The Doctor as a Nutritionist
←
→
Page content transcription
If your browser does not render page correctly, please read the page content below
The Doctor as a Nutritionist -
A Discussion Paper on Nutrition in Medical Careers
The UK Intercollegiate Group on Nutrition (ICGN), leads on nutrition amongst the
UK Royal Colleges and the British Dietetic as well as Dental Associations. The
ICGN, has identified four main pillars that can be used to define the science of
nutrition (www.icgnutrition.org.uk):
Dietary Intake (What you eat)
Nutritional Status (What you are)
Functional Capacity (What you can do)
Goodness of fit (Biological fit)
Although ‘diet’ and ‘nutrition’ are often used interchangeably, ‘diet’ refers to the
composition (quantity and quality) and consumption (frequency and pattern) of
snacks, meals and beverages. Nutrition also deals with nutrients that the body
synthesizes and the complex interactions between nutritional status and health. This
interaction can become a vicious downward cycle of malnutrition and illness. In 2007
up to 43 % of adults admitted to hospitals in the UK were malnourished; as were 30
% of adults admitted to care homes (British Association of Parenteral and Enteral
Nutrition; Russell & Elia, 2008).
Why nutrition is important for doctors?
Nutrition is vital for good health and to good medical treatment. Diet is an important
modifiable risk factor for many diseases including heart disease and cancer which
account for high rates of morbidity and mortality. The UK is currently dealing with
rising levels of obesity and associated conditions including type 2 diabetes, and
nutrition is an important factor in its aetiology and treatment (Foresight report 2007)
The General Medical Council (GMC) (www.gmc-uk.org) requires doctors to
understand the role played by diet and nutrition (Tomorrow’s Doctors 2002) in health
promotion or disease prevention (and management) and to take active roles in
partnership with dietitians, speech and language therapists, nutritionists, nurses, carers
and of course patients themselves and their families. A Registered Dietitian (RD) is a
regulated professional who is able to translate scientific information about food into
practical dietary advice for patients and other health care professionals
(www.bda.uk.com). Their roles also encompass work with healthy individuals and
groups. Since 2002, Registered Nutritionists / Public Health Nutritionists (RNutr /
RPHNutr) form a new professional group who work mainly with healthy individuals
and groups or populations (www.nutritionsociety.org) in nutrition and dietetics or
public health departments. Registered nutritionists may also include medical doctors
with nutrition competences.
The concepts of the nutritional basis and management of disease are well-established
in medicine. However, although doctors are the most trusted source of information
and advice, they have a reputation for being under-equipped to advise their patients on
diet and nutrition. There is potential for doctors to play a more effective role in
nutritional aspects of care.
Westminster Forum, July 2008 1Core Competences in Nutrition for “Tomorrow’s Doctors”
Universities often have an integrated vertical theme running throughout an MBBS or
MBChB programme, incorporating the elements of a Nutrition a Core Curriculum for
Health Professionals (Department of Health, 1994). This set national standards that
focus on safe practice underpinned by ‘eighteen bullet points’ that form a common
framework for all health professionals. These bullet points are due to be updated to a
new format soon by the ICGN. In addition, the Council of Europe Alliance on
Hospital Food and Nutritional Care has suggested roles and responsibilities for
doctors, in consultation with the British Medical Association. The work of this
alliance has also resulted in the “10 Key Characteristics of Good Nutritional Care”
(www.bapen.org.uk) which is common to all health professionals.
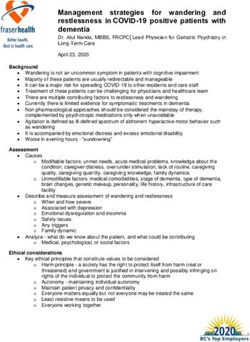
Figure (1)
The “10 Key Characteristics” of Good Nutritional Care
Core standards for all health professions and NHS organisations
1. All patients are screened on admission to identify the patients who are malnourished
or at risk of becoming malnourished. All patients are re-screened weekly.
2. All patients have a care plan which identifies their nutritional care needs and how they
are to be met.
3. The hospital includes specific guidance on food services and nutritional care in its
Clinical Governance arrangements.
4. Patients are involved in the planning and monitoring arrangements for food service
provision.
5. The ward implements Protected Mealtimes to provide an environment conducive to
patients enjoying and being able to eat their food.
6. All staff have the appropriate skills and competencies needed to ensure that the
patient’s nutritional needs are met. All staff receive regular training on nutritional care
and management.
7. Hospital facilities are designed to be flexible and patient centred with the aim of
providing and delivering an excellent experience of food service and nutritional care
24 hours a day, every day.
8. The hospital has a policy for food service and nutritional care which is patient centred
and performance managed in line with home country governance frameworks.
9. Food service and nutritional care is delivered to the patient safely.
10. The hospital supports a multi-disciplinary approach to nutritional care and values the
contribution of all staff groups working in partnership with patients and users.
Westminster Forum, July 2008 2Figure (2)
The “Eighteen Bullet Points” in Nutrition
Key facts all doctors should be able to use in their practice
A. PRINCIPLES OF NUTRITIONAL SCIENCE
1. Diets, foods and nutrients (substrates and cofactors)
2. Metabolic demand, digestion and absorption, balance and turnover, physical activity, metabolic
effects of excess, obesity.
3. Requirements, essentiality, bioavailability, limiting nutrients, effect of nutrient status on biochemical
and organ function.
4. Adaptation to low nutrient intakes, body composition (form and function).
5. Assessment of diet and nutritional status.
6. Physiological mechanisms that determine appetite, sociological, psychological, economic and
behavioural aspects of food choice.
B. PUBLIC HEALTH NUTRITION
1. The average British diet, including sub-group differences (e.g. region, gender, ethnic origin), lifestyle,
risk factors and epidemiology (socio-economic factors, smoking and activity)
2. Pre-conception, pregnancy, breastfeeding, infant nutrition, growth and development, ageing.
3. Dietary Reference Values (DRVs), dietary recommendations and guidelines, diet and coronary heart
disease and stroke, the Health of the Nation targets.
4. Nutritional surveillance and identification of markers of nutritional status.
5. Achieving change, education and motivation (education resources, theory and skills).
6. Food supply, monitoring, cost/benefit of nutritional interventions, legislation, food labelling and policy
which affects food consumption.
C. CLINICAL NUTRITION AND NUTRITIONAL SUPPORT
1. Assessment of clinical and functional metabolic state, effect of functional state on nutritional intake
and status, effect of status on clinical outcomes.
2. Anorexia and starvation, response to injury, infection and stress.
3. Altered nutritional requirements in relevant disease states, unusual requirements.
4. General principles of nutritional support, routes of support.
5. Basis of nutrition related diseases, therapeutic diets (diabetic, renal), weight reduction.
6. Drug-nutrient interactions.
Source: Nutrition Core Curriculum for Nutrition in the Education of Health Professionals,
Department of Health, 1994, pages 10-11.
Piecing together all the bits of Integrated Teaching, to create a complete Nutrition
Skills Toolkit, at the end of undergraduate medical training can be challenging. Core
undergraduate training in nutrition is an area that requires further attention, in order to
optimise preparation for the modern role of Nutrition in Medicine.
Westminster Forum, July 2008 3Choosing to learn more about Nutrition at Medical School Most undergraduate medical curricula consist of Student Selected Components (SSCs) which provide an opportunity to develop skills the student chooses themself. SSCs can vary between two weeks and two months, can enable in-depth learning outside the core medical curriculum, and can help to define career choices. Many universities offer SSCs in aspects of clinical and public health nutrition. An undergraduate wishing to explore a specific area of nutrition in depth could choose a nutrition related topic for a Fourth Year Research Project, or do in-depth nutrition research within an Intercalated Year between the 3rd and 4th years of their medical degree. A good project can result in a published paper or a presentation at a conference, which with some luck, could be at an exotic location! The more adventurous medical student may wish to do an Elective involving nutrition, perhaps overseas in a lower-income country, which often offers rich experience (this is of course time spent other than on soaking up the sights or sun!). A well planned project can lead to considerable academic mileage and educational charities such as the British Nutrition Foundation (BNF) (www.nutrition.org.uk) may be able to provide bursaries, support or advice on funding for deserving students. Voluntary Work Experience undertaken informally at anytime anywhere can provide unparalleled opportunities to gain an appreciation of day-to-day professional practice in nutrition. Postgraduate Education and Training in Nutrition for Doctors The Medical Royal Colleges through the ICGN, offer an intensive five-day Intercollegiate Certificate Course in Human Nutrition at different UK centres two to three times yearly. This underpins all specialist training by the Colleges, some of which are exploring higher levels of training by identifying the educational needs for nutrition in different sub-specialities. There is also some discussion on developing a defined clinical speciality in Nutrition. With these developments, nutritionists, dietitians and doctors with expertise in nutrition are identified as a valuable resource. Examples of key sub-specialists linked with nutrition include Gastroenterologists who are often responsible for Clinical Nutrition Support Teams. However, knowledge and skills in nutrition are relevant in many other clinical specialties. Some highly experienced doctors have been admitted to the GMC specialist register on account of their specialist knowledge and skills in nutrition. More recently the Royal College of Paediatrics and Child Health (www.rcpch.ac.uk) has started a Diploma in Paediatric Nutrition. However, in the wake of Modernising Medical Careers and the overarching role of the new Postgraduate Medical Education and Training Board (www.pmetb.org.uk), it is expected that well defined training and accreditation pathways for doctors with a dedicated interest in nutrition, will emerge from within all relevant medical specialties. In Public Health, there are new standards and revamped training, open to doctors and others with a flair for the specialty. The new syllabus includes core concepts and facts about nutrition that every public health specialist should know (www.fph.org.uk). In Westminster Forum, July 2008 4
2006 the UK Voluntary Register was opened for registration in defined areas of specialist practice, including Public Health Nutrition (www.publichealthregister.org.uk). At present, an available route to acquiring basic specialist knowledge and skills in nutrition is through an accredited Master’s degree from a UK university. These courses are usually one year full time and can also be done part-time over two to three years. Current Initiatives The work of the Council of Europe Alliance on Hospital Food and Nutritional Care has led to the “Need for Nutrition Education Project” (NNEdPro), which is funded by an educational grant and is cited in the Department of Health’s Nutrition Action Plan (www.dh.gov.uk). This project seeks to assess and enhance nutrition teaching and learning in UK Medical Schools through a national survey and pilot curriculum intervention. This is timely as the Foundation Curriculum for junior doctors (www.foundationprogramme.nhs.uk) also highlights Nutrition as an important training outcome. A project is currently also underway in Tayside, Scotland to educate and assess a pilot group of Foundation Doctors on important applied aspects of Nutrition. Voluntary Professional Registration in Nutrition The Nutrition Society (NS) (www.nutritionsociety.org) is the leading learned body for nutrition science in the UK and holds a voluntary register for individuals with recognised or accredited bioscience first or higher degrees in nutrition or an equivalent qualification (one that developed specialist competency in nutrition or public health nutrition). Some individuals can show professional competency learnt ‘on the job’ over many years. Since it first opened, the register includes surgeons, physicians, gastroenterologists, endocrinologists, paediatricians and public health doctors with special interests in academic or practical aspects of nutrition. A doctor with a degree in nutrition could be eligible to apply to join the NS register. The NS has an updated list of the courses that it accredits on its website and also provides tips on how to choose courses of study. As a first port of call, qualified doctors are encouraged to attend the ICGN Certificate Course in Human Nutrition. It is hoped that in the near future a full fledged Nutrition Faculty or College will evolve and together with the PMETB and GMC there is potential to reshape the training of doctors with a flair for nutrition. Conclusion Worldwide, in the 21st century, nutrition contributes to key millennium development goals, some left over from the 20th century. The challenges of obesity and over- nutrition, cardiovascular disease, diabetes and cancer increasingly afflict young and old in rich and low-income countries. Effective treatment and prevention will become possible once there are rewarding career pathways in clinical and public health nutrition for doctors, integral to a competent nutrition workforce that will ensure the public chooses health and achieves it too. Westminster Forum, July 2008 5
Dr Sumantra Ray RNutr* Senior Clinical Research & Teaching Fellow, Ninewells Hospital & Medical School, University of Dundee / NHS Tayside, Dundee DD1 9SY. Email: s.ray@dundee.ac.uk *Corresponding Author & Project Leader, NNEdPro BMA Lead on Hospital Nutrition (2005-7) Dr Joan Gandy RD RNutr Research Officer & Editor-in-chief, British Dietetic Association & Journal of Human Nutrition & Dietetics, 5th Floor Charles House, 148-9 Great Charles Street Queensway, Birmingham B3 3HT. Email: researchofficer@bda.uk.com Dr Jacqueline Landman RPHNutr Registrar & Head of Professional Development, Nutition Society Interim Professional Body for Nutrition, 28 Portland Place, London W1B 1DE. Email: j.landman@nutsoc.org.uk Westminster Forum, July 2008 6
You can also read