FROM PRIMARY HEALTH CARE TO UNIVERSAL HEALTH COVERAGE - BARBARA MCPAKE INSTITUTE FOR INTERNATIONAL HEALTH AND DEVELOPMENT, QUEEN MARGARET ...
←
→
Page content transcription
If your browser does not render page correctly, please read the page content below
From Primary Health care to
Universal Health Coverage
Barbara McPake
Institute for International Health and
Development,
Queen Margaret University, EdinburghJulius Nyerere Philosophy to focus on
Arusha declaration 1967: ‘villagisation’; community
participation, bringing health care
Ujamaa, socialism and self- to rural populations, ‘appropriate
reliance technology’ for health care
‘We must not again be
temped by offers of big new
hospitals with all the costs
involved until at least every
one of our citizens has a
basic medical service readily
available to him.’ (Nyerere
quoted in Morley and Lovel,
1986)Primary health care in China • Roots back to 1930s pre-communist era • Post 1948 rural China organised on basis of co-operatives: each paid a levy to fund basic health care for its members • Early model of primary health care delivered through ‘barefoot doctor’ system • Barefoot doctors were secondary school graduates, given 6 months training at a local hospital • Promoted basic hygiene, preventive health care, family planning and treated common illnesses www.qmu.ac.uk/iihd
Primary Health Care Alma Ata 1978 134 nations represented. Virtually all signed up to: ‘Health for All by the Year 2000’
7 elements of PHC: ‘PHC includes at
least…’
• Health education
• Promotion of food supply and nutrition
• Promotion of safe water and basic sanitation
• Maternal and child health care including family
planning
• Immunisation
• Prevention and control of infectious and common
diseases and injuries
• Essential drugs
wwwm.qmu.ac.uk/iihd‘Selective’ versus ‘Comprehensive’ PHC
• After Alma Ata, Walsh and Warren (1979)1
immediately respond to Alma Ata – a heated
debate about how to do PHC and what it
really means:
– A selected list of cost-effective interventions
– Or a revolutionary new approach to locating
authority over health in communities and
households based on community participation,
appropriate technology and democratisation
1Walsh J A & Warren K S. Selective primary health
care: an interim strategy for disease control in
developing countries. N. Engl. J. Med. 301.967-74.• Explicit consensus in 1978 on the primary health care approach • Ideological warfare on what it really means • Implicit consensus on a public health system to deliver it • Not much discussion until 1987 on the public- private mix of financing and provision
Health expenditure per capita: $PPP, 2008 (WHOSIS)
USA
Malta
France
Iceland
Greece
Portugal
Qatar
Lithuania
Botswana
Bulgaria
Turkey
Maldives
Mauritius
Grenada
Libya
Ecuador
Georgia
Peru
Moldova
Tuvalu
Viet Nam
Vanuatu
Uzbekistan
Syria
Ghana
Sierra Leone
Chad
Papua New Guinea
Benin
Malawi
Mozambique
Eritrea
0 1000 2000 3000 4000 5000 6000 7000 8000Health expenditure (as previous slide) compared to GDP per capita
(IMF, 2010; international $)
USA
Malta
France
Iceland
Greece
Portugal
Qatar
Lithuania
Botswana
Bulgaria
Turkey
Maldives
Mauritius
Grenada
Libya
Ecuador
Georgia
Peru Global GDP 2010 = US$51,067,937,268,701.1
Moldova Global population 2010 = 6,885,217,727
Tuvalu Average GDP/capita = $7,417
Viet Nam US health expend/capita = $8,233
Vanuatu (World Development Indicator data)
Uzbekistan
Syria
Ghana
Sierra Leone
Chad
Papua New Guinea
Benin
Malawi
Mozambique
Eritrea
0 10000 20000 30000 40000 50000 60000 70000 80000 90000 100000Universal health coverage: From Agenda for Reform to WHR 2010
Agenda for Reform • Advocated for greater roles for out-of-pocket payments (user charges) and private sector provision and insurance • This advocated in part as a strategy to support primary health care
“Reallocating resources away from hospital care is not easy. It is physically impossible to turn a few large and costly hospitals into many small primary-level health care units or to turn a nation’s highly trained doctors and nurses into less trained and less expensive primary health care workers. . . . It is the financing of expensive hospital care that needs change, not the existence of the care as such. Governments must find ways to charge those who are able to pay for the benefits of public provided curative care.” (p18)
• But – interpreted as generalised prescription
of privatisation and user fee introduction
• Waves of countries introduced and increased
fees in late 1980s and 1990s
• Experience:
– negative demand effects measured in multiple
contexts;
– argument that fees required to improve quality
sustained in only a few projects
– Little revenue raised in relation to global funding
level
– Revenues raised could be important at local levelThe Bamako Initiative 1987- • A plan for self-sustained primary health care in African villages • Communities share in the financing of local health services by buying drugs above the wholesale purchase price and using the proceeds to maintain drug supplies and subsidize services • This core element known as a ‘revolving drug fund’ • Benin, Rwanda, Guinea and Mali scaled up this initiative as the basis of their national rural primary health care strategy • In other countries, it remained a project operating in a few localities • Main critique has been affordability of charges for poor families
Experience of out of pocket payments Source: Poullier et al. (2002) Patterns of global health expenditures: results for 191 countries, EIP/HFS/FAR Discussion Paper No. 51, Geneva, World Health Organisation.
Source: Xu et al. (2007) Household catastrophic health expenditure: a multi-country analysis, Lancet, 362, 111- 117
• On the basis of mounting evidence of:
– Significant negative demand side effects of user
charges
– Limited contribution to overall financing
– Limited success with ‘scaling up’ community financing
to support a national PHC system
– Associations of out of pocket payments with
catastrophic health expenditure
• Wave of reforms from late 1990s that removed
user fees and supported ‘free health care’
• Has support for ‘demand side’ (fee removal) been
matched by support for ‘supply side’?5 country case study of fee removal: Ghana, Nepal, Sierra
Leone, Zambia, Zimbabwe
• User fee removal will probably:
– Increase use of health services
– Remove staff bonuses that have been paid from revenues
– Reduce ability of facilities to restock basic medicines with their
own resources
• So needs to:
– Be offset by budget increases that can fill these gaps
– Be accompanied by human resource policies that ensure there
is capacity to meet increased demand
– Find ways of mimicking the incentives to encourage more
demand that user fees present
• Case studies
– Demonstrated importance of the supply side balance
– Showed that attempts to enact supporting supply side measures
were variable across the countries and had mixed success
Source: McPake et al., 2011World Health Report, 2010 www.qmu.ac.uk/iihd
Case study 1: China
Health system post-1981
• The commune system, rural co-operative medical system and
barefoot doctor programme all ended in 1981
• Coverage of RCMS dropped from 90% to 5% in 1984
• In the economy, shift towards individual production in family
units
• In the health system, there was an effective privatisation
• In public health units, health workers incomes were dependent
on sale of services under system of regulated prices
• Strong perverse incentives – health workers recommended
lucrative interventions and failed to offer access to cheaper
ones
www.qmu.ac.uk/iihdCurrent reforms
• 850 bn. Yuan (US$124bn) to public funding of a
‘basic health system’
• Diversified systems of insurance differentiate
entitlements of urban employees, other urban
residents and rural residents
• Direct investment in expanded public services –
managed directly within government
• Strengthening referral and supervision systems
• Major programme of experimentation in delivery
systems and payment mechanisms to inform further
reform
www.qmu.ac.uk/iihdChinese health insurance schemes in 2010
Urban Employee Urban Resident New Cooperative
Basic Medical Basic Medical Medical Scheme
Insurance Insurance
Target population Formal sector Children, students, Rural residents
urban workers elderly, unemployed
and migrants
Financing
Premium (Y) 1559 138 157
Govt. subsidy 0 120 120
Benefits
Inpatient reimbursement (%) 68 48 44
Total reimbursement ceiling Six times average Six times disposable Six times income
wage income of local of local farmers
residents
Source: Yip et al. (2010) Early appraisal of China’s huge and
complex health-care reforms, Lancet, 379, 833-42Early evaluation of the reforms
• Successful in achieving high levels of coverage
through diversified systems of insurance: 835m
enrollees; 90% population has coverage
• But – premised on a narrow ‘package of care’ –
limited coverage of inpatient care and significant
copayments
• Major inefficiencies remain – difficulties enforcing
essential drugs list; hospitals remain dominant in the
system
• Considerable problems of quality, and human
resource shortages to be tackled in second wave of
reform – have to start with primary care
www.qmu.ac.uk/iihdWorld Health Report, 2010 www.qmu.ac.uk/iihd
Case study 2: Ghana
Background to health financing and social health
insurance in Ghana
• User fees abolished at independence, reintroduced in 1969
and increased in 1985 and again under ‘cash and carry’ in
1992; by mid-1990s fees accounted for 70-80% of non-salary
operating budgets
• Delivery exemption policy piloted 2003; extended nationwide
2004 in response to persisting high MMR and inequities in
access to ANC and SBA
• 1990s: Mutual health organisations established: external
funding; covered mainly high cost inpatient care
• NHIS promised by successful New Patriotic Party in 2000
elections – objective of removing financial barriers to access
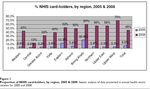
• Passed into law 2003; implementation began 2005Main features of NHIS in Ghana (Witter and Garshong, 2009) • Sources of funding: NHIL=2.5% VAT; payroll deductions (2.5%) formal sector employees; public subsidies; mandatory income based premia for informal workers • District-based mutual health insurance schemes (DMHIS) developed out of MHOs – each district to have one; manage informal sector involvement • Membership mandatory; risk pooling across district schemes • Exempt groups, but tightly defined • Broad minimum package of care • Accreditation of providers • Reimbursement on a modified ‘diagnosis related group’b basis
Source: Witter and Garshong, 2009
Composition of enrolment • Largest share of enrollees (about two thirds) are exempted from making contribution (pregnant women exempted in 2008, children of members are main groups; also indigent, elderly) • Registrations among informal sector workers are quite low (16% of the eligible population in 2008) • In 2009 30% of households were currently enrolled in the NHIS, 14% had previously been enrolled and 56% had never enrolled. Richer households were significantly more likely to enrol than poorer households, • There was higher enrolment in rural (19%) than urban (11%) areas (may relate to history of MHOs), but urban members more likely to renew. Sources: Jehu-Appiah et al., 2011; Witter and Garshong, 2009
Evaluation in 2008
• Increase in access and decrease in out-of-pocket
expenditure for members – but no improvement in use of
maternal care
• Financial sustainability has been major issue – end of 2008
about $34m owing to health facilities – in part because new
members are not paying premia and funding increases have
not been commensurate
• Money follows infrastructure? A hospital with a laboratory
can bill for more services than a health centre without one
– hence resources are skewed towards better endowed
areas
• Reports of informal payments being levied – perhaps
because staff have experienced growth in workload without
compensation
Source: Witter and Garshong, 2009?
World Health Report, 2010
www.qmu.ac.uk/iihdCase study 3: Thailand
Health insurance system in Thailand
• 3 systems of health insurance
– Civil service medical benefit scheme (est. 1980)
– Social Security scheme (est. 1990)
– Universal coverage scheme (completed 2002)
• Succeeded the Medical Welfare Scheme (1975-)
• Voluntary health card scheme (1983-)
• 30 baht scheme=5% of population (20% population uninsured 1998): Antos, 2007
Efficiency measures incorporated into
UC scheme
• Capitation payment method
• Primary care gatekeepers
• HiTAP evaluates components of the package
of care on cost-effectiveness criteria
• Separation of purchaser and providerEquity features of Thai system • UC has increased progressivity of health financing system • Fewer Thai households faced with catastrophic health expenditure
Percent distribution of net government health subsidies among
different income quintiles in 2001 and 2003
A comparison of percent distribution of net government health subsidies among different
income quintiles in 2001 and 2003
35
31
30 28
25 22
20
percent
20 17 18
17 16 2001
15 15
15 2003
10
5
0
Q1 Q2 Q3 Q4 Q5
Income quintile
Note: The concentration index of government health subsidies in 2001 was -0.044 and in 2003 was -0.123
Source: International Health Policy Programme,
Thailand, 2007)Concerns about the Thai system • Significant gaps in benefit coverage under UC • Capitation rate paid may be too low and providers may under-provide care • Some hospitals are accruing significant levels of debt • BUT – the total cost of the system is currently 3.5% of GDP – might be considered space to resolve these problems
World Health Report, 2010 www.qmu.ac.uk/iihd
Conclusions
• Reaching universal coverage is an ever more difficult task –
challenges world’s richest economies; most difficult for
LICs; case studies have been MICs (but look at Rwanda for a
good LIC case study, though heavily donor subsidised)
• Universal coverage is not only about financial accessibility –
cannot be achieved without attending to the efficiency of
the health system
– Focus on a cost-effective package of care
– Use payment mechanisms that structure incentives towards
efficiency for both providers and users
– Concentrate on strengthening primary health care system
• Thai model accepts heterogenous system albeit with
universal access to the basics – may be needed response to
highly heterogenous population
• No quick fixesYou can also read