BIROn - Birkbeck Institutional Research Online
←
→
Page content transcription
If your browser does not render page correctly, please read the page content below
BIROn - Birkbeck Institutional Research Online Oakley, B. and Tillman, J. and Ruigrok, A. and Baranger, A. and Takow, C. and Charman, T. and Jones, Emily J.H. and Cusack, J. and Doherty, M. and Violland, P. and Agnieszka, W. and Simonoff, E. and Buitelaar, J. and Gallagher, L. and Murphy, D. (2021) COVID-19 health and social care access for autistic people: A European policy review. BMJ Open 2021 (11), ISSN 2044-6055. Downloaded from: Usage Guidelines: Please refer to usage guidelines at or alternatively contact lib-eprints@bbk.ac.uk.
Open access Original research
COVID-19 health and social care access
BMJ Open: first published as 10.1136/bmjopen-2020-045341 on 17 May 2021. Downloaded from http://bmjopen.bmj.com/ on July 6, 2021 by guest. Protected by copyright.
for autistic people: European
policy review
Bethany Oakley,1 Julian Tillmann ,2,3 Amber Ruigrok,4 Aurélie Baranger,5
Christian Takow,5 Tony Charman ,2,6 Emily Jones,7 James Cusack,8
Mary Doherty,9 Pierre Violland,5 Agnieszka Wroczyńska,10 Emily Simonoff,11
Jan K Buitelaar,12,13 Louise Gallagher,14 Declan G M Murphy,1,15 AIMS-2-TRIALS
ECRAN & the AIMS-2-TRIALS Consortium
To cite: Oakley B, Tillmann J, ABSTRACT
Ruigrok A, et al. COVID-19 Strengths and limitations of this study
Background The global COVID-19 pandemic has had an
health and social care access unprecedented impact on European health and social care
for autistic people: European ►► Comprehensive review of regional and national pol-
systems, with demands on testing, hospital and intensive
policy review. BMJ Open icies and guidelines on access to COVID-19 health
care capacity exceeding available resources in many
2021;11:e045341. doi:10.1136/ and social care services from 15 European countries.
bmjopen-2020-045341 regions. This has led to concerns that some vulnerable
►► Large- scale survey of the lived experiences of
groups, including autistic people, may be excluded from
►► Prepublication history and
1301 individuals from the autism community, cap-
services.
additional material for this turing real-world COVID-19 health and social care
Methods We reviewed policies from 15 European
paper are available online. To provision.
member states, published in March–July 2020, pertaining
view these files, please visit ►► Synthesis of policy and survey findings in the con-
to (1) access to COVID-19 tests; (2) provisions for
the journal online (http://dx.doi. text of a multi-disciplinary, participatory collabo-
org/10.1136/b mjopen-2020- treatment, hospitalisation and intensive care units (ICUs);
ration, including autistic people, non-profit autism
045341). and (3) changes to standard health and social care. In
stakeholder organisations, clinical experts and re-
parallel, we analysed survey data on the lived experiences
searchers from across Europe.
BO, JT and AR are joint first of 1301 autistic people and caregivers.
►► Nuanced analysis and comparison of regional and
authors. Results Autistic people experienced significant barriers
national service provision is challenging due to vari-
when accessing COVID-19 services. First, despite being at
Received 29 September 2020 ation in health and social care systems and a lack
elevated risk of severe illness due to co-occurring health
Revised 28 January 2021 of available policy or survey data in some European
conditions, there was a lack of accessibility of COVID-19
Accepted 17 February 2021 countries.
testing. Second, many COVID-19 outpatient and inpatient
►► Self-selection of survey respondents and variation
treatment services were reported to be inaccessible,
in the impact of COVID-19 across European coun-
predominantly resulting from individual differences in
tries might have introduced response or publication
communication needs. Third, ICU triage protocols in many
biases that influenced the information available for
European countries (directly or indirectly) resulted in
this study.
discriminatory exclusion from lifesaving treatments. Finally,
interruptions to standard health and social care left over
70% of autistic people without everyday support.
Conclusions The COVID-19 pandemic has further During global viral pandemics and public
exacerbated existing healthcare inequalities for autistic health emergencies, like COVID-19, there
people, probably contributing to disproportionate increases is a significant risk that overwhelming and
in morbidity and mortality, mental health and behavioural sustained demand for healthcare resources
difficulties, and reduced quality of life. An urgent need could exceed the capacity of health-
exists for policies and guidelines on accessibility care systems.2 3 Consequently, mitigation
of COVID-19 services to be updated to prevent the measures to reduce pressure on health and
© Author(s) (or their widespread exclusion of autistic people from services, social care systems have been implemented
employer(s)) 2021. Re-use which represents a violation of international human rights in many regions, including strict national
permitted under CC BY-NC. No law.
commercial re-use. See rights lockdown policies (ie, restrictions on move-
and permissions. Published by ment) to slow virus transmission.4 Neverthe-
BMJ. INTRODUCTION less, within just 1 month of COVID-19 being
For numbered affiliations see Over 26 million SARS- CoV2 infections declared a global pandemic, the European
end of article. (hereafter COVID-19) and 550 000 COVID- Centre for Disease Prevention and Control
Correspondence to 19-
related deaths had been confirmed reported that many EU countries were expe-
Dr Bethany Oakley; in Europe by the close of 2020, making it riencing unprecedented demands on testing
bethany.oakley@k cl.ac.uk one of the worst hit regions worldwide.1 capacity, personal protective equipment
Oakley B, et al. BMJ Open 2021;11:e045341. doi:10.1136/bmjopen-2020-045341 1Open access
(PPE), and hospital and intensive care capacity, far were distributed and implemented within national poli-
BMJ Open: first published as 10.1136/bmjopen-2020-045341 on 17 May 2021. Downloaded from http://bmjopen.bmj.com/ on July 6, 2021 by guest. Protected by copyright.
exceeding available resources.5 In such situations, cies across Europe to safeguard autistic people is unclear.
disparities in healthcare access are magnified, leading We collated and reviewed regional or national poli-
to concerns that some groups of individuals, including cies and guidelines from 15 European member states,
autistic people, might be particularly vulnerable to covering three priority areas: (1) access to COVID-19
being excluded from services, support and treatment in testing and screening; (2) provisions for treatment, hospi-
pandemic situations.6 talisation and access to intensive care units (ICUs); and
Reports from the United States during the first global (3) access to standard health and social care. We consid-
peak of COVID-19 infection indicated inequalities in ered whether current guidelines (directly or indirectly)
access to COVID-19 services, with one study highlighting discriminate against (or are protective of) autistic people.
that 27 states had adopted ‘healthcare rationing’ policies Furthermore, to capture lived experiences of COVID-19
that could harm autistic people and those with disabil- health and social care provision at the level of the indi-
ities (including intellectual disability).7 Furthermore, vidual, Autism-Europe provided secondary data from a
COVID-19 may disproportionately impact autistic people large-scale survey of autistic people and caregivers.
(who represent at least 1% of European citizens and
at least 32% of whom have a co-occurring intellectual
disability)8 9 due to elevated physical health comorbidi-
ties and existing healthcare inequalities. For example, METHODS
physical health conditions are experienced at substan- Study design
tially higher rates by autistic people compared with the AIMS-2-TRIALS is an international public–private part-
general population, including conditions associated with nership that brings together autistic people and their
high risk of severe illness from COVID-19 (eg, cardiovas- families, researchers and clinicians, charities, industry and
cular or immune conditions, diabetes, obesity).10–12 In pharmaceutical companies to improve understanding of
addition, autistic people experience numerous existing autism and enhance treatment options for autistic people
barriers to accessing general healthcare,13 which may (https://www.aims-2-trials.eu/). To assess COVID-19
also increase their risk of being excluded from COVID-19 health and social care provision for autistic people,
services. These barriers include communication or inter- according to the priority areas described above, a two-
pretation difficulties, which can lead to misunderstand- step methodological approach was implemented. First,
ings by healthcare providers and reduced involvement COVID-19 health and social care policies from 15 Euro-
of patients in healthcare decision making (and might be pean countries were collated and reviewed by researchers,
exacerbated by mask wearing, which reduces the avail- clinicians and non-profit groups from the AIMS-2-TRIALS
ability of non-verbal facial cues during interaction); diffi- Clinical Trials and Early Career Researchers in Autism
culties adjusting to change and novel procedures; sensory Networks, and a panel of five representatives from the
sensitivities (eg, around physical examinations, mask autism community.
wearing); difficulties identifying or describing pains and Second, Autism- Europe provided de- identified
symptoms; and inconsistent specialist clinician training, secondary data from their large-scale survey of the impact
awareness and knowledge about autism and intellectual of COVID-19 on 1301 autistic people and caregivers. An
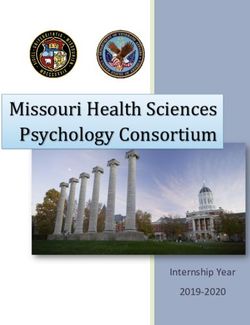
disability.13–15 Health providers might also misattribute overview of the European countries represented in this
COVID-19 symptoms to existing medical, mental health review is presented in figure 1 and Autism-Europe respon-
or behavioural problems, or autism itself (‘diagnostic dent characteristics in online supplemental table 1.
overshadowing’), increasing the risk of severe disease due
to missed or late diagnosis.16 Materials and procedures
Difficulties and delays in accessing COVID-19 services Review of European COVID-19 policy and guidelines
may partly explain why the UK death rate of people with COVID-19-related policies and guidelines from 15 Euro-
intellectual disability (some of whom are also autistic) pean countries (figure 1) were assessed using a common
increased by 134% in the period from mid-April to May review template (please see online supplemental material
2019 compared with 2020, notably higher than in the 1), indexing three priority areas: access to testing and
total population, where deaths increased by 80%.17 18 screening; access to treatment, hospital and intensive
Additionally, at least 40–60% of confirmed deaths from care resources; and changes to existing health and social
COVID-19 across European countries with community care. To be included, policies and guidelines had to be
transmission are believed to have occurred in long-term publicly available (ie, online/open access) and published
care facilities,19 a proportion of which offer residential between March and July 2020. A full list of included docu-
care for autistic people. Of further concern, although ments is provided in online supplemental table 2, with
guidelines around COVID-19 management and intellec- source of access specified.
tual disability were released by the World Health Orga- Policies and guidelines were collated and translated
nization in March 202020 and more detailed information into English by a panel of 30 AIMS-2-TRIALS early career
has since been published by charities and clinical research autism researchers and five representatives from the
teams,21–23 the extent to which these recommendations autism community. In addition, documents were reviewed
2 Oakley B, et al. BMJ Open 2021;11:e045341. doi:10.1136/bmjopen-2020-045341Open access
written permission for the publication of their anony-
BMJ Open: first published as 10.1136/bmjopen-2020-045341 on 17 May 2021. Downloaded from http://bmjopen.bmj.com/ on July 6, 2021 by guest. Protected by copyright.
mised quotations, which were included for illustrative
purposes.
Public and patient involvement
Representatives from the autism community, and chari-
ties Autism-Europe and Autistica, were involved as active
research partners in all aspects of the research through
identifying priority areas for policy review, collating and
reviewing policy guidelines in selected countries, inter-
preting findings, making recommendations for policy
guidance, and editing or co-authoring the manuscript.
Autism- Europe independently designed the survey
content and collated all responses.
Figure 1 Schematic highlighting the 15 European countries
included in this study, colour coded by number of Autism-
Europe survey responses from each region: Spain, n=304; RESULTS
Italy, n=192; Greece, n=165; the Netherlands, n=143; Review of European COVID-19 policy or guidelines (March–
Switzerland, n=144; France, n=86; United Kingdom, n=66; July 2020)
Germany, n=60; Malta, n=53; Belgium, n=34; Luxembourg, Accessibility of COVID-19 testing and screening
n=33; Austria, n=12; Ireland, n=5; Poland, n=3; Portugal, n=1.
First, we considered guidance on access to COVID-19 tests,
particularly in the context of testing shortages. As explic-
itly acknowledged in documentation released by several
by clinicians with extensive experience in autism diagnosis European regions reviewed in this study—including the
and intervention, who provided expert commentary. UK, the Netherlands and Belgium24–26—those with rele-
vant physical comorbidities and/or living in residential
Lived experiences from the autism community care meet criteria for priority COVID-19 testing. This
As noted in the Introduction, where specific guidance has guidance is relevant for autistic people, given a high
been published, the extent to which recommendations proportion experience physical health comorbidities that
for supporting autistic people and those with intellectual are associated with increased risk of developing severe
disability have been implemented in everyday practice disease on contracting COVID-19, including cardiovas-
is unclear. Thus, alongside our policy review, Autism- cular or respiratory illness, autoimmune conditions,
Europe (an international, non- profit organisation: diabetes, obesity and hypertension.
https://www.autismeurope.org/) also provided de-iden- Second, approximately 5–25% of autistic people live
tified secondary data from their independent, large-scale in residential care (ie, higher intensity nursing or large
survey of experiences of the COVID-19 pandemic from group homes) and up to a further 27% in supported
the autism community. accommodation (ie, lower intensity congregate care
For the purposes of this review, we included Autism- settings in the community), with upper bound esti-
Europe survey responses from the 15 countries for which mates referring to those with co-occurring intellectual
we also had access to published policy or guidelines. We disability.27 This is notable because the transmission rate
excluded respondents who were not autistic, or relatives/ of COVID-19 in residential care settings is high due to
caregivers (as the identity of ‘other’ respondents were factors such as care staff interacting with multiple resi-
not clearly defined), and those who opened but did not dents throughout the day; global shortages of PPE and
answer survey questions. This resulted in a final conve- testing for care staff; difficulties for some individuals
nience sample of 1301: 346 autistic people and 955 care- with strict adherence to personal hygiene practices; and
givers. Please see online supplemental table 1 for survey impracticalities of maintaining physical distancing (eg, if
demographics. residents require personal care).28 29
Survey items requested from Autism- Europe for the Despite existing evidence of increased risk of poor
purpose of this review are documented in online supple- outcomes from COVID-19 for autistic people, our review
mental table 3. The survey was disseminated publicly indicated that they have not been routinely specified for
online between 7 April and 31 May 2020, in 10 languages, priority access to testing across Europe. For instance,
with participants recruited via Autism-Europe, UK autism early in the COVID-19 pandemic, many regions with
charities and social media. Administration of the survey testing shortages initially prioritised essential workers
was conducted under the ‘Rights, Equality and Citizen- and those hospitalised with suspected COVID-19 symp-
ship programme 2014–2020’, funded by the European toms.30 In the UK and Ireland, care home residents
Commission. Respondents were notified of the Autism- (including those who were asymptomatic) were not offi-
Europe GDPR policy that responses would be used for cially added to the list for priority access to COVID-19
the development of policy recommendations, and gave testing until 29 and 17 April 2020, respectively, at least
Oakley B, et al. BMJ Open 2021;11:e045341. doi:10.1136/bmjopen-2020-045341 3Open access
2 months after the first confirmed COVID-19 cases in Access to intensive care
BMJ Open: first published as 10.1136/bmjopen-2020-045341 on 17 May 2021. Downloaded from http://bmjopen.bmj.com/ on July 6, 2021 by guest. Protected by copyright.
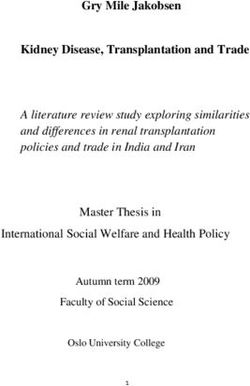
these regions.26 31 Similarly, other countries that did not Our review indicated that—where officially docu-
initially identify individuals in residential care settings mented—interpretation of ICU triage protocols and poli-
as priority for testing, including the Netherlands and cies could pose a barrier to equitable care and access to
Belgium,24 25 now prioritise these groups; the Nether- lifesaving treatments (please see table 1).
lands is the only country to directly prioritise individuals For example, several European countries with
with serious behavioural problems in residential care for published triage protocols recommend the consideration
testing. of ‘functional status’ and/or the use of ‘frailty assess-
However, we did not identify any additional published ments’, including the UK, Ireland, France, the Nether-
guidance, or strategies specifically for enhancing accessi- lands, Italy, Belgium, Austria and Germany.39–47 These
bility of testing for autistic people across any other country assessments were originally designed with reference to
reviewed in this study. For instance, even in the countries elderly populations to determine individuals with very
identified above where individuals with certain physical poor prognosis for recovery from their current illness.48
comorbidities and those living in ‘high risk’ settings were Despite this, concerns have been raised over ambiguity in
prioritised for access to testing in case of shortages, there some current guidance on the application and interpre-
was no guidance published for those living in supported tation of frailty assessments, whereby the support needs of
accommodation and the community. A lack of guidance some autistic people may be conflated with ‘frailty’.37 49 50
was also identified for enhancing the tolerability (and As an example, frailty assessments refer to an individual’s
thus accessibility) of test procedures for autistic people. dependency on others for support with daily care needs
For example, sensory sensitivities and difficulties around and personal care. Similarly, the assessment of functional
uncertainty and changes in routine are highly associated status often includes quality of life outcomes, which are
with autism,32 33 and COVID-19 diagnostic tests frequently known to vary considerably among autistic people but
involve nasal and throat swabs or aspiration,34 use of may also be broadly underestimated because of a reliance
necessary PPE (a potential sensory and communication on ‘neurotypical’ indicators of well-being.51
barrier), long waiting times and travel to an unfamiliar In light of these concerns—and in response to chal-
location—sometimes without the option to be accompa- lenges by advocacy groups and a proposed judicial
nied by a caregiver. review52 53—on 25 March 2020, the UK National Institute
for Health and Care Excellence amended their recom-
mendations to specify that frailty assessments should not
Access to treatment or hospitalisation
be used for younger people or autistic people and those
Next, we reviewed current recommendations for the treat-
with intellectual disability.54 55 They also added weblinks
ment and admission to hospital of autistic people who
to ethical guidance from medical associations (9 April
have COVID-19. Findings first highlighted that guidance
2020) and stated that—where they are appropriate—
from several European countries, including Belgium, Italy frailty assessments should be recorded in the patient’s
and the Netherlands, currently recommends that autistic medical record for transparency (29 April 2020). Similar
people and those with behavioural problems are treated clarifications on the lack of suitability of frailty assessment
for COVID-19 within existing designated specialist neuro- for those with intellectual disability have been published
developmental or neuropsychiatric pathways, rather than in the Netherlands.56 57 Nevertheless, such measures
general hospital settings.35 36 to prevent the misapplication of frailty assessments to
This approach may have some benefit in access to autistic people have not been implemented systematically
a greater range of specialist staff and resources to across European countries.
adequately support individuals with additional needs, Moreover, the Working Group of Bioethics of the
as well as providing more flexibility around some regu- Spanish Society of Intensive, Critical Medicine and Coro-
lations (eg, allowing visitation by a caregiver or support nary Units published triage guidance that explicitly speci-
person, with appropriate hygiene measures in place). fies ‘severe baseline cognitive impairment’ as an exclusion
Nevertheless, in an open letter to EU leaders, the criterion for ICU care.58 This recommendation is based
European Disability Forum specifically recommended on previous advice published in 2010 by the European
that ‘persons with disabilities should not be segregated Society of Intensive Care Medicine Task Force for ICU
into separate facilities, where healthcare for COVID-19 triage during an influenza epidemic, further specifying
is often of a lower standard’.37 Examples of concerns the exclusion of ‘a patient who is unable to perform activ-
about COVID-19 care provision in neurodevelopmental ities of daily living due to cognitive impairment or is insti-
or psychiatric pathways include shortages of staff with tutionalised due to cognitive impairment’.59 60 Similar
medical or surgical and psychiatric expertise and expe- guidance from the COVID-19 Paris region recommends
rience. In addition, there are challenges for controlling attention to a patient’s previous condition, including
infection spread in neurodevelopmental or psychiatric neurocognitive status—mildly or severely impaired cogni-
inpatient settings due to factors like close contact between tive functions.44
patients and care providers and shortages of PPE, for These criteria (and ambiguity in their intended appli-
which general hospitals may be prioritised.38 cation to real-world clinical practice) plainly increase the
4 Oakley B, et al. BMJ Open 2021;11:e045341. doi:10.1136/bmjopen-2020-045341Table 1 COVID-19 triage ethical guidance, published per country, with description of references to frailty, disability, equity and other relevant information
Austria Belgium France Germany Greece Ireland Italy
44
Source(s) Secretariat of Belgian Society of Azoulay et al ; German WHO Regional Office Department of Health Italian Society
the Bioethics Emergency and Disaster Comité Consultatif Interdisciplinary for Europe of Anaesthesia,
Commission, Vienna; Medicine and the Belgian National d'Ethique Association for Analgesia,
Austrian Society for Resuscitation Council; Intensive Care and Resuscitation and
Anaesthesiology, Ethical Committee Care Emergency Medicine Intensive Care
Resuscitation and UZ Leuven
Intensive Care
Date of 31 March 2020; 22 March 2020; 17 March 5 June 2020; 13 17 April 2020 August 2017* 27 March 2020 16 March 2020
publication 17 March 2020 2020 March 2020
‘Frailty’ ►► Short-term ►► Short-term prognosis ►► Baseline ►► Short-term ►► No unified national ►► Short-term ►► Short-term
prognosis using and ‘good functional condition and prognosis and triage system prognosis and prognosis, life
clinical risk outcome’ using frailty score clinical frailty premorbid expectancy and
assessment clinical frailty scale (COVID-19 scale (COVID-19 and long-term functional status
(COVID-19 (severe comorbidity, severity, age, severity, functional health ►► ‘Clinical suitability’
Oakley B, et al. BMJ Open 2021;11:e045341. doi:10.1136/bmjopen-2020-045341
severity, chronic chronic low quality of comorbidities, comorbidities status (COVID-19 (COVID-19
disease/ life, reduced cognition neurocognitive if relevant to severity, severity,
comorbidity, in elderly patients) status) current illness) comorbidities, comorbidities)
physical reserves) frailty independent
of age)
Disability ►► Special support/ ►► None ►► Notes that ►► No exclusion ►► No unified national ►► None (though ►► None
resources for prioritising on the basis triage system no single factor
those with greater life of underlying should be used as
disability to ensure expectancy illnesses/ exclusion criteria)
equal access and could negatively disabilities
life chances impact those
with disabilities
Equity ►► No exclusion ►► Each individual should ►► Value of each ►► All individuals ►► No unified national ►► Recognises the ►► Allocation criteria
based on non- have access to same individual considered triage system moral equality of apply to all
medical criteria current standard recognised as equally and all people intensive care
(including age, of care or ‘the best absolute according to ►► Equal access patients
quality of life) possible spread … to same criteria to/chance of
the maximum amount benefiting from
of people’ healthcare
Continued
Open access
5
BMJ Open: first published as 10.1136/bmjopen-2020-045341 on 17 May 2021. Downloaded from http://bmjopen.bmj.com/ on July 6, 2021 by guest. Protected by copyright.6
Table 1 Continued
Austria Belgium France Germany Greece Ireland Italy
Open access
Other ►► Consider the will ►► Consider the will of ►► Consider the will ►► Consider the will ►► No unified national ►► Consider the will of ►► Consider the will of
of the individual the individual of the individual of the individual triage system the individual the individual
►► Transparency ►► Transparency in ►► Transparency ►► Transparency ►► Transparency ►► Transparency to
in documenting documenting decision in documenting to patients in to patients and patients in decision
decision making making decision making decision making in documenting making
►► Involve local ethics ►► Triage informed by ►► Recommends ►► Involve local decision making ►► Second opinion
advisory service expert team strategies ethics advisory ►► Involve useful for difficult
to reduce service stakeholders in cases
stigmatisation preparedness ►► Flexible/eligible for
of groups planning local adaptation
facing social
inequalities
►► Involve local
ethics advisory
service
Luxembourg The Netherlands Poland Portugal Spain Switzerland UK
Source Commission Royal Dutch Medical Polish Society of National Council of Spanish Society of Swiss Academy of National Institute
Nationale d’Éthique Association Anaesthesiology Ethics for the Life Intensive Critical Medical Sciences for Health and Care
and Intensive Sciences Medicine and Excellence; British
Therapy Coronary Units Medical Association;
Royal College of
Physicians
Date of 31 March 2020 16 June 2020 October 2012* 3 April 2020 21 March 2020 24 March 2020 29 April 2020; April
publication 2020; 2 April 2020
Frailty ►► Short/medium ►► Short-term prognosis ►► Short-term ►► None ►► Short-term ►► Short-term ►► Short-term
term prognosis, with clinical frailty prognosis prognosis prognosis and prognosis with
general health score (including ►► Chronic, severe, ►► Chronic, severe, perceived benefit clinical frailty score
recovery time) but end-of-life end-of-life of intensive care (comorbidities,
do not exclude ID/ comorbid illness comorbid illness ►► Chronic, severe, benefit vs risk,
physical disability end-of-life quality of life) but
based on daily comorbid illness should not be
support needs used for younger
people, those with
stable/chronic
disabilities, autism/
ID
Continued
Oakley B, et al. BMJ Open 2021;11:e045341. doi:10.1136/bmjopen-2020-045341
BMJ Open: first published as 10.1136/bmjopen-2020-045341 on 17 May 2021. Downloaded from http://bmjopen.bmj.com/ on July 6, 2021 by guest. Protected by copyright.Table 1 Continued
Austria Belgium France Germany Greece Ireland Italy
Disability ►► Discrimination ►► Creating capacity ►► None ►► ‘Special ►► Exclude ‘severe ►► Discrimination ►► Duty to not
based on disability for care in attention’ to baseline cognitive based on chronic disadvantage
absolutely neurodevelopmental/ vulnerable groups impairment’ disability precluded one group
prohibited residential care ►► Avoid inequalities disproportionately
settings in access to (eg, disability)
►► Should not consider diagnostics/ ►► Caution indirect
‘mental/physical treatments discrimination,
limitation’, or prior (eg, for those for example,
quality of life with chronic ‘first come first
conditions) served’/‘capacity
to benefit quickly’
may disadvantage
those with
disabilities
Equity ►► No exclusion ►► Allocation criteria ►► None ►► Value of each ►► Selection criteria ►► Equity crucial ►► Each individual
based on non- apply to all intensive individual must be equitably as recognised matters equally;
Oakley B, et al. BMJ Open 2021;11:e045341. doi:10.1136/bmjopen-2020-045341
medical criteria care patients recognised as applied for all who principle of equal chance
►► Value of each absolute would benefit from medical ethics of benefiting
individual ICU from resources
recognised as should mean
absolute equal chance of
►► All patients treated receiving them
fairly and equally
Other ►► Consider the will ►► Transparency to ►► Focus on order ►► Transparency to ►► Consider the will ►► Consider the will of ►► Consider the will of
of the individual patients and in of medical patients and the of the individual the individual the individual
►► Transparency documenting decision prioritisation, public in decision ►► Transparency ►► Transparency ►► Transparency
to patients and making rather than making to patients and in documenting to patients and
in documenting ►► ‘The right care in inclusion/ ►► Remove in documenting decision making in documenting
decision making the right place’ exclusion criteria decision making decision making ►► Triage informed by decision making
►► Involve local ethics (eg, consider home responsibility ►► Involve local ethics expert team ►► Involve local ethics
advisory service treatment) from individual advisory service advisory service
►► Triage informed by care providers ►► Exclude those who ►► Flexibility in
expert team ►► Case-by-case need resources adaptable
decision making that cannot be circumstances
provided
Malta is not included because no publicly available triage recommendations or documentation were identified.
*Current COVID-19 specific triage protocols were not identified, however existing information was available about allocation of resources in the case of shortages.
ID, intellectual disability.
Open access
7
BMJ Open: first published as 10.1136/bmjopen-2020-045341 on 17 May 2021. Downloaded from http://bmjopen.bmj.com/ on July 6, 2021 by guest. Protected by copyright.Open access
potential for discriminatory exclusion of autistic people, Finally, for those receiving community-based care, we
BMJ Open: first published as 10.1136/bmjopen-2020-045341 on 17 May 2021. Downloaded from http://bmjopen.bmj.com/ on July 6, 2021 by guest. Protected by copyright.
especially those with co-occurring intellectual disability, also identified evidence from the UK of ‘easements’ to
and are incompatible with international human rights publicly funded adult social care in response to COVID-
laws (also emphasised by Spanish reports61 62); yet, they 19.73 These easements were introduced to relieve pressure
may be informing clinical decision making.63 on social care services and assist with prioritising support
for those in highest need, by reducing the duty to carry
Access to existing health and social care services out detailed assessments of individual care and support
Overall, our review would suggest that the impact of or financial needs, and reducing the duty to prepare or
COVID-19 has emphasised longstanding pressures on review individual care and support plans. We identified
health and social care systems across Europe and pre- no published evidence to date that any local authorities
existing healthcare inequalities for autistic people. The in England have yet exercised social care easements.74
first trend observed across all regions reviewed has been Nevertheless, it is essential that this situation continues to
the abrupt interruption of usual social support and inter- be closely monitored to ensure that those in need receive
vention services to prevent infection spread. While an adequate support, particularly given the significant lack
important safety precaution, without appropriate mitiga- of reliable data gathered on community-based health and
tion measures in place, for some individuals, services have social care provision across Europe.75
ceased altogether.64
Usual health and social care services for autistic people Lived experiences from the autism community (April–May
have been particularly impacted in three key areas. First, 2020)
many services were already stretched in non-pandemic Accessibility of COVID-19 testing and screening
times, including autism diagnostic services, for which Corresponding to findings from our policy review—
average waiting times can be well over a year (a maximum detailed above—the results from Autism-Europe’s survey
of 13 weeks is recommended by the UK National Insti- of autistic people and caregivers (see table 2) also indi-
tute for Health and Care Excellence).65 Considered ‘non- cated that despite being considered at increased risk of
essential’ in light of the COVID-19 pandemic, cancelled poor outcomes from COVID-19, there was a lack of acces-
or postponed diagnostic appointments may further delay sibility to COVID-19 testing.
autistic people accessing needs-based support (eg, mental For instance, 26% (n=327) of autistic people repre-
health interventions), which could be contingent on sented in Autism-Europe’s survey were reported to be
receiving a formal diagnosis. considered at high risk from COVID-19. Nevertheless,
Second, many community-based services across Europe of the 5% of autistic people who accessed a COVID-19
(eg, day services, workshops, supported employment) are test, 25% (n=13) felt they did not receive, or were unsure
provided by the private sector and non-profit organisa- whether they had received, adequate accessible informa-
tions. These organisations have reported experiencing tion about the test procedure (table 2). Furthermore,
acute financial instability due to COVID-1966 and are only 39% (n=22) were provided with autism- specific
not always eligible to claim reimbursement for appoint- reasonable adjustments (eg, allowed to be accompanied
ments that have been shifted to online delivery (though by a support person; tested in a quiet space). These issues
see flexible legislation from Belgium),67 meaning some were particularly emphasised by the report of one parent
have been forced to close completely.68 As a result, for of a child with autism, who commented:
some autistic people, relatives and other caregivers are I wanted to get my son tested but there was no way
currently the only available support people. to get this done without sedating him. This was not
For those living in residential care settings, with low provided by the doctors and it was such a traumatic
capacity for testing and PPE provisions, restrictions have experience ended up [sic] not doing the test after 1.5
been imposed on visitation from relatives or other care- hours of trying and quarantined instead for 2 weeks.
givers. These restrictions may include a complete ban on
visitation, limits on the number of visitors and/or time
limits on visitation.35 69–71 These measures are designed Access to treatment, hospitalisation and intensive care
to prevent infection spread in ‘high risk’ long-term care Additionally, survey data showed that a proportion of
facilities. However, loss of contact with relatives or care- autistic people also experienced difficulties accessing
givers (also constituting a change in routine) could cause COVID-19 outpatient and inpatient treatment services.
distress for autistic people and increase uncertainty and Of the 2% (n=28) of autistic people captured by
loneliness. Consequently, necessary restrictions on visi- Autism-Europe’s survey who required COVID-19 treat-
tation to residential care settings must be balanced with ment, around half reported access difficulties (n=12),
flexible options for alternative communication, such mostly accounted for by inaccessibility of the process
as regular and consistent access to video or telephone of contacting healthcare providers (n=9; for example,
contact72—though it should be acknowledged that contact by telephone was required):
these options are not sufficient or appropriate for all Similarly, communication difficulties can represent a
individuals. major barrier for receiving quality inpatient treatment
8 Oakley B, et al. BMJ Open 2021;11:e045341. doi:10.1136/bmjopen-2020-045341Open access
Table 2 Autism-Europe survey responses for access to COVID-19 health and social care services for people with autism.
BMJ Open: first published as 10.1136/bmjopen-2020-045341 on 17 May 2021. Downloaded from http://bmjopen.bmj.com/ on July 6, 2021 by guest. Protected by copyright.
Data are numbers (%)
Overall response Autistic person response Caregiver response
Yes No Unsure Yes No Unsure Yes No Unsure
High COVID-19 risk (autistic 327 795 133 90 213 33 237 582 100
person) (26) (63) (11) (27) (63) (10) (26) (63) (11)
Tested for COVID-19 56 1095 1 13 295 0 43 800 1
(5) (95) (0) (4) (96) (0) (5) (95) (0)
Accessible information—COVID-19 40 10 3 7 4 1 33 6 2
test (76) (19) (6) (58) (33) (8) (80) (15) (5)
Reasonable adjustments— 22 31 4 6 11 3 16 20 1
COVID-19 test (39) (54) (7) (30) (55) (15) (43) (54) (3)
Required COVID-19 treatment 28 1112 13 7 296 5 21 816 8
(2) (96) (1) (2) (96) (2) (2) (97) (1)
Difficulties accessing treatment 12 15 1 5 2 0 7 13 1
(43) (54) (4) (71) (29) (0) (33) (62) (5)
Difficulties contacting treatment 9 3 0 3 2 0 (0%) 6 1 0
provider (75) (25) (0) (60) (40) (86) (14) (0)
Require daily or occasional 882 398 21 184 146 16 698 252 5
support (68) (31) (2) (53) (42) (5) (73) (26) (1)
Usual daily support stopped 595 211 31 73 84 17 522 127 14
(71) (25) (4) (42) (48) (10) (79) (19) (2)
High COVID-19 risk (support 279 409 149 50 94 30 229 315 119
person) (33) (49) (18) (29) (54) (17) (35) (48) (18)
Second support person available 247 523 67 44 107 23 203 416 44
(30) (63) (8) (25) (61) (13) (31) (63) (7)
Accessible information—COVID-19 421 557 234 119 117 94 302 440 140
public health (35) (46) (19) (36) (35) (28) (34) (50) (16)
in general hospital settings, as noted by one person with survey respondents being unaware or unsure of accessible
autism: information about current COVID-19 measures.
I had to be hospitalised with acute abdominal cramps.
Access to existing health and social care services
On the spot, the nursing staff took my temperature
Finally, reflecting the impact of the abrupt interrup-
and, worried, they did not know what to do: whether
tion of usual social support and intervention services on
to put me in a separate room, because I could have
autistic people, 71% (n=595) of Autism-Europe survey
COVID-19, or not. I was in the Emergency Room
respondents included in this review indicated that their
for 6 hours, the doctors deliberated my case, and in
usual support services had been stopped due to COVID-
the end I was not tested. During the whole process,
19. This is notable given that approximately one third of
I was mute, paralysed. So I wonder if there is a way
those surveyed indicated that they required daily support
to communicate with the medical professionals about
(35%; n=451) and one third required occasional support
everyone’s situation without adding to the medical
with daily life activities (33%; n=431).
professionals' workload.
In addition, 33% (n=279) of Autism- Europe survey
Moreover, concerns regarding inequalities in access to respondents stated that their usual support person was
COVID-19 services could pose a barrier for seeking treat- also at increased risk of COVID-19% and 63% (n=523)
ment, with one autistic Autism-Europe survey respondent reported they did not have access to another support
revealing: person if their usual caregiver became infected.
I am also afraid that as a mentally impaired [sic] re-
cipient of a disability pension, during possible triage
DISCUSSION
I will be rated worse than those capable of working of
Summary of key findings and recommendations
the same age (ableism) should there be shortages of
We reviewed COVID-19 health and social care access for
medical care.
autistic people across 15 European member states, based
This comment highlights the importance of ensuring on published policies or guidelines and results from a
that public health information is made accessible for the large-scale survey of over 1300 autistic people and care-
autism community, with 65% (n=791) of Autism-Europe givers. Our findings highlighted several issues regarding
Oakley B, et al. BMJ Open 2021;11:e045341. doi:10.1136/bmjopen-2020-045341 9Open access
COVID-19 service access for autistic people that require
Box 1 Recommendations for an aligned European
BMJ Open: first published as 10.1136/bmjopen-2020-045341 on 17 May 2021. Downloaded from http://bmjopen.bmj.com/ on July 6, 2021 by guest. Protected by copyright.
rapid consideration, in terms of testing and screening;
strategy for reducing inequalities in access to health and
accessibility of treatment, hospitalisation and ICU care;
social care services for autistic people and those with
and changes to standard health and social care provision.
intellectual disability in pandemic situations
Specifically, we identified (1) failure to prioritise and
provide adequate adaptations to promote access to testing, Policy recommendations
despite elevated risk of severe COVID-19 disease due to 1. Policy documentation should explicitly outline strategies for promot-
commonly co- occurring physical health problems; (2) ing equitable access to testing and screening for autistic people,
barriers for accessing treatment and hospitalisation (eg, including clinical guidance on identifying symptoms (given evidence
alternative communication needs) and ICU triage proto- for atypical symptom presentation, diagnostic overshadowing and
cols that directly or indirectly (ie, through their ambi- high comorbidity burden), providing accessible inpatient and out-
guity) discriminate against those with additional needs; patient care and enhancing the accessibility of testing procedures
by providing preparatory materials and considering flexible test
and (3) abrupt interruptions to existing service provision
procedures (eg, saliva vs swab testing). Autistic people with phys-
(eg, mental health or community-based services) without ical health comorbidities and those living in ‘high risk’ settings for
appropriate mitigation measures, further exacerbated by disease transmission, such as residential care and supported ac-
longstanding pressures on health and social care. Consid- commodation, should be considered for priority access to proactive
ering these issues, we formulated a set of recommenda- testing and screening, even when apparently asymptomatic.
tions for policy and clinical practice to improve health 2. If hospital admission is necessary, autistic people should receive
and social care access for autistic people in pandemic the necessary accommodations and support to facilitate access to
situations and other public health emergencies (box 1). the same resources and standard of care as other individuals. This
support may include the development of consistent policies to en-
sure: accessible information and communication methods; frequent
Enhancing accessibility of COVID-19 testing and screening consultation between the individual, their families (if appropriate)
As outlined above, our first key finding was a failure to and care provider(s); formal guidance and training to support care
prioritise and systematically provide adequate adapta- providers from all specialities; greater flexibility in care provision.
tions to promote access to testing for autistic people. 3. Triage protocols across Europe require urgent review and update,
COVID-19 strategies published by the World Health in consultation with stakeholders (eg, intensive care and autism
Organization and European Commission emphasise communities), to inform an aligned European strategy on the fair
the critical importance of testing people with suspected allocation of resources in public health emergencies that does not
COVID-19 so that people with confirmed infection can explicitly or inadvertently discriminate against any individual or
groups of individuals on the grounds of pre-existing characteristics
be isolated and their close contacts traced.76 77 COVID-19
or difficulties.
testing strategies and capacity have varied among Euro- 4. The impact of COVID-19 on health and social care service provi-
pean countries. However, broadly, infrastructure limita- sion should be comprehensively reviewed to inform mitigation or
tions (eg, manual processing of test data, financial) and contingency plans for the safe and effective delivery of services in
supply shortages mean that testing capacity has fallen the short and longer term. In particular, the collection of high quality
below growing demand across the EU.78 According to the and reliable data on health and social care provision will support a
World Health Organization and European Commission, targeted approach for identifying (cost-)effective strategies for re-
in the case of insufficient testing capacity, priority groups structuring and investment in health and social care, likely including
for rapid testing in EU countries should include those greater flexibility in service provision (eg, telehealth, needs vs diag-
at increased risk of developing severe disease (including nosis based support) and community based care.
acute respiratory illness and elderly populations with Clinical practice recommendations
chronic health conditions); symptomatic health and 1. Mandatory provision of alternative, accessible and easy- read
social care workers; and those in closed settings, such as healthcare information and communication toolkits.111 112
residential care homes76 79—criteria highly relevant to a 2. Mandatory consultation with autistic people to provide prior infor-
proportion of autistic people. mation about themselves, their preferences and healthcare needs,
in case they become unable to communicate on admission to hos-
However, it must be acknowledged that many autistic
pital (eg, the COVID-19 ‘Grab and Go’ Guide).113 This is essential
people experience additional barriers that could increase to prevent healthcare decisions being made without the consent of
their risk of poor outcome from COVID-19, which should patients and their families, as exemplified by the concerning ap-
therefore also be explicitly acknowledged in policy and plication of COVID-19 'Do not attempt resuscitation’ orders to the
clinical documentation and guidance. These barriers notes of some autistic people, without consultation.114
include atypical symptom presentation (which may partly 3. Mandatory, regularly updated formal guidelines and training for all
reflect high comorbidity burden and also lead to relevant healthcare providers, co-developed with autistic people and sup-
comorbid physical health risk factors going undiagnosed), ported by access to specialist providers like learning disability or
diagnostic overshadowing, and difficulties identifying psychiatric liaison staff.35 63 115
4. Introducing flexibility to some regulations (if appropriate), such as
and describing symptoms (see reviews of interoception
allowing a caregiver or support person to accompany the individual
difficulties and alexithymia in autism),80 81 which could into hospital, following all necessary infection control procedures
lead to late or missed diagnosis, or misdiagnosis, and diffi-
culties gaining access to appropriate treatments. Continued
10 Oakley B, et al. BMJ Open 2021;11:e045341. doi:10.1136/bmjopen-2020-045341Open access
guidance to be provided for clinicians on the fair allo-
Box 1 Continued
BMJ Open: first published as 10.1136/bmjopen-2020-045341 on 17 May 2021. Downloaded from http://bmjopen.bmj.com/ on July 6, 2021 by guest. Protected by copyright.
cation of resources in times of scarcity. For example,
(already in place in regions of the UK, Germany and the Netherlands, officially documented intensive care triage protocols for
according to clinician reviews) and making reasonable adjustments public health emergencies, combined with designated
to ensure this flexibility is fulfilled in real-world clinical settings. local ethics panels within healthcare settings, are essential
to ensure that individual clinicians are never responsible
for taking or implementing triage decisions and to avoid
Considering these issues, our first recommendation conflicts of interest.86 87 On the grounds of fundamental
for an aligned European strategy for responding to human rights, it is paramount that this guidance does not
pandemic situations is that— in the case of testing short- discriminate against individuals or groups of individuals
ages—autistic people should be considered for priority on any illegitimate grounds, including developmental
access to testing if they are living in ‘high risk’ settings for difference or disability, as highlighted in a recent open
disease transmission (even when apparently asymptom- letter by the International Disability Alliance88–90 and
atic), such as residential care and supported accommo- reflected in the ICU triage protocols of eight of the 14
dation (box 1). European regions reviewed (please see table 1).
To further promote equitable access to testing, it is Consequently, our second set of recommendations
important to also consider flexible testing methods to relate to proper resourcing and care planning, which
remove barriers for autistic people, who often experi- must be implemented to support autistic people who
ence sensory sensitivities associated with procedures like develop severe COVID-19 symptoms in general hospital
swab tests. Currently, if an individual is symptomatic but settings (box 1).
cannot be tested then good public health practice would While these recommendations have been specifically
be to treat the individual as a suspected case, which applied to supporting the needs of autistic people, it
could result in enhanced (and potentially unnecessary) should be emphasised that they may be more broadly
restrictions being disproportionately imposed on some beneficial for other groups. For instance, introducing
groups of individuals with additional needs. Examples of flexibility to regulations may also support individuals with
methods for enhancing the accessibility of testing proce- intellectual disability (but not autism), other neurodevel-
dures include the provision of high-quality preparatory opmental conditions (eg, attention deficit hyperactivity
materials, such as social stories and videos, available in disorder and behavioural problems) and mental health
different languages and easy-read formats, to demonstrate conditions, such as anxiety. Similarly, the provision of
the testing procedure in advance (for examples, please accessible healthcare information and communication
see AsIAm 87). Moreover, for those who cannot tolerate toolkits would be equally applicable for individuals with
swab testing, the use of non-invasive saliva sampling could sight or hearing loss, or speech and language difficulties.91
be considered and can be readily performed at home. Of Moreover, our third recommendation is that triage
note, the utility of the saliva method for COVID-19 testing protocols are urgently reviewed and updated, in consul-
has been demonstrated82 83 and is already approved by the tation with stakeholders, to inform an aligned European
US Food and Drug Administration, and in use in some strategy on the fair allocation of resources in public health
European countries, including Germany. emergencies (box 1). This strategy is essential to prevent
the widespread exclusion of autistic people from ICU, to
Enhancing access to treatment, hospitalisation and intensive
promote better healthcare equality across Europe, and to
care
provide official guidance and support to regions where it
Enhancing the accessibility of COVID-19 testing, particu-
is currently unavailable. Joint consultation between ICU
larly in cases of shortage, has added potential to reduce the
clinicians and the autism community could further aid
proportion of autistic people who require any treatment,
hospitalisation or intensive care by reducing viral trans- this progress by clarifying the application of triage proto-
mission. This is significant given that autistic people often cols in everyday clinical practice, reducing the potential
have suboptimal experiences of accessing healthcare and for bias to enter into clinical and legislative recommenda-
hospital admission,13–15 and experience higher odds of tions, and promoting transparency to ensure that individ-
death in hospital. Furthermore, the resources required to uals are not deterred from seeking services due to fear of
adequately support autistic people during hospitalisation exclusion.
are likely to be considerably stretched in pandemic situ-
ations.84 There have been (and are currently) concerns Enhancing access to existing health and social care services
across Europe about the ‘surge’ capacity of healthcare With the proper resourcing and funding of health and
systems to cope with acute increases in patients requiring social care systems, the prospective need to implement
hospital and intensive care beds.85 triage protocols is reduced. After the economic crisis of
Increasing capacity and investing in resilience plan- 2008–13, public spending on health slowed or fell across
ning should be the primary response for ensuring equal at least 24 European countries, both in absolute terms
access to hospital and intensive care resources, across and as a share of overall government spending.92 In
the population. Nevertheless, it is necessary for formal addition, there is very little available evidence to suggest
Oakley B, et al. BMJ Open 2021;11:e045341. doi:10.1136/bmjopen-2020-045341 11Open access
the most (cost-)effective ways to provide social care for provisions (eg, strategies for earlier detection of support
BMJ Open: first published as 10.1136/bmjopen-2020-045341 on 17 May 2021. Downloaded from http://bmjopen.bmj.com/ on July 6, 2021 by guest. Protected by copyright.
autistic people.93 needs and early interventions) for autistic people.
Despite these issues, many non-emergency health and
social care services have not altogether ceased as a result of Learning from best practice and future directions
COVID-19, but instead have been shifted from in-person Though it is of paramount importance to address the
to remote or online delivery (ie, ‘telehealth’). The fast barriers for COVID-19 health and social care services
implementation of telehealth in response to COVID-19 highlighted in this review, it should be noted that we
could have a positive impact on clinical practice in the also identified good examples of strategies to support
longer term,94 95 particularly for improving accessibility autistic people and those with intellectual disability. Many
and reducing costs of health and social care services. services and individual professionals have made consid-
For instance, one previous systematic review showed that erable efforts to continue to support autistic people in
outcomes of telehealth assessment and interventions for these unprecedented times and shown incredible adapt-
autistic people were broadly comparable to face-to-face ability and innovation. For instance, non-profit organisa-
consultations and superior to comparison groups who tions across Europe have provided comprehensive and
received no consultation at all.96 Additionally, telehealth accessible online toolkits to support families and regular
may be particularly beneficial for enabling individuals expert webinars on topics like mental health and coping
who live in areas with particular service or specialist staff with uncertainty.23 102 103 Additionally, some healthcare
shortages to access high-quality support from elsewhere.97 providers have implemented 24/7 telehealth services and
Thus, even prior to COVID-19, telehealth had been iden- live-in residential care.63 Several reasonable adjustments
tified as a key area for promoting more effective, acces- have also been made across Europe for autistic people,
sible and resilient European healthcare systems.98 including exceptions on wearing face masks in public
However, there is a lack of research about the most and allowing increased daily exercise during lockdown
effective and appropriate methods for implementing tele- periods. Finally, in response to lobbying by non-profit
health services that ensure continuity of care, and more organisations, new and amended guidance on supporting
data are needed about which in-person services (particu- autistic people has started to be released, which we aim to
larly in the social care domain) are (or are not) conducive complement and accelerate with the current report.
for remote implementation. Therefore, to ensure that It is clear there are many additional issues facing autistic
telehealth fulfils its future positive potential to improve people in relation to COVID-19, which were beyond the
the quality of healthcare for autistic people and those with scope of the current review, but must be investigated
intellectual disability, more research is required on how in future research. These issues include the impact of
it can be implemented in an accessible and personalised isolation; changes in education and employment; public
way.99 100 For instance, the European Disability Forum understanding of adjustments to regulations for autistic
recommends that all information is provided in plain, people; and, now, how earlier policies have impacted on
easy-to-read language, alternative methods are provided the accessibility of vaccination programmes and strate-
for those who communicate by different means or who gies. In particular, the mental and physical health impacts
do not have access to certain technologies (eg, video, tele- of COVID-19 should be assessed, given high reported
phone, email/messaging services), and the accessibility rates of pandemic-related stressors among families with
needs of different groups (including younger children) a child with autism,104–106 and possible long-term mental
are considered—for example, appropriate sign language and physical health implications of COVID-19 infec-
interpretation or captioning and symbols.101 Some of tion.107 108 Furthermore, longitudinal data on health and
these recommendations require that the care provider social care access and the impact of disruptions to educa-
has specialist training on supporting autistic people and tion and community facilities before, during and after
those with intellectual disability, and all require future the COVID-19 pandemic may reveal critical areas for
research into their efficacy in everyday clinical practice. addressing future policy and practice.
Overall and based on the evidence reported above, our
final (and broadest) recommendation is that the impact Strengths and limitations
of COVID-19 on health and social care service provision This review represents the first comprehensive analysis
for autistic people is comprehensively reviewed to inform of COVID-19 health and social care access for autistic
contingency plans for the safe and effective delivery of people across 15 European countries, also capturing the
services in the short and longer term (box 1). This could lived experiences of over 1300 individuals from the autism
include a shift to more community-based care and incor- community. Nevertheless, our findings must be consid-
porating greater flexibility to ensure that services can ered in the context of the following limitations. First, it
quickly adapt to changing circumstances—for example, was not possible to collect information from all Euro-
reducing the demand for a formal diagnosis of autism as pean countries in this study and there were important
a prerequisite for accessing needs-based support. Further- regional differences within countries that were included,
more, there is a significant need for high-quality and reli- in terms of COVID-19 policies and public health strat-
able data75 to identify key areas for targeted restructuring egies. As a result, the reported findings represent an
and investment for improving health and social care overview, rather than a nuanced analysis, of the current
12 Oakley B, et al. BMJ Open 2021;11:e045341. doi:10.1136/bmjopen-2020-045341You can also read