Management of Newly Diagnosed Type 2 Diabetes Mellitus (T2DM) in Children and Adolescents abstract
←
→
Page content transcription
If your browser does not render page correctly, please read the page content below
Organizational Principles to Guide and Define the Child
Health Care System and/or Improve the Health of all Children
CLINICAL PRACTICE GUIDELINE
Management of Newly Diagnosed Type 2 Diabetes
Mellitus (T2DM) in Children and Adolescents
abstract Kenneth C. Copeland, MD, Janet Silverstein, MD, Kelly R.
Moore, MD, Greg E. Prazar, MD, Terry Raymer, MD, CDE,
Richard N. Shiffman, MD, Shelley C. Springer, MD, MBA,
Over the past 3 decades, the prevalence of childhood obesity has increased
Vidhu V. Thaker, MD, Meaghan Anderson, MS, RD, LD, CDE,
dramatically in North America, ushering in a variety of health problems, Stephen J. Spann, MD, MBA, and Susan K. Flinn, MA
including type 2 diabetes mellitus (T2DM), which previously was not typically
KEY WORDS
seen until much later in life. The rapid emergence of childhood T2DM poses diabetes, type 2 diabetes mellitus, childhood, youth, clinical
challenges to many physicians who find themselves generally ill-equipped to practice guidelines, comanagement, management, treatment
treat adult diseases encountered in children. This clinical practice guideline ABBREVIATIONS
was developed to provide evidence-based recommendations on managing AAP—American Academy of Pediatrics
10- to 18-year-old patients in whom T2DM has been diagnosed. The American AAFP—American Academy of Family Physicians
BG—blood glucose
Academy of Pediatrics (AAP) convened a Subcommittee on Management of FDA—US Food and Drug Administration
T2DM in Children and Adolescents with the support of the American Diabetes HbA1c—hemoglobin A1c
Association, the Pediatric Endocrine Society, the American Academy of Family PES—Pediatric Endocrine Society
Physicians, and the Academy of Nutrition and Dietetics (formerly the Amer- T1DM—type 1 diabetes mellitus
T2DM—type 2 diabetes mellitus
ican Dietetic Association). These groups collaborated to develop an evidence TODAY—Treatment Options for type 2 Diabetes in Adolescents
report that served as a major source of information for these practice guide- and Youth
line recommendations. The guideline emphasizes the use of management This document is copyrighted and is property of the American
modalities that have been shown to affect clinical outcomes in this pediatric Academy of Pediatrics and its Board of Directors. All authors
population. Recommendations are made for situations in which either in- have filed conflict of interest statements with the American
Academy of Pediatrics. Any conflicts have been resolved through
sulin or metformin is the preferred first-line treatment of children and ado- a process approved by the Board of Directors. The American
lescents with T2DM. The recommendations suggest integrating lifestyle Academy of Pediatrics has neither solicited nor accepted any
modifications (ie, diet and exercise) in concert with medication rather than commercial involvement in the development of the content of
as an isolated initial treatment approach. Guidelines for frequency of mon- this publication.
itoring hemoglobin A1c (HbA1c) and finger-stick blood glucose (BG) concen- The recommendations in this report do not indicate an exclusive
course of treatment or serve as a standard of medical care.
trations are presented. Decisions were made on the basis of a systematic
Variations, taking into account individual circumstances, may be
grading of the quality of evidence and strength of recommendation. The appropriate.
clinical practice guideline underwent peer review before it was approved All clinical practice guidelines from the American Academy of
by the AAP. This clinical practice guideline is not intended to replace clinical Pediatrics automatically expire 5 years after publication unless
judgment or establish a protocol for the care of all children with T2DM, and reaffirmed, revised, or retired at or before that time.
its recommendations may not provide the only appropriate approach to the
management of children with T2DM. Providers should consult experts
trained in the care of children and adolescents with T2DM when treatment
goals are not met or when therapy with insulin is initiated. The AAP acknowl-
edges that some primary care clinicians may not be confident of their ability
to successfully treat T2DM in a child because of the child’s age, coexisting
conditions, and/or other concerns. At any point at which a clinician feels he
or she is not adequately trained or is uncertain about treatment, a referral
to a pediatric medical subspecialist should be made. If a diagnosis of T2DM
is made by a pediatric medical subspecialist, the primary care clinician www.pediatrics.org/cgi/doi/10.1542/peds.2012-3494
should develop a comanagement strategy with the subspecialist to ensure doi:10.1542/peds.2012-3494
that the child continues to receive appropriate care consistent with a med-
PEDIATRICS (ISSN Numbers: Print, 0031-4005; Online, 1098-4275).
ical home model in which the pediatrician partners with parents to ensure
Copyright © 2013 by the American Academy of Pediatrics
that all health needs are met. Pediatrics 2013;131:364–382
364 FROM THE AMERICAN ACADEMY OF PEDIATRICS
Downloaded from pediatrics.aappublications.org by guest on May 15, 2015FROM THE AMERICAN ACADEMY OF PEDIATRICS
Key action statements are as follows: cents at the time of diagnosis of b. are initiating or changing their
1. Clinicians must ensure that insulin T2DM. diabetes treatment regimen; or
therapy is initiated for children c. have not met treatment goals; or
and adolescents with T2DM who 3. The committee suggests that clini- d. have intercurrent illnesses.
are ketotic or in diabetic ketoacidosis cians monitor HbA1c concentra-
and in whom the distinction be- tions every 3 months and intensify 5. The committee suggests that clini-
tween types 1 and 2 diabetes mel- treatment if treatment goals for cians incorporate the Academy
finger-stick BG and HbA1c concen- of Nutrition and Dietetics’ Pediatric
litus is unclear and, in usual cases,
trations are not being met (intensi- Weight Management Evidence-Based
should initiate insulin therapy for
fication is defined in the Definitions Nutrition Practice Guidelines in their
patients
box). dietary or nutrition counseling of
a. who have random venous or patients with T2DM at the time of
plasma BG concentrations ≥250 diagnosis and as part of ongoing
mg/dL; or 4. The committee suggests that clini-
management.
b. whose HbA1c is >9%. cians advise patients to monitor
finger-stick BG (see Key Action 6. The committee suggests that clini-
2. In all other instances, clinicians Statement 4 in the guideline for cians encourage children and ado-
should initiate a lifestyle modifi- further details) concentrations in lescents with T2DM to engage in
cation program, including nutri- patients who moderate-to-vigorous exercise for
tion and physical activity, and a. are taking insulin or other med- at least 60 minutes daily and to
start metformin as first-line ications with a risk of hypoglyce- limit nonacademic “screen time”
therapy for children and adoles- mia; or to less than 2 hours a day.
Definitions
Adolescent: an individual in various stages of maturity, generally considered to be between 12 and 18 years of age.
Childhood T2DM: disease in the child who typically
is overweight or obese (BMI ≥85th–94th and >95th percentile for age and gender, respectively);
has a strong family history of T2DM;
has substantial residual insulin secretory capacity at diagnosis (reflected by normal or elevated insulin and
C-peptide concentrations);
has insidious onset of disease;
demonstrates insulin resistance (including clinical evidence of polycystic ovarian syndrome or acanthosis
nigricans);
lacks evidence for diabetic autoimmunity (negative for autoantibodies typically associated with T1DM). These patients
are more likely to have hypertension and dyslipidemia than are those with T1DM.
Clinician: any provider within his or her scope of practice; includes medical practitioners (including physicians and
physician extenders), dietitians, psychologists, and nurses.
Diabetes: according to the American Diabetes Association criteria, defined as
1. HbA1c ≥6.5% (test performed in an appropriately certified laboratory); or
2. fasting (defined as no caloric intake for at least 8 hours) plasma glucose ≥126 mg/dL (7.0 mmol/L); or
3. 2-hour plasma glucose ≥200 mg/dL (11.1 mmol/L) during an oral glucose tolerance test performed as described by
the World Health Organization by using a glucose load containing the equivalent of 75 g anhydrous glucose dissolved
in water; or
4. a random plasma glucose ≥200 mg/dL (11.1 mmol/L) with symptoms of hyperglycemia.
PEDIATRICS Volume 131, Number 2, February 2013 365
Downloaded from pediatrics.aappublications.org by guest on May 15, 2015(In the absence of unequivocal hyperglycemia, criteria 1–3 should be confirmed by repeat testing.) Diabetic ketoacidosis: acidosis resulting from an absolute or relative insulin deficiency, causing fat breakdown and formation of β hydroxybutyrate. Symptoms include nausea, vomiting, dehydration, Kussmaul respirations, and altered mental status. Fasting blood glucose: blood glucose obtained before the first meal of the day and after a fast of at least 8 hours. Glucose toxicity: The effect of high blood glucose causing both insulin resistance and impaired β-cell production of insulin. Intensification: Increase frequency of blood glucose monitoring and adjustment of the dose and type of medication in an attempt to normalize blood glucose concentrations. Intercurrent illnesses: Febrile illnesses or associated symptoms severe enough to cause the patient to stay home from school and/or seek medical care. Microalbuminuria: Albumin:creatinine ratio ≥30 mg/g creatinine but
FROM THE AMERICAN ACADEMY OF PEDIATRICS
T2DM.13,14 The National Diabetes Edu- T2DM, and should communicate and interventions as well as face-to-
cation Program TIP sheets (which can work closely with a diabetes team of face or peer-enhanced activities)
be ordered or downloaded from www. subspecialists when such consultation appear to foster better results, at
yourdiabetesinfo.org or ndep.nih.gov) is available, practical, and appropriate. least for weight management. 23
provide guidance on healthy eating, The frequency of such consultations Success in making lifestyle changes
physical activity, and dealing with will vary, but should usually be to attain therapeutic goals requires
T2DM in children and adolescents, but obtained at diagnosis and then at least the initial and ongoing education of the
few other resources are available that annually if possible. When treatment patient and the entire family about
are directly targeted at youth with this goals are not met, the committee healthy nutrition and exercise. Any be-
disease.15 Most medications used for encourages clinicians to consult with havior change recommendations must
T2DM have been tested for safety and an expert trained in the care of chil- establish realistic goals and take into
efficacy only in people older than 18 dren and adolescents with T2DM.18,19 account the families’ health beliefs
years, and there is scant scientific When first-line therapy (eg, metfor- and behaviors. Understanding the pa-
evidence for optimal management of min) fails, recommendations for in- tient and family’s perception of the
children with T2DM.16,17 Recognizing the tensifying therapy should be generally disease (and overweight status) before
scarcity of evidence-based data, this the same for pediatric and adult establishing a management plan is im-
report provides a set of guidelines for populations. The picture is constantly portant to dispel misconceptions and
the management and treatment of changing, however, as new drugs are promote adherence.24 Because T2DM
children with T2DM that is based on introduced, and some drugs that ini- disproportionately affects minority pop-
a review of current medical literature tially appeared to be safe demon- ulations, there is a need to ensure cul-
covering a period from January 1, 1990, strate adverse effects with wider use. turally appropriate, family-centered care
to July 1, 2008. Clinicians should, therefore, remain along with ongoing education.25–28 Sev-
alert to new developments with regard eral observational studies cite the im-
Despite these limitations, the practic-
to treatment of T2DM. Seeking the ad- portance of addressing cultural issues
ing physician is likely to be faced with
vice of an expert can help ensure that within the family.20–22
the need to provide care for children
the treatment goals are appropriately
with T2DM. Thus, the American Acad-
set and that clinicians benefit from Restrictions in Creating This
emy of Pediatrics (AAP), the Pediatric
cutting-edge treatment information in Document
Endocrine Society (PES), the American
this rapidly changing area. In developing these guidelines, the
Academy of Family Physicians (AAFP),
American Diabetes Association, and The Importance of Family-Centered following restrictions governed the
the Academy of Nutrition and Dietetics Diabetes Care committee’s work:
(formerly the American Dietetic Asso- Family structure, support, and educa- Although the importance of diabe-
ciation) partnered to develop a set of tion help inform clinical decision-making tes detection and screening of at-
guidelines that might benefit endo- and negotiations with the patient and risk populations is acknowledged
crinologists and generalists, including family about medical preferences that and referenced, the guidelines
pediatricians and family physicians affect medical decisions, independent are restricted to patients meeting
alike. This clinical practice guideline of existing clinical recommendations. the diagnostic criteria for diabetes
may not provide the only appropriate Because adherence is a major issue in (eg, this document focuses on
approach to the management of chil- any lifestyle intervention, engaging the treatment postdiagnosis). Specifi-
dren with T2DM. It is not expected to family is critical not only to maintain cally, this document and its recom-
serve as a sole source of guidance in needed changes in lifestyle but also to mendations do not pertain to
the management of children and ado- foster medication adherence.20–22 The patients with impaired fasting
lescents with T2DM, nor is it intended to family’s ideal role in lifestyle inter- plasma glucose (100–125 mg/dL)
replace clinical judgment or establish ventions varies, however, depend- or impaired glucose tolerance (2-
a protocol for the care of all children ing on the child’s age. Behavioral hour oral glucose tolerance test
with this condition. Rather, it is intended interventions in younger children plasma glucose: 140–200 mg/dL)
to assist clinicians in decision-making. have shown a favorable effect. With or isolated insulin resistance.
Primary care providers should en- adolescents, however, interventions Although it is noted that the dis-
deavor to obtain the requisite skills to based on target-age behaviors (eg, tinction between types 1 and 2 di-
care for children and adolescents with including phone or Internet-based abetes mellitus in children may be
PEDIATRICS Volume 131, Number 2, February 2013 367
Downloaded from pediatrics.aappublications.org by guest on May 15, 2015difficult,29,30 these recommendations These groups partnered to develop operators NOT, AND, OR were included in
pertain specifically to patients 10 an evidence report that served as a various combinations. Articles address-
to less than 18 years of age with major source of information for these ing treatment of diabetes mellitus were
T2DM (as defined above). practice guideline recommendations.31 prospectively limited to those that were
Although the importance of high-risk Specific clinical questions addressed published in English between January
care and glycemic control in preg- in the evidence review were as fol- 1990 and June 2008, included abstracts,
nancy, including pregravid glycemia, lows: (1) the effectiveness of treat- and addressed children between the
is affirmed, the evidence considered ment modalities for T2DM in children ages of 120 and 215 months with an
and recommendations contained in and adolescents, (2) the efficacy of established diagnosis of T2DM. Studies
this document do not pertain to di- pharmaceutical therapies for treat- in adults were considered for inclusion
abetes in pregnancy, including dia- ment of children and adolescents with if >10% of the study population was
betes in pregnant adolescents. T2DM, (3) appropriate recommen- 45 years of age or younger. The Med-
dations for screening for comorbid- line search limits included the fol-
Recommended screening sched-
ities typically associated with T2DM lowing: clinical trial; meta-analysis;
ules and management tools for
in children and adolescents, and (4) randomized controlled trial; review;
select comorbid conditions (hyper-
treatment recommendations for comor- child: 6–12 years; and adolescent:
tension, dyslipidemia, nephropathy,
bidities of T2DM in children and ado- 13–18 years. Additional articles were
microalbuminuria, and depression)
lescents. The accompanying technical identified by review of reference lists
are provided as resources in the
report contains more information on of relevant articles and ongoing
accompanying technical report.31
comorbidities.31 studies recommended by a technical
These therapeutic recommenda-
Epidemiologic project staff searched expert advisory group. All articles
tions were adapted from other rec-
Medline, the Cochrane Collaboration, were reviewed for compliance with
ommended guideline documents
and Embase. MESH terms used in the search limitations and appro-
with references, without an inde-
various combinations in the search priateness for inclusion in this
pendent assessment of their sup-
included diabetes, mellitus, type 2, type document.
porting evidence.
1, treatment, prevention, diet, pediat- Initially, 199 abstracts were identified
METHODS ric, T2DM, T1DM, NIDDM, metformin, for possible inclusion, of which 52
lifestyle, RCT, meta-analysis, child, ad- were retained for systematic review.
A systematic review was performed olescent, therapeutics, control, adult, Results of the literature review were
and is described in detail in the ac- obese, gestational, polycystic ovary presented in evidence tables and
companying technical report.31 To de- syndrome, metabolic syndrome, car- published in the final evidence report.
velop the clinical practice guideline on diovascular, dyslipidemia, men, and An additional literature search of
the management of T2DM in children women. In addition, the Boolean Medline and the Cochrane Database of
and adolescents, the AAP convened
the Subcommittee on Management of
T2DM in Children and Adolescents
with the support of the American Di-
abetes Association, the PES, the AAFP,
and the Academy of Nutrition and
Dietetics. The subcommittee was
co-chaired by 2 pediatric endocrinol-
ogists preeminent in their field and
included experts in general pediat-
rics, family medicine, nutrition, Native
American health, epidemiology, and
medical informatics/guideline method-
ology. All panel members reviewed the
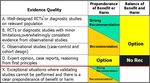
AAP policy on Conflict of Interest and FIGURE 1
Voluntary Disclosure and declared all Evidence quality. Integrating evidence quality appraisal with an assessment of the anticipated balance
between benefits and harms if a policy is carried out leads to designation of a policy as a strong
potential conflicts (see conflicts state- recommendation, recommendation, option, or no recommendation.32 RCT, randomized controlled
ments in the Task Force member list). trial; Rec, recommendation.
368 FROM THE AMERICAN ACADEMY OF PEDIATRICS
Downloaded from pediatrics.aappublications.org by guest on May 15, 2015FROM THE AMERICAN ACADEMY OF PEDIATRICS
TABLE 1 Definitions and Recommendation Implications
Statement Definition Implication
Strong recommendation A strong recommendation in favor of a particular action is Clinicians should follow a strong recommendation unless
made when the anticipated benefits of the recommended a clear and compelling rationale for an alternative approach
intervention clearly exceed the harms (as a strong is present.
recommendation against an action is made when the
anticipated harms clearly exceed the benefits) and the
quality of the supporting evidence is excellent. In some
clearly identified circumstances, strong recommendations
may be made when high-quality evidence is impossible to
obtain and the anticipated benefits strongly outweigh the
harms.
Recommendation A recommendation in favor of a particular action is made when Clinicians would be prudent to follow a recommendation but
the anticipated benefits exceed the harms but the quality of should remain alert to new information and sensitive to
evidence is not as strong. Again, in some clearly identified patient preferences.
circumstances, recommendations may be made when high-
quality evidence is impossible to obtain but the anticipated
benefits outweigh the harms.
Option Options define courses that may be taken when either the Clinicians should consider the option in their decision-making,
quality of evidence is suspect or carefully performed studies and patient preference may have a substantial role.
have shown little clear advantage to 1 approach over
another.
No recommendation No recommendation indicates that there is a lack of pertinent Clinicians should be alert to new published evidence that
published evidence and that the anticipated balance of clarifies the balance of benefit versus harm.
benefits and harms is presently unclear.
It should be noted that, because childhood T2DM is a relatively recent medical phenomenon, there is a paucity of evidence for many or most of the recommendations provided. In some
cases, supporting references for a specific recommendation are provided that do not deal specifically with childhood T2DM, such as T1DM, childhood obesity, or childhood “prediabetes,”
or that were not included in the original comprehensive search. Committee members have made every effort to identify those references that did not affect or alter the level of evidence
for specific recommendations.
Systematic Reviews was performed the final evidence report. An epide- on a late draft of these recommendations,
in July 2009 for articles discussing miologist appraised the methodo- using the GuideLine Implementability
recommendations for screening and logic quality of the research before it Appraisal.33 Several potential obsta-
treatment of 5 recognized comorbidities was considered by the committee cles to successful implementation
of T2DM: cardiovascular disease, dysli- members. were identified and resolved in the
pidemia, retinopathy, nephropathy, and The evidence-based approach to final guideline. Evidence was in-
peripheral vascular disease. Search guideline development requires that corporated systematically into 6 key
criteria were the same as for the search the evidence in support of each key action statements about appropriate
on treatment of T2DM, with the inclusion action statement be identified, ap- management facilitated by BRIDGE-Wiz
of the term “type 1 diabetes mellitus.” praised, and summarized and that an software (Building Recommendations
Search terms included, in various com- explicit link between evidence and in a Developer’s Guideline Editor; Yale
binations, the following: diabetes, melli- recommendations be defined. Evidence- Center for Medical Informatics).
tus, type 2, type 1, pediatric, T2DM, based recommendations reflect the A draft version of this clinical practice
T1DM, NIDDM, hyperlipidemia, retinopa- quality of evidence and the balance of guideline underwent extensive peer re-
thy, microalbuminuria, comorbidities, benefit and harm that is anticipated view by 8 groups within the AAP, the
screening, RCT, meta-analysis, child, and when the recommendation is followed. American Diabetes Association, PES,
adolescent. Boolean operators and The AAP policy statement, “Classifying AAFP, and the Academy of Nutrition and
search limits mirrored those of the Recommendations for Clinical Practice Dietetics. Members of the subcommittee
primary search. Guidelines,”32 was followed in desig- were invited to distribute the draft to
An additional 336 abstracts were nating levels of recommendation (see other representatives and committees
identified for possible inclusion, of Fig 1 and Table 1). within their specialty organizations. The
which 26 were retained for systematic To ensure that these recommendations resulting comments were reviewed by
review. Results of this subsequent can be effectively implemented, the the subcommittee and incorporated into
literature review were also presented Guidelines Review Group at Yale Center the guideline, as appropriate. All AAP
in evidence tables and published in for Medical Informatics provided feedback guidelines are reviewed every 5 years.
PEDIATRICS Volume 131, Number 2, February 2013 369
Downloaded from pediatrics.aappublications.org by guest on May 15, 2015KEY ACTION STATEMENTS process, blood glucose (BG) concen- T2DM. Patients in whom ketoacidosis
Key Action Statement 1 trations may be normal much of the is diagnosed require immediate
time and the patient likely will be treatment with insulin and fluid re-
Clinicians must ensure that insulin asymptomatic. At this stage, the dis- placement in an inpatient setting
therapy is initiated for children ease may only be detected by abnor- under the supervision of a physician
and adolescents with T2DM who mal BG concentrations identified who is experienced in treating this
are ketotic or in diabetic ketoaci- during screening. As insulin secretion complication.
dosis and in whom the distinction declines further, the patient is likely to Youth and adolescents who present with
between T1DM and T2DM is unclear; develop symptoms of hyperglycemia, T2DM with poor glycemic control (BG
and, in usual cases, should initiate occasionally with ketosis or frank concentrations ≥250 mg/dL or HbA1c
insulin therapy for patients: ketoacidosis. High glucose concen- >9%) but who lack evidence of ketosis
a. who have random venous or trations can cause a reversible toxic- or ketoacidosis may also benefit from
plasma BG concentrations ity to islet β cells that contributes initial treatment with insulin, at least on
≥250 mg/dL; or further to insulin deficiency. Of ado- a short-term basis.34 This allows for
b. whose HbA1c is >9%. lescents in whom T2DM is subse- quicker restoration of glycemic con-
(Strong Recommendation: evidence quently diagnosed, 5% to 25% present trol and, theoretically, may allow islet
quality X, validating studies cannot with ketoacidosis.34 β cells to “rest and recover.”35,36
be performed, and C, observational Diabetic ketoacidosis must be treated Furthermore, it has been noted that
studies and expert opinion; pre- with insulin and fluid and electrolyte initiation of insulin may increase
ponderance of benefit over harm.) replacement to prevent worsening long-term adherence to treatment
in children and adolescents with
Action Statement Profile KAS 1 T2DM by enhancing the patient’s per-
Aggregate evidence quality X (validating studies cannot be performed)
ception of the seriousness of the dis-
Benefits Avoidance of progression of diabetic ketoacidosis (DKA) and
worsening metabolic acidosis; resolution of acidosis and ease.7,37–40 Many patients with T2DM
hyperglycemia; avoidance of coma and/or death. Quicker can be weaned gradually from insulin
restoration of glycemic control, potentially allowing islet β therapy and subsequently managed
cells to “rest and recover,” increasing long-term adherence
to treatment; avoiding progression to DKA if T1DM. Avoiding with metformin and lifestyle modifica-
hospitalization. Avoidance of potential risks associated with tion.34
the use of other agents (eg, abdominal discomfort, bloating,
loose stools with metformin; possible cardiovascular risks
As noted previously, in some children
with sulfonylureas). and adolescents with newly diagnosed
Harms/risks/cost Potential for hypoglycemia, insulin-induced weight gain, cost, diabetes mellitus, it may be difficult to
patient discomfort from injection, necessity for BG testing,
distinguish between type 1 and type 2
more time required by the health care team for patient
training. disease (eg, an obese child presenting
Benefits-harms assessment Preponderance of benefit over harm. with ketosis).39,41 These patients are
Value judgments Extensive clinical experience of the expert panel was relied on in best managed initially with insulin
making this recommendation.
Role of patient preferences Minimal. therapy while appropriate tests are
Exclusions None. performed to differentiate between
Intentional vagueness None. T1DM and T2DM. The care of chil-
Strength Strong recommendation.
dren and adolescents who have
either newly diagnosed T2DM or
The presentation of T2DM in children metabolic acidosis, coma, and death.
undifferentiated-type diabetes and
and adolescents varies according to Children and adolescents with symp-
who require initial insulin treatment
the disease stage. Early in the disease, toms of hyperglycemia (polyuria,
should be supervised by a physician
before diabetes diagnostic criteria are polydipsia, and polyphagia) who are
experienced in treating diabetic
met, insulin resistance predominates diagnosed with diabetes mellitus
patients with insulin.
with compensatory high insulin se- should be evaluated for ketosis (serum
cretion, resulting in normoglycemia. or urine ketones) and, if positive, for
Over time, β cells lose their ability to ketoacidosis (venous pH), even if their Key Action Statement 2
secrete adequate amounts of insulin phenotype and risk factor status In all other instances, clinicians
to overcome insulin resistance, and (obesity, acanthosis nigricans, positive should initiate a lifestyle modifica-
hyperglycemia results. Early in this family history of T2DM) suggests tion program, including nutrition
370 FROM THE AMERICAN ACADEMY OF PEDIATRICS
Downloaded from pediatrics.aappublications.org by guest on May 15, 2015FROM THE AMERICAN ACADEMY OF PEDIATRICS
and physical activity, and start committee recommends starting the credible RCTs in adolescents with
metformin as first-line therapy drug at a low dose of 500 mg daily, T2DM. The evidence to recommend
for children and adolescents at increasing by 500 mg every 1 to 2 initiating metformin at diagnosis along
the time of diagnosis of T2DM. weeks, up to an ideal and maximum with lifestyle changes comes from 1
dose of 2000 mg daily in divided RCT, several observational studies, and
(Strong recommendation: evidence
doses.41 It should be noted that the consensus recommendations.
quality B; 1 RCT showing improved
main gastrointestinal adverse effects Lifestyle modifications (including nu-
outcomes with metformin versus (abdominal pain, bloating, loose trition interventions and increased
lifestyle; preponderance of bene- stools) present at initiation of met- physical activity) have long been the
fits over harms.) formin often are transient and often cornerstone of therapy for T2DM. Yet,
medical practitioners recognize that
Action Statement Profile KAS 2
effecting these changes is both chal-
Aggregate evidence quality B (1 randomized controlled trial showing improved outcomes
lenging and often accompanied by
with metformin versus lifestyle combined with expert
opinion). regression over time to behaviors not
Benefit Lower HbA1c, target HbA1c sustained longer, less early conducive to maintaining the target
deterioration of BG, less chance of weight gain, improved range of BG concentrations. In pedi-
insulin sensitivity, improved lipid profile.
Harm (of using metformin) Gastrointestinal adverse effects or potential for lactic acidosis atric patients, lifestyle change is most
and vitamin B12 deficiency, cost of medications, cost to likely to be successful when a multi-
administer, need for additional instruction about medication, disciplinary approach is used and the
self-monitoring blood glucose (SMBG), perceived difficulty of
insulin use, possible metabolic deterioration if T1DM is
entire family is involved. (Encourage-
misdiagnosed and treated as T2DM, potential risk of lactic ment of healthy eating and physical
acidosis in the setting of ketosis or significant dehydration. exercise are discussed in Key Action
It should be noted that there have been no cases reported of
vitamin B12 deficiency or lactic acidosis with the use of
Statements 5 and 6.) Unfortunately,
metformin in children. efforts at lifestyle change often fail for
Benefits-harms assessment Preponderance of benefit over harm. a variety of reasons, including high
Value judgments Committee members valued faster achievement of BG control
over not medicating children.
rates of loss to follow-up; a high rate of
Role of patient preferences Moderate; precise implementation recommendations likely will depression in teenagers, which affects
be dictated by patient preferences regarding healthy adherence; and peer pressure to
nutrition, potential medication adverse reaction, exercise,
participate in activities that often
and physical activity.
Exclusions Although the recommendation to start metformin applies to all, center on unhealthy eating.
certain children and adolescents with T2DM will not be able Expert consensus is that fewer than
to tolerate metformin. In addition, certain older or more
debilitated patients with T2DM may be restricted in the 10% of pediatric T2DM patients will at-
amount of moderate-to-vigorous exercise they can perform tain their BG goals through lifestyle
safely. Nevertheless, this recommendation applies to the vast interventions alone.6,35,44 It is possible
majority of children and adolescents with T2DM.
Intentional vagueness None. that the poor long-term success rates
Policy level Strong recommendation. observed from lifestyle interventions
stem from patients’ perception that the
intervention is not important because
Metformin as First-Line Therapy disappear completely if medication is medications are not being prescribed.
Because of the low success rate with continued. Generally, doses higher One might speculate that prescribing
diet and exercise alone in pediatric than 2000 mg daily do not provide medications, particularly insulin ther-
patients diagnosed with T2DM, met- additional therapeutic benefit.34,42,43 In apy, may convey a greater degree of
formin should be initiated along with addition, the use of extended-release concern for the patient’s health and the
the promotion of lifestyle changes, metformin, especially with evening seriousness of the diagnosis, relative to
unless insulin is needed to reverse dosing, may be considered, although that conveyed when medications are
glucose toxicity in the case of signifi- data regarding the frequency of ad- not needed, and that improved treat-
cant hyperglycemia or ketoacidosis verse effects with this preparation are ment adherence and follow-up may
(see Key Action Statement 1). Because scarce. Metformin is generally better result from the use of medication. In-
gastrointestinal adverse effects are tolerated when taken with food. It is deed, 2 prospective observational
common with metformin therapy, the important to recognize the paucity of studies revealed that treatment with
PEDIATRICS Volume 131, Number 2, February 2013 371
Downloaded from pediatrics.aappublications.org by guest on May 15, 2015lifestyle modification alone is associ- Drug Administration (FDA) for use in Insulin offers theoretical benefits
ated with a higher rate of loss to children, both thiazolidinediones and of improved metabolic control
follow-up than that found in patients incretins are occasionally used in while preserving β-cell function or
who receive medication.45 adolescents younger than 18 years.48 even reversing β-cell damage.34,35
Before initiating treatment with met- Metformin is recommended as the Initial use of insulin therapy may
formin, a number of important con- initial pharmacologic agent in ado- convey to the patient a sense of
siderations must be taken into lescents presenting with mild hyper- seriousness of the disease.7,53
account. First, it is important to de- glycemia and without ketonuria or Throughout the writing of these
termine whether the child with a new severe hyperglycemia. In addition to guidelines, the authors have been
diagnosis has T1DM or T2DM, and it is improving hepatic insulin sensitivity,
following the progress of the National
critical to err on the side of caution if metformin has a number of practical
Institute of Diabetes and Digestive and
there is any uncertainty. The 2009 advantages over insulin:
Kidney Diseases–supported Treat-
Clinical Practice Consensus Guidelines Potential weight loss or weight ment Options for type 2 Diabetes in
on Type 2 Diabetes in Children and neutrality.37,48 Adolescents and Youth (TODAY) trial,54
Adolescents from the International Because of a lower risk of hypogly- designed to compare standard (met-
Society for Pediatric and Adolescent cemia, less frequent finger-stick formin alone) therapy versus more
Diabetes provides more information BG measurements are required aggressive therapy as the initial
on the classification of diabetes in with metformin, compared with insu- treatment of youth with recent-onset
children and adolescents with new lin therapy or sulfonylureas.37,42,49–51 T2DM. Since the completion of these
diagnoses.46 If the diagnosis is un- Improves insulin sensitivity and guidelines, results of the TODAY trial
clear (as may be the case when an may normalize menstrual cycles have become available and reveal
obese child with diabetes presents in females with polycystic ovary that metformin alone is inadequate
also with ketosis), the adolescent syndrome. (Because metformin in effecting sustained glycemic con-
must be treated with insulin until the may also improve fertility in trol in the majority of youth with di-
T2DM diagnosis is confirmed.47 Al- patients with polycystic ovary syn- abetes. The study also revealed that
though it is recognized that some the addition of rosiglitazone to met-
drome, contraception is indicated
children with newly diagnosed T2DM formin is superior to metformin
for sexually active patients who wish
may respond to metformin alone, the alone in preserving glycemic control.
to avoid pregnancy.)
committee believes that the presence Direct application of these findings
of either ketosis or ketoacidosis dic- Taking pills does not have the discom- to clinical practice is problematic,
tates an absolute initial requirement fort associated with injections.
however, because rosiglitazone is not
for insulin replacement. (This is Less instruction time is required to FDA-approved for use in children, and
addressed in Key Action Statement 1.) start oral medication, making it is its use, even in adults, is now se-
Although there is little debate that easier for busy practitioners to verely restricted by the FDA because
a child presenting with significant prescribe. of serious adverse effects reported
hyperglycemia and/or ketosis requires Adolescents do not always accept in adults. Thus, the results suggest
insulin, children presenting with more injections, so oral medication that therapy that is more aggressive
modest levels of hyperglycemia (eg, might enhance adherence.52 than metformin monotherapy may be
random BG of 200–249 mg/dL) or required in these adolescents to
Potential advantages of insulin over
asymptomatic T2DM present addi- prevent loss of glycemic control, but
metformin for treatment at diabetes
tional therapeutic challenges to the they do not provide specific guidance
onset include the following:
clinician. In such cases, metformin because it is not known whether the
alone, insulin alone, or metformin Metabolic control may be achieved effect of the additional agent was
with insulin all represent reasonable more rapidly with insulin com- specific to rosiglitazone or would be
options. Additional agents are likely to pared with metformin therapy.37 seen with the addition of other
become reasonable options for initial With appropriate education and tar- agents. Unfortunately, there are lim-
pharmacologic management in the geting the regimen to the individual, ited data for the use of other cur-
near future. Although metformin and adolescents are able to accept and rently available oral or injected
insulin are the only antidiabetic agents use insulin therapy with improved hypoglycemic agents in this age
currently approved by the US Food and metabolic outcomes.53 range, except for insulin. Therefore,
372 FROM THE AMERICAN ACADEMY OF PEDIATRICS
Downloaded from pediatrics.aappublications.org by guest on May 15, 2015FROM THE AMERICAN ACADEMY OF PEDIATRICS
the writing group for these guide- plus-rosiglitazone intervention in main- evaluated the relationship between
lines continues to recommend met- taining glycemic control over time.54 glycemic control and the risk of de-
formin as first-line therapy in this veloping microvascular and/or mac-
Summary
age group but with close monitoring rovascular complications in children
for glycemic deterioration and the As noted previously, metformin is a safe and adolescents with T2DM. A num-
early addition of insulin or another and effective agent for use at the time of ber of studies of children with
pharmacologic agent if needed. diagnosis in conjunction with lifestyle T1DM55–57 and adults with T2DM have,
changes. Although observational studies however, shown a significant relation-
and expert opinion strongly support ship between glycemic control (as
Lifestyle Modification, Including lifestyle changes as a key component of
Nutrition and Physical Activity measured by HbA1c concentration) and
the regimen in addition to metformin, the risk of microvascular complications
Although lifestyle changes are con- randomized trials are needed to de-
(eg, retinopathy, nephropathy, and neu-
sidered indispensable to reaching lineate whether using lifestyle options
ropathy).58,59 The relationship between
treatment goals in diabetes, no sig- alone is a reasonable first step in
HbA1c concentration and risk of mi-
nificant data from RCTs provide in- treating any select subgroups of chil-
crovascular complications appears to
formation on success rates with such dren with T2DM.
be curvilinear; the lower the HbA1c
an approach alone.
Key Action Statement 3 concentration, the lower the downstream
A potential downside for initiating risk of microvascular complications, with
lifestyle changes alone at T2DM onset The committee suggests that clini- the greatest risk reduction seen at the
is potential loss of patients to follow- cians monitor HbA1c concentrations highest HbA1c concentrations.57
up and worse health outcomes. The every 3 months and intensify treat-
value of lifestyle modification in the ment if treatment goals for BG and It is generally recommended that
management of adolescents with HbA1c concentrations are not being HbA1c concentrations be measured
T2DM is likely forthcoming after a more met. (Option: evidence quality D; every 3 months.60 For adults with
detailed analysis of the lifestyle in- expert opinion and studies in chil- T1DM, the American Diabetes Associ-
tervention arm of the multicenter TODAY dren with T1DM and in adults with ation recommends target HbA1c con-
trial becomes available.54 As noted pre- T2DM; preponderance of benefits centrations of less than 7%; the
viously, although it was published after over harms.) American Association of Clinical Endo-
crinologists recommends target con-
Action Statement Profile KAS 3 centrations of less than 6.5%. Although
Aggregate evidence quality D (expert opinion and studies in children with T1DM and in adults with HbA1c target concentrations for children
T2DM; no studies have been performed in children and adolescents and adolescents with T1DM are higher,13
with T2DM). several review articles suggest target
Benefit Diminishing the risk of progression of disease and deterioration
resulting in hospitalization; prevention of microvascular HbA1c concentrations of less than 7%
complications of T2DM. for children and adolescents with
Harm Potential for hypoglycemia from overintensifying treatment to reach T2DM.40,61–63 The committee concurs
HbA1c target goals; cost of frequent testing and medical consultation;
possible patient discomfort. that, ideally, target HbA1c concentration
Benefits-harms assessment Preponderance of benefits over harms. should be less than 7% but notes that
Value judgments Recommendation dictated by widely accepted standards of diabetic care. specific goals must be achievable for the
Role of patient Minimal; recommendation dictated by widely accepted standards of
preferences diabetic care.
individual patient and that this concen-
Exclusions None. tration may not be applicable for all
Intentional vagueness Intentional vagueness in the recommendation as far as setting goals and patients. For patients in whom a target
intensifying treatment attributable to limited evidence.
Policy level Option.
concentration of less than 7% seems
unattainable, individualized goals should
be set, with the ultimate goal of reaching
guideline target concentrations. In addi-
this guideline was developed, the TODAY HbA1c provides a measure of glyce- tion, in the absence of hypoglycemia,
trial indicated that results from the mic control in patients with diabetes even lower HbA1c target concentrations
metformin-plus-lifestyle intervention were mellitus and allows an estimation of can be considered on the basis of an
not significantly different from either the individual’s average BG over the absence of hypoglycemic events and
metformin alone or the metformin- previous 8 to 12 weeks. No RCTs have other individual considerations.
PEDIATRICS Volume 131, Number 2, February 2013 373
Downloaded from pediatrics.aappublications.org by guest on May 15, 2015When concentrations are found to be Glycemic control correlates closely Recognizing that current practices
above the target, therapy should be with the frequency of BG monitoring in may not always reflect optimal care,
intensified whenever possible, with the adolescents with T1DM.64,65 Although a 2004 survey of practices among
goal of bringing the concentration to studies evaluating the efficacy of fre- members of the PES revealed that
target. Intensification activities may quent BG monitoring have not been 36% of pediatric endocrinologists
include, but are not limited to, in- conducted in children and adoles- asked their pediatric patients with
creasing the frequency of clinic visits, cents with T2DM, benefits have been T2DM to monitor BG concentrations
engaging in more frequent BG moni- described in insulin-treated adults twice daily; 12% asked patients to do
toring, adding 1 or more antidiabetic with T2DM who tested their BG 4 times so once daily; 13% asked patients to
agents, meeting with a registered di- per day, compared with adults fol- do so 3 times per day; and 12% asked
etitian and/or diabetes educator, and lowing a less frequent monitoring patients to do so 4 times daily.61 The
increasing attention to diet and exer- regimen.66 These data support the questionnaire provided to the pedi-
cise regimens. Patients whose HbA1c value of BG monitoring in adults atric endocrinologists did not ask
concentrations remain relatively sta- treated with insulin, and likely are about the frequency of BG monitor-
ble may only need to be tested every 6 relevant to youth with T2DM as well, ing in relationship to the diabetes
months. Ideally, real-time HbA1c con- especially those treated with insulin, regimen, however.
centrations should be available at the at the onset of the disease, when Although normoglycemia may be
time of the patient’s visit with the clini- treatment goals are not met, and difficult to achieve in adolescents
cian to allow the physician and patient when the treatment regimen is with T2DM, a fasting BG concentration
and/or parent to discuss intensification changed. The committee believes that of 70 to 130 mg/dL is a reasonable
of therapy during the visit, if needed. current (2011) ADA recommendations target for most. In addition, because
for finger-stick BG monitoring apply to postprandial hyperglycemia has been
Key Action Statement 4 most youth with T2DM67: associated with increased risk of
The committee suggests that clini- Finger-stick BG monitoring should cardiovascular events in adults,
cians advise patients to monitor be performed 3 or more times daily postprandial BG testing may be
finger-stick BG concentrations in for patients using multiple insulin valuable in select patients. BG con-
those who injections or insulin pump therapy. centrations obtained 2 hours after
a. are taking insulin or other For patients using less-frequent in- meals (and paired with pre-meal
sulin injections, noninsulin thera- concentrations) provide an index of
medications with a risk of hy-
pies, or medical nutrition therapy glycemic excursion, and may be
poglycemia; or
b. are initiating or changing their alone, finger-stick BG monitoring useful in improving glycemic control,
may be useful as a guide to the particularly for the patient whose
diabetes treatment regimen; or
success of therapy. fasting plasma glucose is normal but
c. have not met treatment goals; or
whose HbA1c is not at target.68 Rec-
d. have intercurrent illnesses. To achieve postprandial glucose
ognizing the limited evidence for
(Option: evidence quality D; expert targets, postprandial finger-stick
benefit of FSBG testing in this pop-
consensus. Preponderance of ben- BG monitoring may be appropri-
ulation, the committee provides
efits over harms.) ate.
suggested guidance for testing fre-
quency, tailored to the medication
Action Statement Profile KAS 4
regimen, as follows:
Aggregate evidence quality D (expert consensus).
Benefit Potential for improved metabolic control, improved potential for
prevention of hypoglycemia, decreased long-term complications.
Harm Patient discomfort, cost of materials.
BG Testing Frequency for Patients With
Benefits-harms assessment Benefit over harm. Newly Diagnosed T2DM: Fasting,
Value judgments Despite lack of evidence, there were general committee perceptions that Premeal, and Bedtime Testing
patient safety concerns related to insulin use or clinical status
outweighed any risks from monitoring. The committee suggests that all
Role of patient preferences Moderate to low; recommendation driven primarily by safety concerns. patients with newly diagnosed T2DM,
Exclusions None. regardless of prescribed treatment
Intentional vagueness Intentional vagueness in the recommendation about specific
approaches attributable to lack of evidence and the need to plan, should perform finger-stick BG
individualize treatment. monitoring before meals (including
Policy level Option. a morning fasting concentration) and
374 FROM THE AMERICAN ACADEMY OF PEDIATRICS
Downloaded from pediatrics.aappublications.org by guest on May 15, 2015FROM THE AMERICAN ACADEMY OF PEDIATRICS
at bedtime until reasonable metabolic Oral agents: Once treatment goals are a rapid-acting insulin analog is given
control is achieved.69 Once BG con- met, the frequency of monitoring can be for “X” grams of carbohydrates inges-
centrations are at target levels, the decreased; however, the committee ted (see box below). When using this
frequency of monitoring can be mod- recommends some continued BG test- method, the patient must be willing and
ified depending on the medication ing for all youth with T2DM, at a fre- able to count the number of grams of
used, the regimen’s intensity, and the quency determined within the clinical carbohydrates in the meal and divide
patient’s metabolic control. Patients context (e.g. medication regimen, HbA1c, by the assigned “carb ratio (X)” to
who are prone to marked hypergly- willingness of the patient, etc.). For ex- know how many units of insulin should
cemia or hypoglycemia or who are on ample, an infrequent or intermittent be taken. In addition, the patient must
a therapeutic regimen associated with monitoring schedule may be adequate always check BG concentrations before
increased risk of hypoglycemia will when the patient is using exclusively an the meal to determine how much ad-
require continued frequent BG testing. oral agent associated with a low risk of ditional insulin should be given as
Expectations for frequency and timing hypoglycemia and if HbA1c concen- a correction dose using an algorithm
of BG monitoring should be clearly de- trations are in the ideal or non-diabetic assigned by the care team if the fasting
fined through shared goal-setting be- range. A more frequent monitoring BG is not in target. Insulin pumps are
tween the patient and clinician. The schedule should be advised during based on this concept of “basal-bolus”
adolescent and family members should times of illness or if symptoms of hy- insulin administration and have the
be given a written action plan stating perglycemia or hypoglycemia develop. capability of calculating a suggested
the medication regimen, frequency and bolus dosage, based on inputted grams
timing of expected BG monitoring, as Oral agent plus a single injection of of carbohydrates and BG concen-
well as follow-up instructions. a long-acting insulin: Some youth with trations. Because the BG value deter-
T2DM can be managed successfully with mines the amount of insulin to be given
a single injection of long-acting insulin in at each meal, the recommended testing
BG Testing Frequency for Patients on conjunction with an oral agent. Twice a frequency for patients on this regimen
Single Insulin Daily Injections and Oral day BG monitoring (fasting plus a sec- is before every meal.
Agents ond BG concentration – ideally 2-hour
Single bedtime long-acting insulin: post prandial) often is recommended, as
The simplest insulin regimen con- long as HbA1c and BG concentrations Box 1 Example of Basal Bolus
sists of a single injection of long- remain at goal and the patient remains Insulin Regimen
acting insulin at bedtime (basal asymptomatic. If an adolescent has a BG of 250
insulin only). The appropriateness of mg/dL, is to consume a meal
the insulin dose for patients using BG Testing Frequency for Patients containing 60 g of carbohydrates,
this regimen is best defined by the Receiving Multiple Daily Insulin with a carbohydrate ratio of 1:10
fasting/prebreakfast BG test. For Injections (eg, Basal Bolus Regimens): and an assigned correction dose
patients on this insulin regimen, the Premeal and Bedtime Testing of 1:25>125 (with 25 being the
committee suggests daily fasting BG Basal bolus regimens are commonly insulin sensitivity and 125 mg/dL
measurements. This regimen is as- used in children and youth with T1DM the target blood glucose level),
sociated with some risk of hypogly- and may be appropriate for some youth the mealtime bolus dose of
cemia (especially overnight or with T2DM as well. They are the most insulin would be as follows:
fasting hypoglycemia) and may not labor intensive, providing both basal 60 g/10 “carb ratio” =
provide adequate insulin coverage insulin plus bolus doses of short-acting 6 units rapid-acting insulin for
for mealtime ingestions throughout insulin at meals. Basal insulin is pro- meal
the day, as reflected by fasting BG vided through either the use of long-
plus
concentrations in target, but day- acting, relatively peak-free insulin (by
time readings above target. In such needle) or via an insulin pump. Bolus (250–125)/25 = 125/25 =
cases, treatment with meglitinide insulin doses are given at meal-time, 5 units rapid-acting insulin for
(Prandin [Novo Nordisk Pharma- using one of the rapid-acting insulin correction
ceuticals] or Starlix [Novartis Phar- analogs. The bolus dose is calculated by Thus, total bolus insulin coverage
maceuticals]) or a short-acting using a correction algorithm for the at mealtime is: 11 U (6 + 5) of
insulin before meals (see below) premeal BG concentration as well as rapid-acting insulin.
may be beneficial. a “carb ratio,” in which 1 unit of
PEDIATRICS Volume 131, Number 2, February 2013 375
Downloaded from pediatrics.aappublications.org by guest on May 15, 2015Key Action Statement 5 patients with T2DM both at the time agement, summarized below (A
The committee suggests that clini- of diagnosis and as part of ongoing complete list of these recom-
cians incorporate the Academy of management. (Option; evidence mendations is accessible to health
Nutrition and Dietetics’ Pediatric quality D; expert opinion; pre- care professionals at: http://www.
Weight Management Evidence- ponderance of benefits over andevidencelibrary.com/topic.cfm?
Based Nutrition Practice Guide- harms. Role of patient preference cat=4102&auth=1.)
lines in the nutrition counseling of is dominant.) According to the Academy of Nutri-
tion and Dietetics’ guidelines, when
incorporated with lifestyle changes,
Action Statement Profile KAS 5 balanced macronutrient diets at 900
Aggregate evidence quality D (expert opinion). to 1200 kcal per day are associated
Benefit Promotes weight loss; improves insulin sensitivity; contributes
to glycemic control; prevents worsening of disease; facilitates
with both short- and long-term (eg,
a sense of well-being; and improves cardiovascular health. ≥ 1 year) improvements in weight
Harm Costs of nutrition counseling; inadequate reimbursement of status and body composition in
clinicians’ time; lost opportunity costs vis-a-vis time and
resources spent in other counseling activities.
children 6 to 12 years of age.70
Benefits-harms assessment Benefit over harm. These calorie recommendations
Value judgments There is a broad societal agreement on the benefits of dietary are to be incorporated with lifestyle
recommendations.
changes, including increased activ-
Role of patient preference Dominant. Patients may have different preferences for how they
wish to receive assistance in managing their weight-loss ity and possibly medication. Re-
goals. Some patients may prefer a referral to a nutritionist strictions of no less than 1200 kcal
while others might prefer accessing online sources of help.
per day in adolescents 13 to 18
Patient preference should play a significant role in
determining an appropriate weight-loss strategy. years old result in improved weight
Exclusions None. status and body composition as
Intentional vagueness Intentional vagueness in the recommendation about specific
well. 71 The Diabetes Prevention Pro-
approaches attributable to lack of evidence and the need to
individualize treatment. gram demonstrated that partic-
Policy level Option. ipants assigned to the intensive
lifestyle-intervention arm had a re-
duction in daily energy intake of 450
kcal and a 58% reduction in pro-
Consuming more calories than one children and adolescents, because gression to diabetes at the 2.8-year
uses results in weight gain and is the great majority of children with follow-up.71 At the study’s end, 50%
a major contributor to the increasing T2DM are obese or overweight at of the lifestyle-arm participants had
incidence of T2DM in children and diagnosis.26 The committee suggests achieved the goal weight loss of at
adolescents. Current literature is in- that clinicians encourage children least 7% after the 24-week curricu-
conclusive about a single best meal and adolescents with T2DM to follow lum and 38% showed weight loss of
plan for patients with diabetes mel- the Academy of Nutrition and Di- at least 7% at the time of their most
litus, however, and studies specifi- etetics’ recommendations for main- recent visit.72 The Academy of Nutri-
cally addressing the diet of children taining healthy weight to promote tion and Dietetics recommends that
and adolescents with T2DM are health and reduce obesity in this protein-sparing, modified-fast (keto-
limited. Challenges to making rec- population. The committee recom- genic) diets be restricted to children
ommendations stem from the small mends that clinicians refer patients who are >120% of their ideal body
sample size of these studies, limit- to a registered dietitian who has weight and who have a serious
ed specificity for children and expertise in the nutritional needs of medical complication that would
adolescents, and difficulties in gen- youth with T2DM. Clinicians should benefit from rapid weight loss.71
eralizing the data from dietary re- incorporate the Academy of Nutri- Specific recommendations are for
search studies to the general tion and Dietetics’ Pediatric Weight the intervention to be short-term
population. Management Evidence-Based Nutri- (typically 10 weeks) and to be con-
Although evidence is lacking in chil- tion Practice Guidelines, which de- ducted under the supervision of
dren with T2DM, numerous studies scribe effective, evidence-based a multidisciplinary team specializ-
have been conducted in overweight treatment options for weight man- ing in pediatric obesity.
376 FROM THE AMERICAN ACADEMY OF PEDIATRICS
Downloaded from pediatrics.aappublications.org by guest on May 15, 2015You can also read