Covid-19 Vaccination Standard Operating Procedure - DCHS Vaccination Centres DCHS Local Vaccination Services inc Hospital Hubs
←
→
Page content transcription
If your browser does not render page correctly, please read the page content below
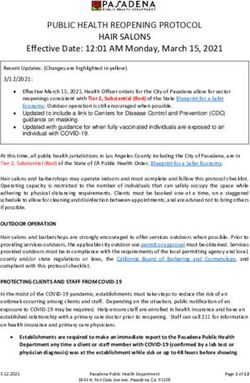
DCHS Covid19 Vaccination SOP Covid-19 Vaccination Standard Operating Procedure DCHS Vaccination Centres DCHS Local Vaccination Services inc Hospital Hubs Jan 2021 final v2 Review Sept 2021 Page 1
DCHS Covid19 Vaccination SOP
Contents
1. Introduction............................................................................................................................................ 3
1.1 Governance ....................................................................................................................................................... 3
1.2 Accessing the Target Population ...................................................................................................................... 3
1.3 Infection Prevention & Control .......................................................................................................................... 3
1.4 Vaccine Properties & Requirements ................................................................................................................. 4
1.5 Vaccine Ordering See Section 5 ....................................................................................................................... 4
1.6 Vaccine Receipt, Storage & Waste See section 5 & 6...................................................................................... 4
1.7 Authorisation to Administer Covid Vaccines See Section 7 .............................................................................. 5
1.8 Data Protection.................................................................................................................................................. 5
1.9 Maintenance of Records ................................................................................................................................... 5
1.10 Disposal of Vaccines and Other Waste ............................................................................................................ 6
1.11 Business Continuity Plan Appendix 21 ........................................................................................................ 6
2. Staffing .................................................................................................................................................. 7
Staff Roles and Responsibilities.................................................................................................................................... 7
3. Overview of Clinical Process ................................................................................................................. 7
4. Non-vaccine Supply Chain Consumables .............................................................................................. 8
5. Vaccine Ordering, Receipt, Stock Control, Waste .................................................................................. 9
5.1 Responsibility .................................................................................................................................................. 9
5.2 Receiving Vaccine Stock ................................................................................................................................... 9
5.3 Vaccine Stock Management ........................................................................................................................... 10
5.4 Issuing Vaccines ............................................................................................................................................. 10
5.5 Vaccine Returns .............................................................................................................................................. 11
5.6 Vaccine Waste ................................................................................................................................................ 11
6. Fridge Storage, Temperature Monitoring, Cold Chain .......................................................................... 12
6.1 Temperature Monitoring of Vaccine Fridges ................................................................................................... 13
6.2 Temperature Excursions ................................................................................................................................. 14
6.3 Validated Cool Bags & Boxes (vaccine porters) ............................................................................................. 14
7. Authority to administer: Patient Specific Direction (PSD), National Protocol, Patient Group Direction
(PGD) ......................................................................................................................................................... 15
7.1 Staff Authorisation to be supplied with and Administer Covid-19 Vaccines ................................................... 15
7.2 Patient Specific Direction ................................................................................................................................ 15
7.3 Patient Group Direction (PGD) Appendix 7 .................................................................................................... 16
7.4 National Protocol ............................................................................................................................................. 16
8. Vaccine Specifics ................................................................................................................................ 17
9. Vaccination, Observation, Clinical Incidents ........................................................................................ 18
10. Record Keeping Other than Vaccine Stocks .................................................................................... 18
11. Supply of Vaccines to Roving Vaccinators Including Care Homes ................................................... 19
12.1 IT ..................................................................................................................................................................... 19
12.2 Cleaning .......................................................................................................................................................... 19
Jan 2021 final v2 Review Sept 2021 Page 2DCHS Covid19 Vaccination SOP
12.3 Waste Management ........................................................................................................................................ 19
12.4 Security ........................................................................................................................................................... 19
12.5 Business Continuity plan : Appendix 16 ......................................................................................................... 20
13. Occupational Health ............................................................................................................................. 20
14. Appendices ........................................................................................................................................... 20
1. Introduction
This document describes processes and procedures for safe delivery of Covid-19 vaccination within a fixed
vaccination facility using an inserted Point of delivery (Pod) model of delivery. It is to be read in conjunction
with the relevant policy:
COVID-19: the green book, chapter 14a - GOV.UK (www.gov.uk)
COVID-19 Vaccines – SPS - Specialist Pharmacy Service – The first stop for professional medicines
advice
Model NHS COVID-19 Primary Care Vaccine handling and management policy 2020-21 Appendix
17
Vaccine handling and management policy (Hospital Hubs and Centres) 2020/21 Appendix 18 and
Vaccine Deployment in community setting SOP Appendix 19
1.1 Governance
DCHS will take the role as lead provider for Covid-19 vaccination in Derbyshire. Governance
policies of the local provider will be followed by all persons working within this SOP. The nurse
manage, site manager and clinical co-ordinator are responsible for sharing and checking
understanding of staff working each shift with relevant sections of this SOP with staff working.
Before Go-live Vaccination Centres DCHS hospital Hubs require sign off by DCHS Chief Pharmacist
following NHS England Chief pharmacist letter.
1.2 Accessing the Target Population
The Service Lead Provider and regional vaccination teams will establish target population for
vaccination as directed by NHSE Cohort Priorities, to ensure capacity and service requirements are
capable of meeting demand and expected vaccinations figures.
These should include but not be limited to:
Size of target population
Population demographic / conurbation centres (age, sex, ethnicity, culture)
Single Practice list, Combined Practice lists, geographical area, specific location (care home)
Special requirements or features of the target population (occupational health, reduced mental
capacity, shielding, detained)
Access issues for population
1.3 Infection Prevention & Control
Adherence to DCHS PPE guidance and social distancing guidance must be followed:
Vaccinators to wear face mask – these need to be changed after each session or if soiled
Jan 2021 final v2 Review Sept 2021 Page 3DCHS Covid19 Vaccination SOP
Staff diluting the pfizer vaccine must wear apron, gloves and facemask
Patients to wear face covering
1.4 Vaccine Properties & Requirements
There will be several different Covid-19 vaccinations available in the UK. On any given day the
service will understand the properties of the vaccine, storage and cold chain requirements and
follow safe procedures for the transportation and delivery of the vaccine to the point of
administration.
All Covid-19 Vaccines will be unlicensed during this vaccination program. The UK government with
the Medicines Healthcare Regulatory Agency have introduced special measures and processes to
support the administration of unlicensed vaccines
Vaccination centres: are to become temporary hospital premises listed as the temporary
responsibility of a particular NHS Trust. The expectation is that those vaccines requiring final dilution
to be done at those premises will be done under section 10 of the Medicines Act 1968, i.e. by or
under the supervision of a pharmacist, unless the vaccine characteristics do not warrant this.
GP (PCN) led local vaccination services come under Regulatory compliance by the doctor/GP
under reg.3 of the Human Medicines Regulations 2012 means that GPs are accountable for the
process, being done in their name and they must be satisfied it is being done by a person acting
within their professional competence, ordinarily a pharmacist but it could be a suitably trained nurse
1.5 Vaccine Ordering See Section 5
DCHS clinical leads for vaccine centres and Hospital Hubs are responsible for ordering vaccines.
Each site / centre needs registering on IMMFORM On receipt of orders batch numbers need to be
recorded on Pinnacle for public vaccinations or NIVs for staff peer to peer vaccinations to allow
vaccinators to select batch numbers from a drop down list.
1.6 Vaccine Receipt, Storage & Waste See section 5 & 6
A named registered healthcare professional must be available on site to check and receipt vaccines
and place in appropriate secure medical fridge. The named registered healthcare professional must
be aware of vaccine quantities expected and escalate any missing stock immediately.
Batch numbers and expiry dates must be checked and recorded on both Foundry / and or NIVs and
in Stock control register.
Vaccine must be stored in secure medical fridge with temperature monitoring and a data logger.
The fridge temperature must be logged and reset at the start, end and middle of the day. Completed
temperature logs must be stored and filed.
Label of the vial packaging must be defaced or destroyed before disposal. This is due to the risk of
theft of empty packaging.
Empty outer cartons must be disposed of in a secure manner which prevents theft. ie score through
label text with a permanent marker and cut the box up into pieces before disposal.
Jan 2021 final v2 Review Sept 2021 Page 4DCHS Covid19 Vaccination SOP
1.7 Authorisation to Administer Covid Vaccines See Section 7
This summary should be read alongside the more detailed version:
https://www.england.nhs.uk/coronavirus/publication/legal-mechanisms-for-administration-of-the-c
Note as each new vaccine is approved a new Patient Group Direction and National Protocol will
require development and National approval. During the interim period a Patient Specific Direction
may be used whilst waiting other national templates
Prescribing: Doctors and nurse and pharmacist independent non-medical prescribers (NMPs) as
‘appropriate practitioners’ can supply prescription only medicines without prescriptions and
administer injectables without directions (Human Medicines Regulations reg.214 (1) and (2) (3).
This means that a Patient Specific Direction (PSD) or another type of written direction is not
required as long as the doctor or NMP is carrying out the whole process of clinical assessment,
consent and administration. A clinical record of this must be made (using the relevant IT system) as
is normal practice.
Patient Specific Direction (PSD): if tasks are being split with a different Health Care Professional
(HCP) or trained staff member carrying out the vaccine administration process, this would require a
written PSD to be in place to cover legal supply and administration by the other healthcare
professional or trained staff member. A PSD requires a prescriber to carry out the clinical
assessment process.
Patient Group Direction (PGD): when using a PGD the clinical assessment cannot be split from
the administration and documentation all of these need to be undertaken by the same healthcare
professional authorised to work under the PGD, as does completion of the clinical record.
National Protocol: The National Protocol allows tasks to be split between registered and non-
registered healthcare professionals throughout the vaccination process, from clinical assessment
and consent to administration and post vaccination observation. Alternatively it may be followed
wholly from assessment through to post-vaccination by an appropriately registered healthcare
professional. Where multiple person models are used, the service provider/contractor must ensure
that all elements of the protocol are complied with in the provision of vaccination to each individual.
The provider/contractor is responsible for ensuring that persons are trained and competent to safely
deliver the activity they are employed to provide under this protocol. As a minimum, competence
requirements stipulated in the protocol under Characteristics of staff must be adhered to.
Further information can also be found on the Specialist Pharmacy Services website.
1.8 Data Protection
All staff have a responsibility to ensure that they do not disclose information about the service,
service users, staff members and corporate documentation to unauthorised individuals.
1.9 Maintenance of Records
All records must be maintained in accordance with relevant SOPs. These include the ordering,
receipt and issue of vaccines, tracking of product, plus patient focused records including consent
and administration.
Any serious adverse reactions are to be escalated for immediate senior clinical input; such
situations are to be fully documented following the event and a record kept of relevant product batch
numbers. A record of all serious adverse events is to be provided to the Responsible Pharmacist.
Jan 2021 final v2 Review Sept 2021 Page 5DCHS Covid19 Vaccination SOP
1.10 Disposal of Vaccines and Other Waste
Disposal of waste vaccines and any sharps must be undertaken in a safe and secure manner in
accordance with relevant SOPs see section 12.3.
1.11 Business Continuity Plan Appendix 21
A business continuity plan is available for reference see Appendix 21
Jan 2021 final v2 Review Sept 2021 Page 6DCHS Covid19 Vaccination SOP
2. Staffing
Staff Roles and Responsibilities
Staff roles and responsibilities differ according to vaccination model and according to availability of
appropriate legislation to support the process:
PGD: all aspects from assessment to administration must be undertaken by the named registered
Healthcare professional
National Protocol: clinical assessment must be undertaken by a trained registered healthcare
professional, other roles including dilution, vaccine preparation and administration can be
undertaken by trained non-registered staff
Vaccination Centres require a pharmacist to be present throughout to oversee vaccine storage,
supply, issues handling and dilution in order to assure vaccine integrity. Hospital Hub sites require
supervision by a pharmacist. In other vaccination sites and services a pharmacist presence is not
required, the nurse manager or clinical lead is responsible for maintaining vaccine integrity and
process as outlined above.
3. Overview of Clinical Process
All staff and volunteers must receive training in their role and responsibilities and be signed off
before being eligible for working in Covid-19 vaccination programs and following the instruction in
this Standard Operating Procedure (SOP).
At the start of each shift the nurse manager must ensure each member of clinical staff, Doctors,
Nurses, Pharmacists, Other Healthcare professionals, HealthCare workers, Vaccinators, non-
registered staff and administrative support staff are:
o Informed of their roles and responsibilities ideally by using a written role card, this includes
named person for vaccine stock management including issues, receipts and monitoring
vaccine waste.
o Complete declaration of training and competence register relevant to their role and
o If following the National Protocol the clinical supervisor (nurse, doctor, pharmacist) must
ensure all staff working under the National Protocol (including the clinical supervisor role)
sign off their role These registered must be filed and stored for 10 years,
The operation manager must repeat the above for site Marshall, Front of House
All staff must be compliant with Infection Prevention and Control measures and wear PPE
appropriate to role.
During the operation of the vaccine centre and local vaccine services staff must be available as
described above.
Vaccine stock will be ordered, receipted and stored in line with Order, Receipt and Storage section
of this SOP.
On confirmation of booking into a session the vaccinee presents at allotted time to the designated
location
Jan 2021 final v2 Review Sept 2021 Page 7DCHS Covid19 Vaccination SOP
The vaccinee will be screened before access into premises for health check and confirmation of
appointment by Marshal. See Appendix 1.
Eligible vaccinees will be asked to wait in an appropriately distanced waiting area and invited into
the building by a marshal according to flow.
National Protocol or PSD
In an assessment area:
A registered Health Care Professional will complete clinical screening to identify vaccinees who
have a contra-indication to the vaccine or who require a temporary deferral of the vaccine and refer
these individual to medical staff for further advice. The registered Health Care Professional will also
provide information regarding the vaccine and ask for patient consent see Appendix 7
If a Patient Specific Direction (PSD) is being used vaccinees will be assessed by a prescriber for
vaccination and where appropriate completion of Patient Specific Direction. See Appendix 7.
Eligible vaccines will progress to vaccination area where a trained member of staff (registered or
non-registered) will prepare and draw-up the vaccine and either administer the vaccine or supply the
vaccine to the vaccinator to administer
- An appropriately trained member of staff will record vaccinator and vaccinee details, vaccine batch
number and manufacturer’s expiry date, as well as site of injection see Section 10 Record Keeping
and supply a vaccination card as a prompt to attend for second dose of the same vaccine. Following
vaccination patients will be reminded to attend for a second dose and invited to sit in the
observation bay for observation of any immediate reactions / side effects for duration of:
15* minutes for all patients driving or any patient receiving Pfizer vaccine * may change according to
vaccine brand/ manufacturer. Patients will self time
Note: car insurance may be invalidated if vaccinees choose to drive without waiting for the advised
time
Vaccine stock control, storage and waste must be closely monitored and reported using the agreed
process. See Section 5 for details.
Patient Group Direction (PGD)
Under A PGD the full process from patient assessment, consent, vaccine administration, patient
information and record keeping must be completed by the same healthcare professional.
Administrative staff may check patient’s details are correct on the clinical system prior to the PGD
process taking place. Post vaccine observation must take place as detailed under National Protocol
and can be conducted by another member of staff. See Appendix 7
4. Non-vaccine Supply Chain Consumables
See Appendix 2.
Foundry order system will be used
Anaphylactic Kits (Appendix 11) will be supplied on order system, there are 2 types available, one is
contains adrenaline the other contains adrenaline, chlorphenamine and hydrocortisone. MHRA and
Resus Council UK advise that from Dec 2020 the guideline advocates administration of adrenaline
IM only.
Jan 2021 final v2 Review Sept 2021 Page 8DCHS Covid19 Vaccination SOP
DCHS pharmacy have a stock of DCHS anaphylactic kits which contain adrenaline plus the Resus
council UK anaphylactic chart and safety needles and syringes which are available for DCHS staff
working in areas without immediate medical support eg roving teams and can be ordered from
DCHST.pharmacyorders@nhs.net.
5. Vaccine Ordering, Receipt, Stock Control, Waste
All sites must capture standardised data to successfully track and trace the vaccine from supply to
administration.
All sites, irrespective of stock management system, must record the same data and should liaise
with their supplier.
There will be a daily stock report generated showing available stock at sites which will be used
nationally if stock needs to be redistributed.
Receipt and issue of vaccination stock must be recorded on the IT order system eg Foundry and the
Vaccine Stock Control Register for vaccine stock management (use amended controlled drug
register or Excel programme see Appendix 4a) .
In addition batch numbers need to be recorded on NIVs for staff peer to peer vaccinations
The process includes dealing with problems such as damaged stock, errors and wastage.
5.1 Responsibility
The registered pharmacy professional (where available) or alternatively the nurse manager is
responsibility for management of vaccine stock including receipt, ordering, handling, issues,
storage, stock rotation and waste.
The responsible professional needs to ensure that vaccines appropriately booked into IT systems,
vaccine stock register is maintained, batch numbers recorded onto NIVs, Pinnacle and Foundry,
maintain the cold chain and appropriate temperature storage, store securely at all points between
receipt and use or disposal.
Waste vaccines, empty vials and cartons must be managed according to local waste
management procedures, and in such a way as to prevent theft. See Section 5.6 and 12
Health and Safety risk assessments should be undertaken locally to ensure these risks are
adequately controlled.
The following process must be followed :
Ordering: Appendix 3 ordering vaccines VH1 in centres or Ordering vaccines in PCN
Sites https://www.sps.nhs.uk/articles/ordering-pfizer-biontech-covid-19-vaccine-by-pcn-
designated-sites/
5.2 Receiving Vaccine Stock
A dedicated Health Care Professional must be allocated to receive and manage vaccine stock.
Jan 2021 final v2 Review Sept 2021 Page 9DCHS Covid19 Vaccination SOP
The assigned staff must be aware of the importance of maintaining the cold chain and follow this
SOP including training in handling stock including keeping mRNA Pfizer vaccine upright
For each order, follow the process in Appendix 4a receipt of vaccines, checking quantity, batch
numbers and integrity of product, quarantining, reporting and documenting any missing or
damaged stock according to the table in waste
5.3 Vaccine Stock Management
A separate fridge shelf should be allocated for each vaccine delivery.
Fridge Vaccine boxes must be labelled with vaccine expiry date.
Shortest dated vaccines must be used first.
No vaccines can be returned to the main fridge after issue.
5.4 Issuing Vaccines
At the start of each shift the:
Quantity of vaccine in all fridges should be checked and confirmed against Foundry /the vaccine
stock control register
Any expired stock must be identified, documented on IT system and register and witness destroyed
using the waste codes descriptors in section 5.6
Individual with responsibility for vaccine stock should issue each vaccinator with a supply of vaccine
sufficient for the number of patients to be treated until break time.
NOTE
The ID of the person collecting the vaccines must be checked and documented.
Documentation must be kept of every issue (See Appendix 4), including date, time, brand, quantity,
and location of issue
Use a separate page for each vaccine brand.
The quantity issued will depend on the number of vaccinations planned per session list and
vaccine’s cold chain properties, e.g.
o Pfizer vaccine is only stable for 2 hours if undiluted at room temperature hence only a
limited number of vials should be issued at any one time in a zip lock bag labelled with 2
hour expiry
o Most other vaccines are stable for long periods at temperatures of 2 – 80C. Quantities can
be issued according to cold chain temperatures and scheduled vaccinations per session.
Note DCHS validated cool bags generally only maintain the temperature for a maximum of 4
hours hence roving vaccinators should only be issued with sufficient vaccines for this time frame.
Validated vaccine porters / boxes may maintain cold temperature for longer, eg up to 12 hours.
Jan 2021 final v2 Review Sept 2021 Page 10DCHS Covid19 Vaccination SOP
5.5 Vaccine Returns
Currently NO vaccines can be returned to the main fridge once they have been issued.
Vaccines not used at the end of each session should have their expiry dates / times checked by
vaccinators, short dated stock destroyed and documented on Foundry and / or the vaccine
register. See Waste section 5.6.
Vaccines unused by roving teams must be destroyed at the end of each session and documented
on Foundry and /or the vaccine register even if the cold chain has been maintained following the
process in Waste below
Within a Pod vaccinators may share concentrated vaccines
5.6 Vaccine Waste
Vaccine waste must be documented on Foundry
Vaccine waste may occur at 3 points in the process:
Main fridge stock going out of date or fridge temperature failure
Wastage during the process of vaccination session
Unused vaccines remaining at the end of vaccination session
Main fridge stock: waste should be disposed of safely and in such a manner that deters individuals
from trying to retrieve discarded doses or packaging
o Vaccine wasted doses must be disposed of securely in yellow lidded rigid leak proof
containers sharps bins. In addition:-
o Ensure the label of the vial packaging and vial is defaced or destroyed before disposal.
This is due to the risk of theft of empty packaging and possible re-introduction of
product in medicine supply process
o Securely store the yellow lidded sharps before collection by waste disposal contractors.
o Main stock waste must be reported to the nurse manager so that Foundry* or other IT
systems and /or the Vaccine stock control register can be updated using the using the codes
in the table below.
Jan 2021 final v2 Review Sept 2021 Page 11DCHS Covid19 Vaccination SOP
Vaccine Waste generated during the process of preparing vaccines does not need to be
documented in the Vaccine Stock control Register but on the clinical session waste Sheet See
Appendix 5. Wastage of more than 5% is considered a red flag and must be investigated.
Ensure the label of the vial packaging is defaced or destroyed before disposal. This is due to the
risk of theft of empty packaging.
Empty outer cartons must be disposed of in a secure manner which prevents theft. Score through
label text with a permanent marker and cut the box up into pieces before disposal.
Wasted’ vials must be disposed of in a yellow lidded sharps bin.
The nurse clinical supervisor must review waste documentation regularly throughout each
vaccination session and must be vigilant to any practice contributing to vaccine waste and give
support and advice to vaccinators regarding technique
At the end of each session waste forms must be reviewed and filed by the nurse manager.
Wastage of vaccines at the end of Roving sessions needs to be documented as per Roving session
process.
5.7 Spillages Appendix 7
The Pfizer-BioNTech COVID-19 (BNT162b2) is not supplied with a Material Safety Data Sheet and
the manufacturer reports that there are no special COSHH handling requirements for either routine
handling or dealing with spillages.
Procedure – Spillages on skin/eyes
Staff must be aware of location of hand washing facilities and eyewash kits. Spillages on skin
should be washed with soap and water.
If a vaccine is splashed in the eyes, they should be washed with sterile 0.9% sodium chloride
solution and medical advice should be sought.
Procedure – Spillages on surfaces
Spillages must be cleared up quickly and gloves should be worn.
The spillage should be soaked up with paper towels, taking care to avoid skin puncture from glass
or needles.
The area should be cleaned according to the local chemical disinfection policy.
Gloves, towels, etc. should be sent for incineration.
6. Fridge Storage, Temperature Monitoring, Cold Chain
The principles of vaccine storage must be adhered to i.e:
All vaccines must be stored in a medicine fridge with temperature monitoring Section 6.1
All vaccines must be stored in manufacturer’s original containers
The fridge must not be over stocked
Vaccine stock must be used in order of receipt
Jan 2021 final v2 Review Sept 2021 Page 12DCHS Covid19 Vaccination SOP
Ideally a single shelf should be allocated for each delivery
Where fridges are mostly empty it is advisable that validated cool bags and cool packs are stored in
the fridge to help maintain the efficient functioning of the fridge.
6.1 Temperature Monitoring of Vaccine Fridges
Validation and monitoring of cold chain
Refrigerators should be validated and monitored in accordance with existing local procedures. If
cold chain recommendations are adhered to and the temperature is properly monitored, the risk
of vaccine storage incidents and cold chain failures will be reduced, ensuring that vaccines are in
optimum condition for those individuals they are given to and also reducing the risk of vaccine
wastage.
General principles of vaccine storage are:
All vaccines and diluents must be stored in a lockable dedicated vaccine/medicine fridge between
2oC and 8oC (unless other specific storage requirements have been specified)
Systems to prevent accidental interruption of the power supply to the fridge must be in place,
ideally fridges should be hard wired into electricity supply
Fridges should be situated away from radiators and other sources of heat that could affect how
they work
Records should be kept of regular servicing and thermometer calibration
The temperature in the fridge must be continually monitored using a current/minimum/maximum
thermometer
Fridge temperatures should be monitored and recorded on a designated chart at the start and
end of each shift.
Fridge alarm parameters should be set appropriately to alert to any deviations from the 2oC to 8oC
range
Vaccines must be stored in their original packaging
Vaccines with shorter expiry dates should be placed at the front of the fridge
Expired stock should be removed from the fridge and destroyed and an entry made in the vaccine
stock control register
Staff must know what action to take if temperature goes outside recommended range: see below
Covid-19
There should be a named person and a deputy responsible for COVID-19 vaccine storage. This
person will be identified at the start of each shift by the nurse manager
Those responsible should be familiar with the fridge digital display readings, the functioning of the
thermometer reset button, and the manufacturer's user guidelines. See Appendix 6a Temperature
Monitoring Charts
Jan 2021 final v2 Review Sept 2021 Page 13DCHS Covid19 Vaccination SOP
Data loggers can be useful in the event of a cold chain breach as the data can be used to calculate
cumulative exposure to out of range temperatures. However, they should always be used in
conjunction with the integral fridge thermometer and should not be used to replace the daily
temperature monitoring and recording.
A visual check of the actual temperature should also be made each time a vaccine is
removed from the fridge.
A fridge data logger independent of the main power source (for example, battery operated) should
be available to monitor the temperature in the event of a power failure. Data loggers are
recommended as a back up to regular visual temperature inspection and recording.
Temperature probes with cables should be correctly positioned in the fridge, ensuring that the cable
does not interfere with the door seal and that the probe is not up against the back or sides of the
fridge.
Vaccines being stored or transported in portable cool bags or refrigeration devices should be
monitored to the same standard as vaccines stored in vaccine fridges.
Vaccine storage systems must be closely monitored to ensure that the temperature
recommendations are maintained at all times.
6.2 Temperature Excursions
In the event of a temperature excursion outside the recommended range for the Covid-19
vaccines. See Appendix 6b
6.3 Validated Cool Bags & Boxes (vaccine porters)
It is essential to maintain vaccine cold chain
Only validated cool bags or boxes are suitable for transporting vaccines
Covid-19 vaccines except Pfizer brand are suitable for transport in validated cool bags/ boxes
To maintain the integrity of the vaccine validated cool bags/ boxes must be packed according to
manufacturer’s instructions
Cool blocks and gel must be chilled in a fridge as the designated temperature – often at 4 0C for at
least 24 hours in order to maintain the temperature of the container for the required duration. Failure
to do this may result in increased wastage.
It is advisable to keep a stock of cool blocks/ packaging/ plastic concentrated vaccine carrier boxes
in a fridge. These can be stored in the vaccine fridge as well as a separate fridge.
Pfizer Vaccines must be kept upright during transport, this can be achieved by carrying cool bags
like a pizza box
Example of Polar clamshell cool bag instructions in use at DCHS. See Appendix 6c
Other validated cool bags are available. These may be supplied centrally with freezing gels. It is
essential that manufacturer’s instructions are followed regarding preparing these bags, monitoring
temperature and NOT placing vaccines in these bags until the internal temperature reaches 20C.
Frozen / re-frozen vaccines must be reported and destroyed
Jan 2021 final v2 Review Sept 2021 Page 14DCHS Covid19 Vaccination SOP
7. Authority to administer: Patient Specific Direction (PSD),
National Protocol, Patient Group Direction (PGD)
7.1 Staff Authorisation to be supplied with and Administer Covid-19
Vaccines
This summary should be read alongside the more detailed version:
https://www.england.nhs.uk/coronavirus/publication/legal-mechanisms-for-administration-of-the-c
Note as each new vaccine is approved a new Patient Group Direction and National Protocol will
require development and National approval. During the interim period a patient Specific Direction
may be used whilst waiting other national templates. Using appropriate legal mechanisms for the
administration of COVID-19 vaccines – SPS - Specialist Pharmacy Service – The first stop for
professional medicines advice
Vaccines are prescription only medicines as such an appropriate and formal authorisation for
vaccine administration e.g. a Patient Specific Direction, Patient Group Direction, National protocol,
prescription or written instruction is required. Staff who administer the Covid-19 vaccine must be
those defined as eligible to do so.
7.2 Patient Specific Direction
(See Appendices 7 & 8)
Doctors and nurse and pharmacist independent non-medical prescribers (NMPs) as
‘appropriate practitioners’ can supply prescription only medicines without prescriptions and
administer injectables without directions (Human Medicines Regulations reg.214(1) and (2) (3).)
This means that a Patient Specific Direction (PSD) or another type of written direction is not
required as long as the doctor or NMP is carrying out the whole process of clinical assessment,
consent and administration. A clinical record of this must be made (using the relevant IT system) as
is normal practice.
However, if tasks are being split with a different Health Care Professional (HCP) or trained
staff member carrying out the vaccine administration process, this would require a written
PSD to be in place to cover legal supply and administration by the other healthcare
professional or trained staff member. A PSD requires a prescriber to carry out the clinical
assessment process.
Under a PSD a prescriber will need to give an authorised instruction to administer a medicine to a
list of individually named patients where each patient on the list has been individually assessed by
that prescriber. The prescriber must have adequate knowledge of the patient’s health and be
satisfied that the medicine to be administered serves the individual needs of each patient on that
list. The prescriber takes full accountability and responsibility for the patient and the members of
staff administering the vaccine. It is therefore essential that the prescriber is content with taking on
this responsibility.
The patients must have an individual clinical assessment. The clinical assessment proforma for the
Pfizer PSD and the PSD template should be completed by trained staff (Appendix 7) and Frequently
Asked Questions (Appendix 8)
If anyone other than the prescriber is carrying out the clinical assessment and consent process the
prescriber must be able to assure themselves of the process being undertaken, and the ability of the
assessing individual to carry out and record the same reliably. The prescriber must be able to
review the person being assessed prior to vaccination and intervene should this be necessary
Jan 2021 final v2 Review Sept 2021 Page 15DCHS Covid19 Vaccination SOP
Role of Prescriber
To become personally familiar with the vaccine, its conditions and limitations for prescribing and
safe administration
To make a complete the assessment of individuals presenting for vaccination and sign the
appropriate PSD
To train clinical assessors to support in the delivery of that assessment
To monitor the accuracy of the assessment processors
Role of Clinical Assessor
To become personally familiar with the vaccine, its conditions and limitations for prescribing and
safe administration
To undertake training in the assessment of individual’s suitability for vaccination
To make a prepare an assessment of individuals presenting for vaccination in support of the
Prescriber
To support audit and governance processes as required.
7.3 Patient Group Direction (PGD) Appendix 7
Note as each new vaccine is approved a new National Protocol will require development and
National approval. During the interim period a patient Specific Direction may be used whilst waiting
national templates
See link below for current national templates: Using appropriate legal mechanisms for the
administration of COVID-19 vaccines – SPS - Specialist Pharmacy Service – The first stop for
professional medicines advice
Only Registered Health Care Professionals can operate under a PGD where their registered
profession has been defined by the law.
These are: chiropodists and podiatrists, dental hygienists, dental therapists, dieticians, midwives,
nurses, occupational therapists, optometrists, orthoptists, orthotists and prosthetists, paramedics,
pharmacists, physiotherapists, radiographers and speech and language therapists.
The patient group direction provides authority for these named healthcare professionals to
administer the specific covid vaccine to individuals who meet the PGD eligibility criteria. In order to
use the PGD each individual healthcare professional must have completed the appropriate training,
have read and understood the PGD and be signed off by their line manager to use the PGD. At the
start of each shift it is the responsibility of the nurse manager to check every vaccinator and
assessor has completed training and been signed off for use on the PGD.
All tasks must be carried out by a registered healthcare professional (as defined) and cannot be
delegated to others regardless of their professional group or level of training.
For example, if the medicine is to be administered under a PGD, this should be by the same health
professional that assessed the patient under the PGD, and they will also need to be the one to
record it in the patient records.
7.4 National Protocol
Note as each new vaccine is approved a new National Protocol will require development and
National approval. During the interim period a patient Specific Direction may be used whilst waiting
national templates.
A national protocol may be followed wholly from assessment through to post-vaccination by an
Jan 2021 final v2 Review Sept 2021 Page 16DCHS Covid19 Vaccination SOP
appropriately registered healthcare professional. Alternatively, multiple persons may undertake
stages in the vaccination pathway in accordance with this protocol. Where multiple person models
are used, the service provider/contractor must ensure that all elements of the protocol are complied
with in the provision of vaccination to each individual. The provider/contractor is responsible for
ensuring that persons are trained and competent to safely deliver the activity they are employed to
provide under this protocol. As a minimum, competence requirements stipulated in the protocol
under Characteristics of staff must be adhered to.
A clinical supervisor, who must be a registered doctor, nurse or pharmacist trained and competent
in all aspects of the protocol, must be present and take overall responsibility for provision of
vaccination under the protocol at all times and be identifiable to service users. The final dilution and
drawing up of the vaccine has its own supervision requirements in accordance with Part 1 of the
HMR 2012 and will need to be done by, or under the supervision of, a doctor, nurse or pharmacist.
If a vaccination service is being provided at scale, the clinical supervisor should only take on
specific supervision requirements in relation to the dilution and drawing up of the vaccine if this can
be done safely alongside their overarching role. Any time the protocol is used, the name of the
clinical supervisor taking responsibility and all the people working under different stages of the
protocol must be recorded for the session. The clinical supervisor has ultimate responsibility for safe
care being provided under the terms of the protocol. Staff working under the protocol may be
supported by additional registered healthcare professionals, but the clinical supervisor retains
responsibility. Staff working to the protocol must understand who the clinical supervisor for their
practice at any time is and can only proceed with their authority. The clinical supervisor may
withdraw this authority for all members of staff or individual members of staff at any time and has
authority to stop and start service provision under the protocol as necessary. Every member of staff
has a responsibility to, and should, report immediately to the clinical supervisor any concerns they
have about working under the protocol in general or about a specific individual, process, issue or
event.
The clinical supervisor must be a registered doctor, nurse or pharmacist trained and competent in all
aspects of the protocol, must be present and provide clinical supervision for the overall provision of
clinical care provided under the legal authority of the protocol.
Operation under this protocol is the responsibility of service providers/contractors.
See link below for current national templates Using appropriate legal mechanisms for the
administration of COVID-19 vaccines – SPS - Specialist Pharmacy Service – The first stop for
professional medicines advice
8. Vaccine Specifics
See Appendices 9 & 10 for preparation and administration of specific vaccines and
checklist.
The vaccine dose needs to be presented in a syringe ready for administration. Some of the covid
vaccines will need manipulating either by drawing up doses from a multi-dose vial or by dilution
Other covid vaccines may be presented in prefilled syringes
Staff must follow the preparation instructions precisely, use each drawn dose immediately and use
the same needle to administer the dose which has been used to drawn up the dose, changing the
needle results in loss of dose
Infection Prevention and Control processes must be followed
Aprons and gloves should be worn when preparing vaccine.
Pfizer mRNA vaccine is very fragile. Vials must not be shaken – if a foam develops it is a sign
that the vaccine has been damaged and the vial must be discarded.
Jan 2021 final v2 Review Sept 2021 Page 17DCHS Covid19 Vaccination SOP
see COVID-19 Vaccines – SPS - Specialist Pharmacy Service – The first stop for professional
medicines advice
9. Vaccination, Observation, Clinical Incidents
Vaccine centres and locations will operate in line with Covid-19 Workforce Pod Design (Appendix
10). Patient eligibility for vaccination, clinical assessment, consent and vaccine preparation will be
as Section 7 and 8 of this SOP.
All staff involved in the vaccination process must have completed the training including
anaphylaxis and BLS appropriate to their role as described in Appendix 12. Also see COVID-
19 Resource Hub: Webinar: Anaphylaxis (rcgp.org.uk)
An anaphylactic kit (Appendix 11) will be available in each Pod and for each roaming vaccinator
Post-vaccination observation period
After vaccination the individual will make their way to a socially distanced seat in the post-
vaccination observation area where they will be asked to wait for a period of time which may vary
according to the characteristics of the vaccine. All individuals driving will be required to wait 15
minutes if driving for post vaccination observation. Individuals will time themselves but can be
helped by staff providing timed labels or cards
Any patients feeling or looking unwell must be escalated to the Doctor on site
All vaccinees with possible anaphylaxis reaction should be managed appropriately on the site
before transfer to the nearest Emergency Department (if appropriate) where If available then
tryptase testing can take place.
All incidents must be reported in line with the national SOP via
Regional Vaccination Operations Centre (RVOC/ROC, to enable appropriate escalation and
logging of the incident. This is in addition to covid yellow card reporting..
Information and guidance for healthcare workers regarding Covid 19 vaccination and other incidents
is detailed in Appendix 20
10. Record Keeping Other than Vaccine Stocks
Accurate recording of all vaccines given and good management of all associated documentation is
essential. The nurse manager is responsible for accurate documentation.
Final documentation requirements are to be confirmed but may include:
Any DNAs (Did Not Attends)
Any contraindications to the vaccine and any alternative offered
Any decline of an offer of vaccination
Clinical Assessments
PSD
Vaccine related reactions
Jan 2021 final v2 Review Sept 2021 Page 18DCHS Covid19 Vaccination SOP
The following must be documented on Pinnacle (PCN services) or NIVs (staff peer to peer vaccinations)
Patient Details: Name, NHS number, Date of Birth
Vaccine name, product name, batch number and expiry date
Dose administered
Site vaccine administered (eg left arm)
Date immunisation(s) were given
Name and signature of vaccinator
Locality of vaccinator
11. Supply of Vaccines to Roving Vaccinators Including
Care Homes
The named registered Healthcare professional with responsibility for vaccine stock must liaise with roving
teams to supply required number of vaccine doses and appropriately chilled and packed cool bag section
6.3. Vaccine issued must be documented in stock register and collector’s ID checked see section 5.4 and
place in labelled bag indicating time removed from fridge. Waste must be monitored as in section 5.6
12. Site Support
The senior operation manager is responsible for managing and co-ordinating:
12.1 IT
Co-ordinating and working with the provider on each site. Prior to starting a shift staff need to
register for access to IT systems relevant to their roles
12.2 Cleaning
As per current site arrangements.
During working hours Pod areas will generally be maintained and cleaned by Health Care
Assistants and Observation areas will be maintained and chairs wiped down between vaccines by
the person in observer role.
12.3 Waste Management
Sites must have systems in place to manage clinical waste and unused expired vaccine stock to
ensure stock does not get stolen, re-introduced into the vaccine supply or misused in any way see
section 5.6 Vaccine waste
12.4 Security
Reasonable security requirements for the local vaccination services should be put in place and
ensure the police are aware of the location. Consider site security (including staff, locks and
alarms) if storing vaccine overnight, particularly in non-NHS sites. And raise any issues or
incidents with their commissioner and Regional Vaccination Operations Centre (RVOC
Jan 2021 final v2 Review Sept 2021 Page 19DCHS Covid19 Vaccination SOP
These must include:
Providing a safe place of work for staff and public as well as secure overnight storage of inbound
goods, expired or wasted vaccine, consumables and equipment and secure overnight storage and
maintenance of vaccine cold chain.
All staff must be aware of processes to manage incidents as and when they arise.
All incidents must be reported to the senior site manager and managed as per Appendix 20
12.5 Business Continuity plan : Appendix 16
Each site must have a business continuity plan which includes detail on how the service will respond,
recover and manage its services during disruption relating to people, information, security, premises
including utilities, facilities particularly ULT and refrigerator failure, supplier, IT and data.
13. Occupational Health
Any needlestick or other injuries must be addressed in accordance with the policies of the relevant
employing legal entity.
14. Appendices
Appendix 1 Marshal Pre-entry Checklist
Marshal checklist.pdf
Appendix 2 Non-Vaccine Supply Chain
non vaccine supply
chain 26 nov.pdf
Appendix 3 Ordering Vaccines in centres https://www.sps.nhs.uk/articles/ordering-
pfizer-biontech-covid-19-vaccine-by-pcn-
Ordering vaccine in PCN sites designated-sites/
vaccine ordering.pdf
Appendix 4 4a Receipt of Vaccines IT VH2
SOP 4a COVID-19 Vaccines – SPS - Specialist
Pharmacy Service – The first stop for
4b Receipt of Pfizer Vaccine professional medicines advice
4c Receipt of AstraZeneca
Vaccine 4b Handling in Trusts – SPS - Specialist
Pharmacy Service – The first stop for
professional medicines advice
4c Handling in Trusts – SPS - Specialist
Pharmacy Service – The first stop for
professional medicines advice
Jan 2021 final v2 Review Sept 2021 Page 20DCHS Covid19 Vaccination SOP
Appendix 5 Documenting Vaccine Waste
During Clinical Session
waste vaccine
recording clinical session.pdf
Appendix 6 6a Fridge Temperature
Monitoring
6b Fridge Temperature Fridge temperature Fridge Temperature validated cool bag
Excursions monitoring chart.pdf Excursion advice.pdf example.pdf
6c Validated Cool Bags
Appendix 7 7Clinical Assessment PSD
National Protocol Pfizer,
Clinical Assessment Clinical Assessment Clinical assessment
AstraZeneca Covid19 vaccines pfizer PGD or national protocol
pfizer PSD
v2.pdf
v2.pdf AZ National protocol or PGD.pdf
clinical assessment
AZ PSD adapted.pdf
Regulatory, COVID-19 Vaccines – SPS -
Specialist Pharmacy Service – The first stop for
professional medicines advice
Appendix 8 8a Covid-19 Guidance for
Healthcare Workers
COVID-19_vaccinati FAQ covid vaccine
8b Covid-19 Vaccine FAQ on_programme_guidance_for_healthcare_workers_December_20
v2.pdf
Regulatory approval of Pfizer/BioNTech vaccine
8c SPC
for COVID-19 - GOV.UK (www.gov.uk)
Regulatory approval of COVID-19 Vaccine
AstraZeneca - GOV.UK (www.gov.uk)
Appendix 9 Vaccine Specific Handling Pfizer-BioNTech Vaccine Preparation in Trusts
– SPS - Specialist Pharmacy Service – The first
9a Pfizer Vaccine Preparation stop for professional medicines advice
9b Pfizer Vaccine preparation
visual aid
Pfizer vaccine Pfizer Vaccine
dilution visual aid.pdfSpillages and breakages.pdf
9c Pfizer spillages AstraZeneca
COVID-19 Vaccine Preparation in Trusts – SPS
9d AstraZeneca Vaccine
- Specialist Pharmacy Service – The first stop
preparation for professional medicines advice
9e AstraZeneca Spillages
AstraZeneca-Vaccine
-Preparation-Work-Instruction-Issue-1.0.pdf
Appendix 10 Administration /PGD Prompt
sheet
Administration
prompt sheet V2.pdf
Appendix 11 Anaphylactic Kits
Anaphylactic Kits.pdf
Appendix 12 Training
Training overview for staff
groups
Training courses elearning List Training Training elearning Prescribers Training
requirements for workforce.pdf
courses.doc.pdf for PSD.pdf
Training for prescribers/ medical
staff PSD
Jan 2021 final v2 Review Sept 2021 Page 21DCHS Covid19 Vaccination SOP
Appendix 13 Covid-19 Workforce Pod Design
COVID19_Workforce
_Pod Design_PSD-02122020 v2.0-Final.pdf
Appendix 15 Roving Vaccinator SOP TO BE ADDED
Appendix 16 Business Continuity Plan
Business Continuity
Plan.pdf
Appendix 17 Primary Care Vaccine handling
and management policy 2020-21
C0945 Governance
Annex A handling and preparation of vaccines by GP_led_Local
Appendix 18 Hospital Hubs and Centres
NHS COVID-19 Vaccine handling
and management policy 2020/21 C0926 COVID-19
vaccination Governance handling and preparation of v
Annex A
Appendix 19 Vaccine deployment in
community setting SOP
C0910-COVID-19-Va
ccine-Deployment-in-Community-Settings-LVS-SOP-v2
Appendix 20 20a Covid 19 vaccination
information for healthcare
practitioners COVID-19_vaccinati C0951 Managing
20 b C0951 covid 19 Incident on_programme_guidance_for_healthcare_workers_December_20
Covid-19 Vaccination Incidents and Enquirie
reporting
Appendix 21 Patient Group Direction
PGD Pfizer mRNA vaccine COVID-19 vaccination programme - GOV.UK
National Protocol Pfizer Vaccine (www.gov.uk)
Jan 2021 final v2 Review Sept 2021 Page 22You can also read