failure,
with heart diseases and BPH had an increased likelihood of
checking digoxin levels, factors associated with digoxin toxicity
incident CM-digoxin use of 115% and 102%, respectively. Defi-
[chronic renal failure, hypomaganesium, hypercalcemia, hypo-
nitely, those elderly who made two to five outpatient visits per
thyroidism]), and other concomitant medications associated with
month and who had ever been prescribed more distinct medi-
digoxin toxicity (i.e., all types of diuretics, potassium supple-
cations tended to newly use digoxin with CMs. Those elderly NHI
ments, angiotensin-converting enzyme inhibitors, p-glycoprotein
beneficiaries enrolled in the south region were approximately
inhibitors, nonsteroidal anti-inflammatory drugs [NSAIDs], and
38% less likely to encounter incident digoxin-CM concurrent use.
medication that might cause transcellular potassium shift) [9].
Of those elderly whom we evaluated for their outcomes (N ¼
692), after 3-month follow-up from the index dates of digoxin-
Statistical Analyses specific CM use and the counterpart digoxin-only use, there was a
The corresponding findings were presented as mean ⫾ SD, or higher occurrence of all-cause hospitalizations, more diagnoses
frequency (relative frequency, %). Differences between groups of with hypopotassemia, more checks of digoxin levels, more con-
patients on continuous variables were analyzed using independ- current prescriptions of potassium-sparing medications and
ent t tests, and differences on nominal-scale variables were NSAIDs, and higher mean total medical expenditure on emer-
analyzed using Pearson’s chi-square test. To explore the factors gency room visits and outpatient visits among the incident
associated with the new concurrent use of digoxin and CMs and digoxin-specific CM elderly users. Almost all these outcomes,
the incident occurrence of digoxin-specific CM interactions however, were not statistically significantly different, except for
among the elderly, patient characteristics and health service the use of potassium-sparing medications and NSAIDs (P ¼ 0.016
utilizations were compared between the two groups. Univariate and o0.001, respectively) (Table 4).
and multivariate logistic regression analyses were performed to
estimate the crude odds ratios, adjusted ORs, and 95% confidence
interval to quantify the risk of incident digoxin-CM use and Discussion
incident digoxin-specific CM interactions. All the potential factors
listed were included in the model for multivariate analyses, and In this study, we found that only 3% of elderly NHI beneficiaries
all analyses were performed using SAS version 9.2 (SAS Institute, were prescribed with digoxin in 2006. Also, they were less likely
Inc., Cary, NC). to be prescribed with concentrated CMs with digoxin (0.43%) and
only half of them were newly prescribed with concentrated CM
(0.22%) in 2006. Although digoxin was prescribed for 190 days on
average to those NHI elderly beneficiaries in 2006, the concen-
Results
trated CMs were somewhat less commonly prescribed concom-
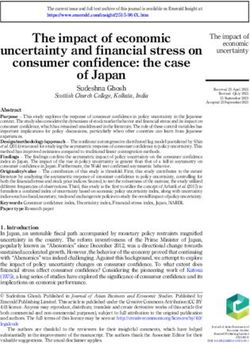
Of the 2 million randomly selected NHI beneficiaries, 9.25% were itantly (i.e., average duration was approximately 17 days). The
considered elderly in 2005 and survived to 2006. There were 6373 following factors were statistically significantly associated with
elderly individuals prescribed with digoxin (prevalence of digoxin the incremental incidence of concurrent digoxin-CM use and the
prescription in elderly ¼ 3.4%) (Fig. 1), and the average duration of incremental occurrence of digoxin-specific CM interactions: pre-
digoxin prescription was 190.41 ⫾ 137.02 days (maximum ¼ 365 vious diagnosis of heart diseases or BPH, outpatient clinic visits
days) in 2006. In total, 789 patients were prescribed with con- per month ranging from two to five, or more distinct medications
centrated CMs for at least 1 day (prevalence of digoxin-CM use prescribed in 2006. In contrast, those elderly NHI beneficiaries
among the elderly ¼ 0.43%). The incidence of digoxin-CM use enrolled in the south region were less likely to encounter incident
among the elderly was 0.22% (N ¼ 400). The average duration of digoxin-CM concurrent use and incident digoxin-specific CM
concurrent use was 17.25 ⫾ 23.89 days (maximum ¼ 228 days) in interactions. More than 96% of all incident digoxin-CM elderly
2006. Of the 400 incident digoxin-CM elderly users, 385 (96.5%) users had encountered the evidence-approved digoxin-specific
had ever encountered evidence-approved digoxin-specific CM CM interactions. Although their 3-month follow-up medical out-
interactions. The most common occurrence of digoxin-specific comes after the initial occurrence were evaluated, no statistically
CM interaction was digoxin-licorice (94% of all incident digoxin- significant findings were found.
CM elderly users and 98% of all incident digoxin-specific CM In this study, we found that elderly patients were relatively
elderly users), and the average duration of concurrent use was less likely to be prescribed with this narrow therapeutic index
16.52 ⫾ 23.65 days in 2006 (Table 1). medication, digoxin, in Taiwan, whereas 17% of older adults were
Although the 1:1 matching approach using specified propen- initially prescribed with digoxin in the United States [30]. Another
sity score was performed, there were some different character- study also showed that 38% of HF NHI beneficiaries of all age
istics between incident digoxin-CM elderly users and digoxin- were prescribed with digoxin and 26% were newly prescribed in
only elderly users, in terms of mean age, presence of heart Taiwan [31]. Although 7% to 21% of the patients with cardiovas-
diseases or benign prostatic hyperplasia (BPH), number of out- cular symptoms took herbal medicine in the United States and
patient clinic visits per month, and number of prescribed distinct other countries [32,33], there was a relatively low prevalence and
medications (Table 2). This implies that incident digoxin-CM incidence of digoxin-CM use among the elderly in this study
elderly users had a higher prevalence of heart diseases and BPH (0.43% and 0.22%, respectively). Such rates were comparatively214 VALUE IN HEALTH REGIONAL ISSUES 3C (2014) 211–221
Subjects who were randomly selected into NationalHealth Insurance
Research Databases [Using 2000 LHID and 2005 LHID databases] in 2005
N=2,000,000
Elderly who were enrolled in NHI in 2005 (i.e., age >=
65 year-old since January 1, 2005)
N=199,631
(Prevalence of elderly=9.98%) Excluding elderly who
withdrew from NHI for
some reasons (e.g., death)
Elderly who were enrolled in NHI in 2005, as well as in 2006 N=14,555
(i.e., age >= 65 year-old since January 1, 2006)
N=185,076
(Prevalence of survival elderly in 2005 and 2006=9.25%)
Elderly who were ever prescribed with digoxin (any brand) for at least one day in 2006
N= 6,373
(Prevalence of subjects being prescribed with digoxin among NHI enrolled elderly in 2006=3.44%)
Elderly who were prescribed with digoxin Elderly who were prescribed with
and concentrated Chinese medications digoxin but had no prescription of
(CMs) concurrently in 2006 concentrated CMs in 2006
N=789 N=5,584
(Prevalence of digoxin-CHM use among
elderly =0.43% )
Excluding elderly who were Randomly select 1:1 matching
ever prescribed with subjects with respect of the
concentrated CMs in six months propensity scores derived from
before the date of concurrent the corresponding combination
use digoxin with CMs; N=389 of the specified variables*
Elderly who were prescribed with digoxin and newly Matched elderly who were prescribed with digoxin
prescribed with concentrated CMs in 2006 only and without CM prescription in 2006
N of incident digoxin-CM elderly users=400 N of matched digoxin-only elderly users =389
(Incidence of digoxin-CM use among elderly= 0.22%) (†N of matched digoxin-only elderly users for
(† N of incident digoxin-specific CM users =385) incident digoxin-specific CM users =385)
Exploring the contributing factors associated with incident digoxin- CM use and incident of
digoxin- specific CM interactions in 2006 among the elderly NHI beneficiaries
Elderly encountered incident digoxin- specific CM Mached digoxin-only elderly users who still
interactions and had health service records after has health service records after three month
three month follow-up since initial concurrent use follow-up since initial concurrent use were
were identified for further assessments identified for further assessments
N=351 N=341
Examining the outcomes associated with new occurrence of digoxin- specific CM
interactions after three month follow-up since initial concurrent use among incident
digoxin-specific CM users and matched digoxin-only elderly users
Fig. 1 – Study population. CM, Chinese medication; LHID, longitudinal health insurance database; NHI, national health
insurance. *For each incident digoxin-CM elderly user, we randomly selected a digoxin user from the propensity score derived
from the combination of the following variables: the month of the index date, the same duration of digoxin use, age, with or
without catastrophic certification, outpatient clinic visits per year, number of prescribed distinct medications, total medical
expenditure. †There were 385 incident digoxin-CM elderly users prescribed with specific CMs, which were proven to have
interactions with digoxin (i.e., incidence of digoxin-specific CM interaction among elderly ¼ 0.21%) so that another 385 elderly
who were prescribed with digoxin only were matched accordingly on the propensity score.
lower than the findings obtained from a nationwide survey in beneficiaries had used NHI-covered TCM services in 2001, 62.5%
Taiwan in 2001 (i.e., 4.3% of all survey participants used both NHI- had used NHI-covered TCM services at least once from 1996 to
covered all kinds of Western medication and TCM) [34] and that 2001, and 86% had ever been prescribed with concentrated CMs in
of our previous population-based cohort study using 1 million Taiwan [35]. In this sense, our study showed that those Western
NHIRD data for all ages of digoxin users (10.7% and 5.4%, medicine physicians who prescribed digoxin for the elderly in
respectively) in 2005 [14]. In addition, the duration of concurrent Taiwan were more conservative than those in other countries,
use in this study was approximately 2 days less than that than for all aged patients with HF, and for all age digoxin users in
obtained from all age incident digoxin-CM users (19.3 ⫾ 29.9 Taiwan. Also, those Chinese medicine physicians more strin-
days) in 2005 [14]. One study showed that 28% of all NHI gently prescribed concentrated CMs for elderly patients withVALUE IN HEALTH REGIONAL ISSUES 3C (2014) 211–221 215
Table 1 – Duration of concurrent use (days) of digoxin with specific CMs, which had evidence of digoxin-CM
interactions, in 2006.
CHM in All digoxin-CHM elderly users (n ¼ 789) Incident digoxin-CHM elderly users (n ¼ 400)
English
Number of Duration of concurrent use (d), Number of Duration of concurrent use (d),
users (%) mean ⫾ SD users (%) mean ⫾ SD
Da huang 190 (24.1) 27.88 ⫾ 50.53 66 (16.5) 13.91 ⫾ 14.66
Hawthorn 34 (4.3) 14.12 ⫾ 22.29 17 (4.3) 10.71 ⫾ 10.68
Dan shen 150 (19.0) 21.42 ⫾ 34.36 66 (16.5) 15.97 ⫾ 19.64
Liquorice 717 (90.9) 27.99 ⫾ 43.84 376 (94) 16.52 ⫾ 23.65
Oyster shell 84 (10.6%) 14.62 ⫾ 17.41 35 (8.75) 10.08 ⫾ 7.93
Siberian 1 (0.1) 30 0 (0.0) –
ginseng
Senna 2 (0.2) 10.5 ⫾ 21.2 0 (0.0) –
Aloe vera 4 (0.5) 7 ⫾ 4.76 1 (0.25) 4
CM, Chinese medication; CHM, Chinese herbal medication.
Table 2 – Comparisons of patient characteristics between incident digoxin-CM elderly users and the
corresponding matched digoxin-only elderly users.
Characteristic n (%) P
Total elderly Incident digoxin- Digoxin-only
digoxin users CHM elderly users elderly users
Sample size 789 400 389
Females 443 (56.15) 225 (56.25) 218 (56.04) 0.9529
Age (y)
Mean 76.45 ⫾ 6.46 75.95 ⫾ 6.15 77.00 ⫾ 6.69 0.0366*
Medium 76 75 77
65–69 118 (14.96) 62 (15.50) 56 (14.40) 0.0732
70–74 215 (27.25) 124 (31.00) 91 (23.39)
75–79 222 (28.14) 105 (26.25) 117 (30.08)
Z80 234 (29.66) 109 (27.25) 125 (32.13)
Monthly reported income (TWD) 0.3007
r17,280 506 (64.13) 256 (64.00) 250 (64.27)
17,281–28,800 267 (33.84) 139 (34.75) 128 (32.90)
28,801–45,800 6 (0.76) 3 (0.75) 3 (0.77)
45,801–72,800 2 (0.25) 1 (0.25) 1 (0.26)
Z72801 8 (1.01) 1 (0.25) 7 (1.80)
Region of NHI enrolment 0.3081
North 379 (48.04) 195 (48.75) 184 (47.30)
Central 180 (22.81) 99 (24.75) 81 (20.82)
South 194 (24.59) 88 (22.00) 106 (27.25)
East 23 (2.92) 12 (3.00) 11 (2.83)
Other 3 (0.72) 5 (1.25) 3 (0.77)
No data 4 (1.03) 1 (0.25) 4 (1.03)
Comorbidity†
Hypertension 491 (62.23) 253 (63.25) 238 (61.18) 0.5576
Heart diseases 629 (79.72) 340 (85.00) 289 (74.29) 0.0002*,‡
Stroke 177 (22.43) 90 (22.50) 87 (22.37) 0.9638
Cancer 31 (3.93) 18 (4.50) 13 (3.34) 0.4656
Diabetes 185 (23.45) 89 (22.25) 96 (24.68) 0.4498
Hyperlipidemia 127 (16.10) 66 (16.50) 61 (15.68) 0.7720
Asthma 71 (9.00) 39 (9.75) 32 (8.23) 0.4590
Pneumonia 52 (6.59) 26 (6.50) 26 (6.68) 1.0000
Benign prostatic hyperplasia 115 (14.58) 73 (18.25) 42 (10.80) 0.0034*,‡
Seizure 11 (1.39) 3 (0.75) 8 (2.06) 0.1382
Depression 59 (7.48) 32 (8.00) 27 (6.94) 0.5909
Chronic kidney disease 6 (0.76) 4 (1.00) 2 (0.05) 0.9872
Outpatient clinic visits in 2006†
Mean ⫾ SD 3.28 ⫾ 2.15 3.60 ⫾ 2.14 2.91 ⫾ 2.08 o0.0001*,‡
continued on next page216 VALUE IN HEALTH REGIONAL ISSUES 3C (2014) 211–221
Table 2 – continued
Characteristic n (%) P
Total elderly Incident digoxin- Digoxin-only
digoxin users CHM elderly users elderly users
Medium 2.2 3.3 2.2
o13 168 (21.29) 55 (13.75) 113 (29.05) o0.0001*
13–24 230 (29.15) 113 (28.25) 117 (30.08)
25–36 159 (20.15) 93 (23.25) 66 (16.97)
37–48 87 (11.03) 53 (12.79) 34 (8.74)
49–60 55 (6.97) 34 (8.50) 21 (5.40)
Z61 90 (11.41) 52 (13.00) 38 (9.77)
Number of prescribed distinct medications†
Mean ⫾ SD 22.26 ⫾ 14.39 25.12 ⫾ 15.18 18.89 ⫾ 12.31 o0.0001*,‡
Medium 19 21.5 16
Total items of prescribed distinct medications† o0.0001*,‡
o10 126 (15.97) 39 (9.75) 87 (22.37)
10–19 296 (37.52) 142 (35.50) 154 (39.59)
20–29 176 (22.31) 93 (23.25) 83 (21.34)
30–39 104 (13.18) 66 (16.50) 38 (9.77)
Z40 87 (11.03) 60 (15.00) 27 (6.94)
Ever hospitalization*,† 163 (20.66) 82 (20.50) 81 (20.82) 0.9301
Total medical expenditure (TWD)†
Mean 44,892.41 42,433.44 47,545.67 0.1634
Min–Max 0–1,293,339 782–1,177,231 0–1,293,339
Medium 21,219.50 21,869 19,804
Interval of total medical expenditure*,† 0.0654
o10,000 181 (22.94) 78 (19.50) 103 (26.48)
10,001–29,999 340 (43.09) 181 (45.25) 159 (40.87)
30,000–49,999 119 (15.08) 68 (17.00) 51 (13.11)
Z50000 149 (18.88) 73 (18.25) 76 (19.54)
Note. We used chi-square tests and t test to compare differences between incident digoxin-CM elderly users and digoxin-only elderly users for
nominal scale and continuous variables.
CM, Chinese medication; CHM, Chinese herbal medication; NHI, National Health Insurance; TWD, New Taiwan dollar.
* There were statistically significant differences between the elderly encountered incident digoxin-CHM use and the corresponding digoxin-
only elderly users.
†
Ascertained during the 6-mo period before the date of first CM prescription.
‡
There were statistically significant differences between elderly encountered incident digoxin-specific CM interactions and the corresponding
digoxin-only elderly users.
Table 3 – Factors associated with exposure of incident concurrent use of digoxin with CHM among the elderly
(logistic regression).
Characteristic Crude OR (95% CI) after single logistic Adjusted OR (95% CI) after multivariate logistic
regression analysis regression analysis
Sex
Male 1 1
Female 0.995 (0.737–1.344) 1.282 (0.910–1.806)
Age (y)
65–69 1 1
70–74 1.024 (0.637–1.644) 1.070 (0.646–1.773)
75–79 0.734 (0.458–1.177) 0.689 (0.416–1.140)
Z80 0.766 (0.479–1.226) 0.735 (0.442–1.221)
Monthly reported
income (TWD)
r17,280 1 1
17,281–28,800 0.957 (0.695–1.316) 1.049 (0.739–1.489)
28,801–45,800 0.593 (0.191–1.839) 0.851 (0.252–2.871)
Region of NHI
enrolment
North 1 1
Central 1.172 (0.800–1.717) 1.050 (0.692–1.592)
continued on next pageVALUE IN HEALTH REGIONAL ISSUES 3C (2014) 211–221 217
Table 3 – continued
Characteristic Crude OR (95% CI) after single logistic Adjusted OR (95% CI) after multivariate logistic
regression analysis regression analysis
South 0.694 (0.479–1.005) 0.621 (0.413–0.934)*
East 1.131 (0.527–2.425) 0.923 (0.401–2.122)
Other 0.307 (0.032–2.977) 0.396 (0.037–4.244)
Disease status†
With hypertension 1.011 (0.745–1.372) 1.014 (0.727–1.416)
With heart disease‡ 1.986 (1.359–2.901)* 2.151 (1.428–3.240)*
With MI 0.773 (0.301–1.982) 0.630 (0.228–1.735)
With ventricular 1.188 (0.747–1.891) 1.168 (0.698–1.953)
arrhythmias
With heart failure 0.848 (0.541–1.331) 0.911 (0.548–1.514)
With stroke 1.050 (0.731–1.509) 1.047 (0.695–1.576)
With cancer 1.246 (0.558–2.785) 1.019 (0.419–2.477)
With diabetes 1.078 (0.683–1.703) 1.019 (0.607–1.712)
With hyperlipidemia 1.052 (0.702–1.577) 0.891 (0.572–1.386)
With asthma 1.154 (0.686–1.939) 0.819 (0.463–1.449)
With pneumonia 0.883 (0.485–1.607) 0.867 (0.426–1.762)
With BPH‡ 1.962 (1.267–3.037)* 2.015 (1.204–3.371)*
With seizure 0.320 (0.064–1.596) 0.271 (0.051–1.453)
With CKD 1.954 (0.356–10.736) 2.835 (0.466–17.251)
Outpatient clinic visits per month*,†
o2 1 1
2–o3 1.846 (1.188–2.869)* 1.757 (1.049–2.942)*
3–o4 2.633 (1.633–4.246)* 2.178 (1.163–4.079)*
4–o5 3.175 (1.783–5.652)* 2.309 (1.084–4.918)*
5–6 3.551 (1.762–7.155)* 2.403 (0.916–6.305)
Z6 2.575 (1.473–4.500)* 1.561 (0.610–3.999)
Total items of prescribed distinct medications†
o10 1 1
10–19 2.074 (1.293–3.326)* 2.212 (1.322–3.700)*
20–29 2.411 (1.445–4.024)* 2.461 (1.332–4.549)*
30–39 3.721 (2.050–6.755)* 3.680 (1.730–7.830)*
Z40 4.850 (2.602–9.040)* 5.044 (2.065–12.323)*
Ever hospitalization† 0.947 (0.652–1.377) 0.853 (0.474–1.535)
Interval of total medical expenditure†
o10,000 1 1
10,001–29,999 1.463 (0.993–2.153) 0.992 (0.639–1.541)
30,000–49,999 1.580 (0.958–2.606) 0.749 (0.394–1.423)
Z50,000 1.216 (0.759–1.948) 0.551 (0.245–1.2365)
BPH, benign prostatic hyperplasia; CI, confidence interval; CKD, chronic kidney disease; CM, Chinese medication; CHM, Chinese herbal
medication; NHI, National Health Insurance; OR, odds ratio.
* There were statistically significant differences between the occurrence of digoxin-CHM interactions, where 95% CI not included 1.
†
There were statistically significant differences between the elderly encountered incident digoxin-CHM use and the corresponding digoxin-
only elderly users.
‡
There were statistically significant differences between the occurrence of digoxin-specific CHM interactions, where 95% CI not included 1.
digoxin for some unknown reasons. Nevertheless, it is unknown likely to be newly prescribed with concentrated CMs, whereas
whether this phenomenon occurred because of concern over such occurrence existed beyond that which is possible due to
potential digoxin toxicities after the announcement of Beer’s chance. In fact, our findings were different from a previous
criteria in 2003 [36] or because of other reasons. study focusing on all age adults who were ever prescribed with
Furthermore, we found that those elderly with heart dis- seven high-risk Western mediations (aspirin, clopidogrel, dipyr-
eases and BPH were 2.15 and 2.02 times, respectively, likely to idamole, ticlopidine, heparin, warfarin, and digoxin) in Taiwan
be newly prescribed with concentrated CMs when they had a [14]. A systematic review showed that Chinese herbal medicine
prescription of digoxin at the same time compared with those is more impressive with regard to the improvement in quality
who did not have these diseases. This was also true when of life, reduction of prostate volume, and the occurrence of
controlled for other factors. In contrast, there were no statisti- adverse events compared with Western medications, although
cally significant differences in the extent of ORs among those the evidence is not robust to support the efficacy of Chinese
who had chronic kidney diseases, myocardium infarction, herbal medicine for BPH [37]. Although the number of patients
ventricular arrhythmias, and HF during the 6-month period with prostate cancers using covered CMs increased from 1996 to
before the index date. Using propensity scores to reduce the 2008 (i.e., 72.8% to 78.8% of all TCM therapies) in Taiwan [38], it
likelihood of selection bias in this study, it implies that those is understandable that the usage of CMs with digoxin among
elderly on digoxin and with heart diseases and BPH were more those elderly with BPH in Taiwan might increase for the218 VALUE IN HEALTH REGIONAL ISSUES 3C (2014) 211–221
Table 4 – Effect of concurrent use of digoxin with CHM after 3-mo follow-up since initial concurrent use.
Effect/outcomes after 3-mo follow-up n (%) P
Total elderly Incident digoxin- Digoxin-only
digoxin users CHM elderly elderly users
(n ¼ 692) users (n ¼ 351) (n ¼ 341)
Health service utilization
All-cause hospitalizations 224 (32.4) 121 (34.5) 103 (30.2) 0.1550
Hospitalization 106 (15.32) 61 (17.38) 45 (13.20) 0.1267
Emergency room visits 118 (17.05) 60 (17.09) 58 (17.01) 0.9762
Three-month medical expenditure after index dates (TWD)
Total ER expenditure/person 31,255 32,219 30,263 0.8489
Total inpatient expenditure/person 26,776 24,707 28,906 0.5350
Total outpatient expenditure/person 109,633 118,498 100,508 0.4669
Clinical outcomes
Disease status and/or disorders related to digoxin
intoxication
Due to digoxin intoxications 2 (0.29) 1 (0.28) 1 (0.29) 0.9837
Due to ventricular arrhythmia and atrioventricular block, 42 (6.07) 19 (5.41) 23 (6.74) 0.4632
bradycardia
Acute renal failure 2 (0.29) 1 (0.28) 1 (0.29) 0.9837
Hypopotassemia 8 (1.16) 5 (1.42) 3 (0.88) 0.5027
Checking digoxin levels in outpatient or inpatient visits 37 (5.35) 20 (5.70) 17 (4.99) 0.6769
Factors associated with digoxin toxicity
Chronic renal failure 5 (0.72) 3 (0.85) 2 (0.59) 0.6771
Hypomaganesium 0 0 0 –
Hypercalcemia 0 0 0 –
Mixed acid-base balance disorder 1 (0.14) 1 (0.28) 0 0.3240
Hyperpotassemia 4 (0.58) 3 (0.85) 1 (0.29) 0.3300
Hypothyroidism 0 0 0 –
Concomitant mediations, which might be associated with
digoxin intoxication and/or toxicity (atrioventricular block,
arrhythmia)
All types of diuretics
Potassium-depleting diuretics
Thiazides 40 (5.78) 20 (5.70) 20 (5.87) 0.9250
Loop 237 (34.25) 124 (35.33) 113 (33.14) 0.5439
Potassium-sparing 77 (11.13) 49 (13.96) 28 (8.21) 0.0162*
Potassium supplements 22 (3.18) 14 (3.99) 8 (2.35) 0.2182
Angiotensin-converting enzyme inhibitors 186 (26.88) 98 (27.92) 88 (25.81) 0.5306
P-Glycoprotein inhibitors 204 (29.48) 109 (31.05) 95 (27.86) 0.3568
Nonsteroidal anti-inflammatory drugs 328 (47.40) 196 (55.84) 132 (38.71) o0.0001*
Medications that might cause transcellular potassium shift 103 (14.88) 55 (15.67) 48 (14.08) 0.5561
CM, Chinese medication; CHM, Chinese herbal medication; ER, emergency room; TWD, New Taiwan dollar.
* Censor up to December 31, if no health service utilization reported in 2006.
aforementioned reasons. We focused only, however, on 1 year beneficiaries enrolled in the south region were less likely to
of NHI utilization in Taiwan in 2006. Therefore, further explo- encounter incident digoxin-CM concurrent use and incident
ration about the utilization of CMs with Western medications digoxin-specific CM interactions, while there was no difference
for prostate-related diseases across time after 2006 or for the among the other regions. Such a finding is inconsistent with our
most updated databases might be necessary. previous study, as well as with the results of other studies
In Taiwan, the implementation of NHI as a single-payer, social [14,25,35,39,40]. In contrast, all the other studies showed that
insurance plan has provided almost all citizens with modest cost NHI beneficiaries enrolled in the central region were more likely
sharing. At present, the coverage of the population is as high as to be prescribed concentrated CMs with Western medications,
99%, so the Bureau of NHI has provided the NHIRD for corre- including digoxin, while no differences were identified among the
sponding research on issues related to cost quality of health other regions in this study. More studies might be necessary to
services, medical practice patterns, accessibility to health care explore the rationales beyond for the regional differences in NHI-
programs, and treatment outcomes at the national or local level. covered CM utilization.
The Bureau of NHI has had contracts with 97% of registered It is reasonable to hypothesize that those elderly NHI benefi-
hospitals, which provide Western and/or Chinese medicine ciaries who ever visited Western and Chinese medicine clinics in
services, since 1996 to ensure sufficient access in Taiwan. the same period of time would require a greater number of
Approximately 92% of all hospitals that provided Chinese med- outpatient visits and would be prescribed with more distinct
icine services were contracted by the Bureau of NHI to offer TCM medications, including Western and Chinese medications. Con-
medical care. In our study, we found that those elderly NHI sequently, these two factors were statistically associated with theVALUE IN HEALTH REGIONAL ISSUES 3C (2014) 211–221 219
incremental incidence of digoxin-CM concurrent use and during the 3-month period after the date of incident digoxin-
digoxin-specific CM interactions. Those who had made two to specific CM interactions and the corresponding digoxin-only use
five outpatient clinic visits per month, however, were more likely in this study. Further studies might be necessary to examine the
to encounter new digoxin-CM concurrent use and digoxin- rationale and the actual risks and benefits of this phenomenon.
specific CM interactions; this was different from our previous Although 32% of all-cause hospitalizations were found in the
study focusing on all age NHI adult beneficiaries for high-risk following 3 months after exposure to digoxin-specific CM inter-
Western medications (including anticoagulants and digoxin) in actions, there were relatively rare occurrences of digoxin intox-
2005 [14]. We presumed that the elderly population might con- ication, arrhythmia, bradycardia, acute renal failure, or hypo-
tribute to such difference. potassemia in this study. These might be due to underreporting
Importantly, this study retrieved the 3-month follow-up or underdocumenting the relevant signs, symptoms, precipitant
information about relevant clinical and economic consequences factors, and associated concomitant medications in the health
after the new occurrence of digoxin-specific CM interactions care settings and/or the fact that no actual harmful effect
among the NHI elderly beneficiaries, which accounted for almost occurred for some reasons. With the relatively less common
all incident digoxin-CM elderly users. Although those who use of digoxin, incident digoxin-CM use, and incident digoxin-
encountered digoxin intoxications might also experience ven- specific CM interactions, the rare occurrence of clinical and
tricular arrhythmia, atrioventricular block, bradycardia, acute economic consequences in any aspect might encounter a type
renal failure, or hypopotassemia, and may require follow-up II error because the sample size is not big enough for the
digoxin level evaluations, we were also concerned about the assessment of outcomes. Further studies using open cohort
other relevant outcomes, including medical care expenditure, across several study years to recruit more subjects might be able
abnormal electrolyte disorders, and concomitant prescribed med- to overcome this pitfall, in particular if digoxin use and digoxin-
ications. All these outcomes might be associated with digoxin CM concurrent use were not as rare as our findings suggest.
toxicities, other than the all-cause hospitalizations. Finally, we In addition, several other limitations in our study need to be
did not find any statistically significant difference in these addressed. First, there is limited information describing actual
potentially relevant outcomes, the factors associated with medication use patterns (NHI-covered medications only), disease
digoxin toxicity, or the concomitant medications. status (up to three diagnoses were documented in outpatient
The incident digoxin-specific CM elderly users, however, were data sets and up to five diagnoses in inpatient data sets), and
prescribed with more potassium-sparing diuretics and NSAIDs health service utilization patterns (only NHI-covered and co-
than their counterpart digoxin-only elderly users. It is unclear payment) using the NHIRD, which are derived from the LHID
whether the potassium-sparing diuretics were prescribed to administrative claimed data sets. Unfortunately, the correspond-
manage the problem of hypopotassemia, to prevent the occur- ing indications of CMs and digoxin were unknown using the
rence of digoxin toxicities, or for other reasons. Although 0.39% of NHIRD. In fact, the relevant ICD-9 codes, in terms of indications
new digoxin users were diagnosed with digoxin intoxication (ICD- for all prescribed Western medicine, are required in each CM
9 code ¼ 972.1) among all 590,955 patients with HF from 2001 to prescription, although TCM physicians usually make their deci-
2004 in Taiwan in Wang et al.’s study [31], only 1 elderly sions of CM prescription on the basis of complex TCM theories
individual in each group was documented to have encountered (e.g., yin/yang, five elements, Jing, blood, qi, Jin Ye). Thus, the
digoxin intoxication during the 3-month period after the index listed ICD-9 codes associated with CMs and digoxin were ascer-
dates of the incident occurrence of digoxin-specific CM interac- tained during the 6-month period before the dates of first CM
tions in this study. In other words, the incidence of documented prescription, in terms of index dates. Focusing on 1 year of NHI
digoxin intoxication was relatively low (i.e., 0.03%) among all utilization in 2006 in Taiwan, the definition of 1-day exposure
elderly prescribed with digoxin in 2006 in this study. Although might cause the overestimation of its incidence and prevalence
the nested case-control studies using open cohorts were per- of concurrent use. Although only 6% of the adults had ever used
formed to explore the risks of exposing interactions between noncovered TCM therapies [44] and the majority of all NHI
digoxin and diuretics, as well as other medications [31,41], further beneficiaries using TCM therapies had ever been prescribed with
studies using different study designs (e.g., nested case-control concentrated CMs in Taiwan [35], this study explored the actual
study, case cross-over study) to involve more subjects and concurrent use patterns of digoxin with concentrated CMs among
compare subjects by themselves might be necessary to confirm the elderly. Second, there is more than one active chemical
our findings. compound in one single CM, which might have various concen-
A previous study demonstrated that higher serum digoxin trations of corresponding chemical compounds due to coming
concentrations were statistically associated with incremental from different locations and seasons. There are no official docu-
mortality for those patients with HF [42]. The use of digoxin ments listing all active chemical compounds in the concentrated
was associated with a significant increase in all-cause mortality CM products yet, let alone having published information listing
in patients with atrial fibrillation [43]. Although HF and atrial the recommended dose/concentration, duration, and frequency
fibrillation are common diseases among the elderly, digoxin of any particular chemical compound. Thus, it is unknown what
utilization is indeed decreased in Taiwan compared with HF- chemical compounds in the concentrated CMs interact with
related findings obtained from Wang et al.’s study between 2001 digoxin. Instead, we focused on those prespecified CMs that were
and 2004 [31]. It is presumed that one reason for this might be the documented in various levels of the literature. Although several
inferior effectiveness of treatment compared with beta- of these CMs are either a component of Asian food or an
adrenergic inhibitors, angiotensin-converting enzyme inhibitors, ingredient in Asian cuisine, unfortunately, the NHIRD included
and angiotensin II receptor blockers for HF [9]. Nevertheless, only those covered CMs. Information about the diets, nutrition, or
several studies have recommended not overlooking digoxin foods with these CMs in the NHIRD is available.
toxicities, especially for those who are older, female patients, Third, the extent of concurrent use in this study was different
with low lean body weight, with renal insufficiency, and with from that in other studies due to the different data resources,
concomitant medication use [9,14,42,43]. All these studies sug- study designs, and focused populations, as well as the definitions
gest that checking digoxin concentration is necessary to evaluate of Western medications and CMs. For instance, by using the
the risk and benefit for those digoxin users for any condition. NHIRD we cannot know for what indications these concentrated
Only approximately 5% of all elderly individuals with digoxin CMs were prescribed. The review of medical charts using in-
prescriptions, however, were ordered to check their digoxin levels house databases across different hospital settings might be able220 VALUE IN HEALTH REGIONAL ISSUES 3C (2014) 211–221
to provide such indication-related information. Fourth, the speci- [4] Cheung CK, Wyman JF, Halcon LL. Use of complementary and
fied propensity scores were used to 1:1 match the counterpart alternative therapies in community-dwelling older adults. J Altern
Complement Med 2007;13:997–1006.
digoxin-only elderly users with incident digoxin-CM elderly users
[5] Eisenberg DM, Davis RB, Ettner SL, et al. Trends in alternative medicine
and incident digoxin-specific CM users. There were still some use in the United States, 1990-1997: results of a follow-up national
different characteristics between incident digoxin-CM elderly survey. JAMA 1998;280:1569–75.
users/incident digoxin-specific CM elderly users and the corre- [6] Alherbish A, Charrois TL, Ackman ML, et al. The prevalence of natural
sponding digoxin-only elderly users. Thus, we did not perform health product use in patients with acute cardiovascular disease. PloS
One 2011;6:e19623.
conditional logistic regression, as other studies did [11,32], to
[7] Chung VC, Hillier S, Lau CH, et al. Referral to and attitude towards
examine the factors associated with new concurrent use and traditional Chinese medicine amongst western medical doctors in
interactions of digoxin and CMs. Instead, we conducted tradi- postcolonial Hong Kong. Soc Sci Med 2011;72:247–55.
tional univariate and multivariate logistic regression analyses, [8] Ahmed A. DEFEAT - Heart Failure: a guide to management of geriatric
which assumed that individuals were independent from each heart failure by generalist physicians. Minerva Medica 2009;100:39–50.
[9] Yang EH, Shah S, Criley JM. Digitalis toxicity: a fading but crucial
other. Furthermore, although our findings could be an example to complication to recognize. Am J Med 2012;125:337–43.
other countries practicing Chinese medicine or CAMs commonly, [10] American Geriatrics Society Beers Criteria Update Expert Panel.
future cross-nation studies in Asia or worldwide might be needed American Geriatrics Society updated Beers Criteria for potentially
to verify the findings and enhance their generalization. inappropriate medication use in older adults. J Am Geriatr Soc
In conclusion, there were relatively rare incidents of digoxin 2012;60:616–31.
[11] Chan AL, Wang MT, Su CY, Tsai FH. Risk of digoxin intoxication caused
prescription, digoxin-CM use, and the occurrence of new digoxin- by clarithromycin-digoxin interactions in heart failure patients: a
specific CM interactions among the elderly in Taiwan. Although population-based study. Eur J Clin Pharmacol 2009;65:1237–43.
those who used more outpatient services and medications might [12] Chow L, Johnson M, Wells A, Dasgupta A. Effect of the traditional
increase the exposure of incident digoxin-CM use and incident Chinese medicines Chan Su, Lu-Shen-Wan, Dan Shen, and Asian
ginseng on serum digoxin measurement by Tina-quant (Roche) and
digoxin-specific CM interactions among the elderly, more atten-
Synchron LX system (Beckman) digoxin immunoassays. J Clin Lab Anal
tion should be paid to those elderly with specific diseases (heart 2003;17:22–7.
disease and BPH) and checking their digoxin concentration more [13] Tankanow R, Tamer HR, Streetman DS, et al. Interaction study between
aggressively to follow-up the risks and benefits. We recognize digoxin and a preparation of hawthorn (Crataegus oxyacantha). J Clin
this study as an initiative to explore the elderly concurrent use of Pharmacol 2003;3:637–42.
[14] Tsai HH, Lin HW, Chien CR, Li TC. Concurrent use of antiplatelets,
CMs with digoxin, and demonstrated that no significant harm
anticoagulants, or digoxin with Chinese medications: a population-
occurred. Overall, these findings are substantial and informative based cohort study. Eur J Clin Pharmacol 2013;69(3):629–39.
to support that Taiwanese physicians practicing either Western [15] Mashour NH, Lin GI, Frishman WH. Herbal medicine for the treatment
medicine or Chinese medicine are very responsible in prescribing of cardiovascular disease: clinical considerations. Arch Intern Med
medications cautiously for the elderly. It is presumed that they 1998;158:2225–34.
[16] Izzo A, Ernst E. Interactions between herbal medicines and prescribed
intend to mitigate problems associated with a system that has drugs. Drugs 2001;61:2163–75.
patients using multiple prescribers and visiting multiple hospital [17] Yaheya Mohammad IM. Herb-drug interactions and patient counseling.
settings, possibly with concerns about medication toxicities that Int J Pharm Pharm Sci 2009;1:151–9.
the patient may experience. [18] World Health Organization. WHO Guidelines on Safety Monitoring of
Herbal Medicines in Pharmacovigilance Systems. Geneva, Switzerland:
World Health Organization, 2004:1–82.
[19] Albert NM, Rathman L, Ross D, et al. Predictors of over-the-counter
drug and herbal therapies use in elderly patients with heart failure. J
Card Fail 2009;15:600–6.
[20] Tindle HA, Davis RB, Phillips RS, Eisenberg DM. Trends in use of
Acknowledgments
complementary and alternative medicine by US adults: 1997–2002.
This study is based in part on data from the National Health Altern Ther Health Med 2005;1:42–9.
[21] Rossler W, Lauber C, Angst J, et al. The use of complementary and
Insurance Research Database provided by the Bureau of National
alternative medicine in the general population: results from a
Health Insurance, Department of Health, and managed by longitudinal community study. Psychol Med 2007;37:73–84.
National Health Research Institutes. The interpretation and con- [22] Chou P. Factors related to utilization of traditional Chinese medicine in
clusions contained herein do not represent those of the Bureau of Taiwan. Zhonghua Yi Xue Za Zhi (Taipei) 2001;64:191–202.
National Health Insurance, Department of Health or National [23] Sibbritt D, Adams J, Murthy V. The prevalence and determinants of
Chinese medicine use by Australian women: analysis of a cohort of
Health Research Institutes, and financial sponsors. 10,287 women aged 56–61 years. Am J Chin Med 2013;41:281–91.
Source of financial support: This study was fully supported by [24] Shih CC, Liao CC, Su YC, et al. Gender differences in traditional Chinese
the National Science Council (NSC 99-2320-B-039-031-MY3), and medicine use among adults in Taiwan. PloS One 2012;7:e32540.
partially sponsored by other studies, CCMP-102-RD-003 and NSC [25] Chang LC, Huang N, Chou YJ, et al. Utilization patterns of Chinese
medicine and Western medicine under the National Health Insurance
102-2320-B-039-007. The funding agencies had no role in the
Program in Taiwan, a population-based study from 1997 to 2003. BMC
study implementation, analysis or interpretation of data, or Health Serv Res 2008;8:170.
preparation, review, or approval of the manuscript. The authors [26] Department of Chinese Medicine and Pharmacy, Ministry of Health and
would like to express their gratitude to I-Wen Yu, Yi-Liang Chen, Welfare, Executive Yuan. Related Regulations for Chinese Medications.
and Shan-Chieh Wu for their assistance to implement the study. Available from: http://www.mohw.gov.tw/CHT/DOCMAP/DM1.aspx?f_
list_no=204&fod_list_no=138. [Accessed May 12, 2014].
[27] Department of Chinese Medicine and Pharmacy, Ministry of Health and
R EF E R EN CE S Welfare, Executive Yuan. Permit license of Chinese medications.
Avalable from: http://www.mohw.gov.tw/CHT/DOCMAP/query_liense.
aspx?mode=1. [Accessed March 24, 2014].
[28] Tsai HH, Lin HW, Lu YH, et al. A review of potential harmful
[1] Gallagher P, Barry P, O’Mahony D. Inappropriate prescribing in the interactions between anticoagulant/antiplatelet agents and Chinese
elderly. J Clin Pharm Ther 2007;32:113–21. herbal medicines. PloS One 2013;8:e64255.
[2] Obreli-Neto PR, Nobili A, de Oliveira Baldoni A, et al. Adverse drug [29] Mehta DH, Phillips RS, Davis RB, McCarthy EP. Use of complementary
reactions caused by drug-drug interactions in elderly outpatients: a and alternative therapies by Asian Americans: results from the
prospective cohort study. Eur J Clin Pharmacol 2012;68:1667–76. National Health Interview Survey. J Gen Intern Med 2007;22:762–7.
[3] Grant SJ, Yu SB, Kiat H, Chang D. The use of complementary and [30] Gagne JJ, Polinski JM, Kesselheim AS, et al. Patterns and predictors of
alternative medicine by people with cardiovascular disease: a generic narrow therapeutic index drug use among older adults. J Am
systematic review. BMC Public Health 2012;12:299. Geriatr Soc 2013;61:1586–91.You can also read