Il bambino e il dolore - Dr. Pablo M. Ingelmo
←
→
Page content transcription
If your browser does not render page correctly, please read the page content below
Prevalence
Source of chronic pain Prevalence per
100000
Dysmenorrhoea 7200-7900
Knee pain 3900-18500
Back pain 2800-7800
Migraine headache 1400-37000
Recurrent abdominal pain 6000-15000
Recurrent limb pain 4200-33600
McGrath PA. Epidemiology of Pain. IASP Press, Seattle, 1999: 81-101Children with chronic pain
Aged 5–23 ys: 62 % reported continuing pain
Females were significantly more likely to report
continuing pain, use of health care, medication
and non-drug methods of pain control
Continuing pain associated psychosocial
factors: females 76 %, males 21 %
Pain episodes increased with age
Martin A. Pain 2007, 128: 13–19Painful procedures can be harmful
When babies’ pain was high, mean AOPP and TH blood
levels increased significantly
Even common routine procedures can be potentially
harmful for the newborn if they provoke a high level of pain
Bellieni CV. PAIN 2009 ; 147: 128–131Pain in Neonates: Consequences
Altered pain sensitivity (may last into adolescence)
Permanent neuroanatomic and behavioral abnormalities
Emotional, behavioral, and learning disabilities
Altered pain sensitivity can be ameliorated with effective
pain relief
PEDIATRICS 2009; 118: 2231-2241Out-of-hospital pain
Acute pain: 37%, Intense to severe: 67%
Trauma associated with acute pain: OR 818
Analgesia: 84% experienced some pain relief
On arrival at hospital 67% still in pain
Galinski M. American Journal of Emergency Medicine 2010A very big problem…ED
Admission: 1/10 severe pain , 1/4 severe distress
4/10 received analgesics in ED
1/5 worsening of pain, 1/4 pain remained the same
1/10 prescription for analgesics at discharge.
1 week after discharge: 1/20 pain; 1/3 distress
Physical restraint of struggling children during painful
procedures, ‘‘brutacaine’’, should no longer be an
acceptable part of modern practice
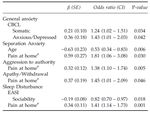
Johnston C. Pediatric Emergency Care 2005; 21: 342-346Adverse events in childhood and
chronic widespread pain in adult life
Increased risk of CWP
Road traffic accident : RR 1.5 (1.05–2.1)
Resided in institutional care: RR 1.7(1.3–2.4)
Maternal death: RR 2.0(1.08–3.7)
Familial financial hardship: RR 1.6 (1.3–1.9)
Jones GT. PAIN 2009; 143: 92–96Pain after ADT
Fortier MA. Pediatrics 2009Maladaptive behavior change
Fortier M. Pediatric Anesthesia 2010 20: 445–453Mommy and daddy
Parents are actually more likely to
undermedicate than overmedicate
Parents tend to withhold pain medication,
even if they assess their child as having pain
Parents may not recall analgesia instructions
(or any instructions)
Fathers, more often than mothers, seem to
have misleading perceptions of the nature
and adverse effects of children’s analgesics
Yaster M. 1994; Capici F 2007Dolore Postcraniotomia
OR 95% CI p
Inadequate pain control
General Hospital (vs Ped.H) 5.0 1.2-20.2 0.02
Pain Crisis
General Hospital (vs Ped.H) 8.2 0.9-70.2 0.02
Inhalation Anaethesia (vs TIVA) 30.0 3.4-264.8 0.05
Brain Pain Study Group ASA 2011Cognitive development
0 to 2 years: fear, anger, idiosyncratic words, somatic
localization Behavior
2 to 6 years: concrete and magic thinking, simple
conceptual words Self report +/- Behavior
7-10 years: external causation, symptoms, pain and
illness. Cognitive strategies Self report
11 to 18 years: Pain experiences and explanations in
adults terms Self report
Stanford EA. Pain 2005, 114: 278-284Paediatric pain assessment at the ED
Paediatric pain management which may need to be based upon
the children’s or parent’s assessment rather than that of the
nurse
Rajasagaram U. Journal of Paediatrics and Child Health 2009; 45:199–203Associazione Italiana Emato-Oncologia
Pediatrica
“ …almeno la prima puntura lombare e/o aspirato
midollare nei bambini con patologia oncologica
dovrebbe essere effettuata in sedazione”….
La presa in carico globale del bambino leucemico. Ponte di Legno Working Group 2001Procedure senza sedazione: PAURA !!!
3 e 8 anni 9 e 12 anni
Senza Con Senza Con
Sedazione Sedazione sedazione Sedazione
(n 16) (n 20) (n 20) (n 18)
Paura pre procedura 15 4 13 2
(molta o moltissima)
Paura post procedura 8 1 5 0
(molta o moltissima)
Dolore procedura 14 1 11 0
(forte o insopportabile)
Bosatra M.SARNePI 2007Sentimenti dei genitori
Senza sedazione Con sedazione
n 48 n 54
Impotenza 16 (32%) 18 (32%)
Paura 14 (30%) 16 (30%)
Sofferenza 10 (20%) 0 (*)
Rabbia 5 (11%) 2 (4%)
Sconforto 2 (8%) 4 (8%)
I genitori hanno sempre paura quando i loro figli
vengono sottoposti a procedure dolorose
Bosatra M.SARNePI 2007Pharmacologic pain management
By the ladder
• By the clock
• By the mouth
• By the child
PAIN IN PEDIATRIC ONCOLOGYClinical situations
Infection
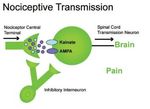
Nociceptive Neuropathic
Postoperative
Psychogenic
Phantom pain
A child with sarcoma may have A child with an meningococus infection
nociceptive pain from bone may have nociceptive pain because of
metastasis, neuropathic pain from tissue necrosis, acute postoperative
tumor growth in a nerve plexus and pain and phantom pain after the leg
considerable psychological stress. amputation.Pediatric therapy
Few well-designed RCT: case reports, case series
Therapy extrapolated from adult data
Combined pharmacological regimens
Slow titration to minimize side effects.
Anticipatory guidance regarding side effects
Trade-off between pain control/side effects.
Berde CB. et al. NEJM 2002,347: 1094-03Interdisciplinary Team
Better physical and psychological functioning.
Return to “normal” activity, oppioids consuption,
medical attention.
Negative outcome by not providing full integrated
interdisciplinary pain care
Pediatrician, oncologist,
Anesthesiologist, Physical therapist, Psychologist
Flor H. Pain 1992; 49: 221-230 Robbins H. Anesth Analg 2003; 97: 156-162We have a PROBLEM !!!
A responsibility of physicians who care for children is
eliminating pain and suffering when possible.
Available tools: to evaluate and treat acute pain in
children using low-cost and safe methods.
A substantial percentage of children have been
undertreated
It’s an adult responsibility to help children with pain
Is not a children responsibility to convince adults to
give them analgesics whenever they need them….
AAP/APS Pediatrics 2001, 108: 793-797Grazie
Psychological therapy
Relaxation, biofeedback, cognitive behavioral therapy
(distraction, imagery, transformation), exercise
therapy.
NNT 2.3: headache, recurrent abdominal pain, sickle
cell pain
CRPS-I: T°/EMG biofeedback + exercise therapy
Experienced psychological and medical personnel
.
Lee BH. J Pediatr 2002; 141: 135-140 Eccleston C. Pain 2002, 99: 157-165Pain clinicians and GPs
Lack of adequate training and resources available to pain
clinicians and GPs for managing chronic pain in children
Setting up chronic pain programs in existing pediatric
centers
Bathia A. Pediatric Anesthesia 2008 18: 957–966Venipuncture and IV cannula insertions
Most common sources of pain in hospitalized children.
IV cannula: second most common cause of the worst pain
experienced during hospitalization (second only to pain relatedto the
patient’s underlying disease).
In the absence of premedication or psychological interventions, high
levels of distress during venipuncture were reported in 50% of the
children.
High levels of distress: 83% 2–6 ys, 51% 7–12 ys, 28% adolescents
Needle phobia: a true medical condition present in up to 10% of the
population (Diagnostic and Statistical Manual of Mental Disorders)
Kenedy RM. Pediatrics 2008;122;S130-S133Much pain, low gain…..
Preterm infants given fentanyl in addition to
nitrous oxide had significantly lower hormonal
responses to surgery for ligation of the patent
ductus arteriosus than did infants who did not
receive fentanyl.
Neonates who received high-dose sufentanil
compared with halothane-morphine had
improved survival rates after cardiac surgery.
Anand KJ Lancet. 1987;1(8524):62–66 Anand KJ. N Engl J Med. 1992;326(1):1–9Shoud I pay o should I Wait…
for a painless IV ctheter placement
Parents would be willing to spend additional time in
the ED and incur additional expense to make a
hypothetical IV placement in their child painless
Walsh B. Pediatric Emergency Care 2006; 22: 669-703Consigning ‘‘BRUTACAINE’’ to history
2 + 2 +1
Half of UK EDs use modern
pharmacological methods of
procedural pain control
There is still considerable
potential to improve the
management of pain in children.
Physical restraint of struggling children during painful
procedures, ‘‘brutacaine’’, should no longer be an
acceptable part of modern practice
Loryman B. Emerg Med J 2006;23:838–840Pediatric vs adult pain control
Cause of pain
Acute leukaemia or a brain tumour.
Pain mainly therapy-associated
75% of adult cancer patients experiencing pain
suffer from carcinoma.
Adult pain is mainly due to progressive tumour
growth (15% antineoplastic therapy pain)
Ljungman 2000, Zech 1995Genitori durante la procedura
Senza sedazione Con sedazione
n 48 n 54
Contenzione fisica durante 34 (71%) 5 (9%)
procedura
Contenzione fisica dopo 41 (85%) 24 (44%)
procedura
Ruolo riassicurante 23 (48%) 38 (70%)
Aiuto al personale 9 (20%) 11 (20%)
Impedimento al personale 2 (4%) 2 (4%)
Bosatra M.SARNePI 2007You can also read