The Triple Aim's Missing Link: Meaningful Engagement for Patients with Chronic Conditions
←
→
Page content transcription
If your browser does not render page correctly, please read the page content below
Volume 27, Number 15 • August 1, 2014
The Triple Aim’s Missing Link: Meaningful Engagement
for Patients with Chronic Conditions
Amy Bucher and Raphaela O’Day
What will it take to optimize health system per- time in an appointment to fully explore the
formance and, most critically, patient outcomes? patient’s health concerns, the hard work of
The Triple Aim is the Institute for Healthcare changing behaviors happens outside the office.
Improvement’s (IHI’s) answer to this question Patients and their caregivers are the ones who
and encompasses three areas of improvement: must live into dietary and activity changes, take
medications and measure biometric progress,
• the patient experience, as measured both and pay attention to the day-to-day details of
through quality and satisfaction; their health. Unless the patient is fully engaged
• population health, as measured by out- in his or her own health, the Triple Aim cannot
comes; and fully achieve its objective.
• reduction of cost.
The Triple Aim and the Polychronic Patient
While each pillar of the Triple Aim is clearly To be clear, the systemic issues that the Triple
essential for optimal performance and out- Aim is intended to address are significant.
comes, we argue that there is a fourth, equally Patients with chronic conditions represent a
critical pillar: engaging the patient in the sys- large segment of the population, with 53.9
tem of care. percent of all patients seen in the United States
in 2010 having at least one chronic condition
Although the health care system clearly offers and 39.5 percent having two or more.4 These
opportunity for improvement, we believe that patients accrue significant health care costs. In
much of the real work of improving health out- 2013, Oliver Wyman determined that although
comes takes place outside of the system, within polychronic patients — people with multiple
the patients’ daily lives. Data indicate that pro- chronic conditions — represent only 5 percent
viders may spend no more than 12 percent of of the total U.S. population, they drive 45 per-
their total work time interacting directly with cent of health care costs,5 due to factors such
patients,1 with an average patient visit length as emergency room (ER) visits and overutiliza-
of just over 20 minutes in 2010.2 Although no tion of services.
clear relationship between provider visit length
and patient outcomes has been established, it Once a person has been diagnosed with
is clear that patient satisfaction drops when four or more chronic conditions, his or her
provider visits are shorter.3 health care expenditures soar to over seven
times the national average.6 With the passage
Even in the best case-scenario where patient of the Affordable Care Act (ACA) and its
and provider spend an adequate amount of provisions for outcome-based reimbursement,Page 2 ■ Managed Care Outlook ■ August 1, 2014
health systems have a vested interest in helping progress, and feel understood and accepted.
patients succeed at living into the recommen- When these needs are supported by the system,
dations of their providers and complying with patients are more likely to feel motivated and
instructions. engage in positive health behaviors.
The interventions that currently exist within We sometimes speak of patient motivational
health plans and systems to help people cope levels as if they range from low to high, with
with chronic conditions suffer from a set of highly motivated patients being the ones to
common problems. Delivering high-touch show engagement in health. The reality is
coaching or counseling is extremely high cost. slightly more complex. We also should con-
Because of human capital and other resource sider motivational quality, which speaks to
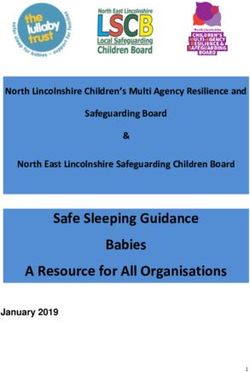
constraints, it is also not scalable. And, as more the factors underlying a person’s motivation.
and more members suffer from polychronic Motivational quality can range from the totally
conditions, the cost and scalability issues extrinsic to the totally intrinsic. (See Figure 1)
intensify. Finally, it is difficult to get members
to engage with interventions outside of the In general, intrinsic motivators are more
doctor’s office. likely to sustain long-term behavior change.11
In between those two extremes are introjected
Although financial incentives can increase motivation (e.g., the internalized nagging voice
initial participation in programs such as health reminding you of what you “should” do), iden-
risk assessments,7 the impact of these incen- tified motivation (in which a behavior is consis-
tives does not typically sustain behavior change tent with other goals you have), and integrated
in the long term.8 Moreover, patients who are motivation (in which a behavior is part of your
not engaged in their own care incur up to 21 identity). In general, by supporting people’s
percent higher health care costs than their basic needs of autonomy, competence, and
more engaged counterparts.9 For the Triple relatedness, we can help them find motivators
Aim to succeed, we must find a way to improve closer to the intrinsic side of the motivation
patients’ sustained engagement with their spectrum, and in that way help promote sus-
health over time. tained behavior change.
Engaging Patients How Digital Health Coaching Brings
When patients are engaged with their health, Patient Engagement to Life
they feel a sense of ownership over it. The The application of this theoretical approach
engaged patient collaborates with providers and has been coined “motivational design.” The
supporters (such as friends or family mem- beauty of motivational design is that, as an
bers) to achieve desired health and personal approach, it can be applied to any type of
outcomes. Engaging patients to become active health intervention, including face-to-face
participants in the health care process requires encounters as well as digital program design.
understanding both individual motivations for In our HealthMedia® Digital Health Coaching
change as well as supporting the members’ holis- programs at Johnson & Johnson Health and
tic medical, emotional, and daily living needs. Wellness Solutions Group, we strive to bring
these underpinnings of patient engagement to
Psychological theory and research suggest life. Here’s how.
that an engaged patient is being supported in
three fundamental needs. According to Self- Autonomy: Supporting a patient’s autonomy
Determination Theory,10 people share basic means giving the person as much choice as pos-
needs for autonomy, competence, and related- sible, often within a set of constraints
ness. That is, patients must have some sense (e.g., losing weight nearly always requires
of control over their health experience, believe limiting calorie intake). A person feels auton-
in their ability to take action and experience omy support when behaviors are presented inAugust 1, 2014 ■ Managed Care Outlook ■ Page 3
Figure 1:
Types of Motivation
[More likely to engage in and sustain behavior change]
Amotivated External Introjected Identified Integrated Intrinsic
I am not My employer/ I know I The behavior is The behavior The behavior
motivated doctor/coach should consistent with is part of my feels good
told me I my goals identity
need to
Controlled Autonomous
Adapted from Segar & Hall. Think Intrinsic Motivation is the Holy Grail of Exercise Participation?
Think Again. Society of Behavioral Medicine Annual Conference, April 29, 2011.
Ryan & Deci (2000) American Psychologist, 55(1), 68–78.
a way that allows them to express volitional Human beings are naturally hardwired to
choice. That is to say, even if the person does want to experience growth and success. Tactics
not enjoy the specific behavior, he or she sees it to help them do that include offering posi-
as a stepping stone to reach a larger goal that tive feedback when a behavior is aligned with
he or she does value. A person who really wants the goal, timely and specific feedback when
to lose weight for intrinsic reasons will be more a behavior is inconsistent with the goal, and
engaged in selecting a low-calorie meal each sequencing learning of skills logically and
day than a person whose only reason for losing transparently so that a person is more likely
weight is to satisfy a nagging spouse. to experience success as he or she tackles
the list.
In the context of Digital Health Coaching,
then, the first step to supporting autonomy is Within Digital Health Coaching, we high-
helping the user create a framework for voli- light a user’s areas of success, no matter how
tional choice. We begin the coaching experience small. Especially for a polychronic patient
by stepping the user through the process of who may feel overwhelmed by constant
thinking about important personal goals and negative health feedback, acknowledging the
values. These values are then threaded through things that are going right can be a powerful
the program experience to highlight how motivator. We also strive to make construc-
individual health behaviors contribute to the tive feedback timely and specific, particularly
achievement of the overall goal. At every point through tools such as Track Your Health,
in the Digital Health Coaching experience, the which provide granular activity data. Finally,
user is kept mindful of his or her personal goals the assigned activities within coaching are
and values as a way to promote autonomous tailored to the individual user’s beginning
choice. state and eventual goal; they are designed
to be appropriately challenging and get
Competence: Supporting someone’s compe- more so over time as the user makes health
tence means helping them learn and achieve. improvements.Page 4 ■ Managed Care Outlook ■ August 1, 2014
Relatedness: Supporting a user’s sense of Conclusion
relatedness requires conveying warmth and The Triple Aim is a worthwhile endeavor
positive regard. People who feel recognized as that, if achieved, will not only save costs
individuals, whose personal characteristics are across the American health care system but
acknowledged and positively regarded, feel sup- also improve the quality of life for millions
ported with respect to relatedness. Relatedness of patients. In order to get there, we need to
also can be supported by conveying belonging- consider the missing link of patient engage-
ness to a relationship or a larger group. ment: helping patients to take ownership of
their own health behaviors for the long term.
In Digital Health Coaching, our tailor- We believe that engaging patients requires a
ing technology is the cornerstone of how we deep understanding of what motivates behav-
support relatedness. The program content is ior change, including fundamental human
highly personalized based on each individual needs to be autonomous, competent, and
user’s data. The unique combination of both related. If we keep these considerations at the
condition-specific and psychographic user data forefront when designing interventions and
including readiness for change, motivation, self- interacting with patients, we can help advance
efficacy, and personal barriers to change are the Triple Aim.
foundations to delivering the right information,
in the right way, and at the right time to sup- Amy Bucher, PhD, Associate Director, Behavioral
port behavior change. Science, works as a member of the Behavioral
Science and Data Analytics Group at Johnson &
Research on tailoring shows that people Johnson Health and Wellness Solutions Group, with
who read tailored content show brain activ- a focus on grounding digital health coaching program
ity in the neural structures associated with content, design, and functionality with behavioral-
memory and self-relevance.12 This suggests that science based approaches. Her research interests
the personalized content is in fact triggering a include motivational design, patient and user engage-
sense of relatedness. Digital Health Coaching ment, happiness, and social relationships and their
also supports relatedness by emphasizing users’ influence on health and well-being. Dr. Bucher re-
membership in social groups, whether it be by ceived her AB magna cum laude in psychology from
coaching them through communication tech- Harvard University and her MA and PhD in organiza-
niques and social support strategies for family tional psychology from the University of Michigan.
and friends or by sharing normative feedback
that helps users understand how other poly- Raphaela O’Day, PhD, Behavioral Scientist, is a
chronic patients like them cope with health member of the Science and Innovation team at
behavior change. Johnson & Johnson Health and Wellness Solutions
Group. She has primary responsibility for develop-
The outcomes associated with Digital Health ing participation and engagement strategies that are
Coaching suggest that motivational design grounded in behavioral science and support sus-
can help engage patients, including those with tained behavior change. She received her Bachelor of
multiple chronic conditions. The Johnson & Science degree in Human Physiology, with an addi-
Johnson HealthMedia® CARE® For Your tional focus in Psychology from Michigan State Uni-
Health program, which addresses management versity, her MA in School and Community Psychology,
of chronic conditions, has been found in two specializing in Marriage and Family Therapy, and her
peer-reviewed studies to significantly reduce PhD in Educational Psychology, with a concentration
medical utilization costs in a health system in Neuroscience from Wayne State University. ■
setting.13 This is in addition to a body of self-
report outcomes that suggest improvements Endnotes:
in doctor-patient communication, medication 1. Block, L., et al. (2013). In the wake of the 2003
adherence, and other critical factors in condi- and 2011 duty hours regulations, how do internal
tion management. medicine interns spend their time? Journal of GeneralAugust 1, 2014 ■ Managed Care Outlook ■ Page 5
Internal Medicine, 28(8), 1042-1047. Doi: 10.1007/ 9. Hibbard J., Greene J., & Overton V. (2013). Patient
s11606-013-2376-6. Activation and Health Care Costs: Do More Acti-
2. www.cdc.gov/nchs/data/ahcd/namcs_summary/2010_ vated Patients Have Lower Costs? Health Affairs.
namcs_web_tables.pdf 32(2): 216-222.
3. Dugdale, D. C., Epstein, R., & Pantilat, S. Z. (1999). 10. Ryan, R. M. & Deci, E. L. (2000) Self-determination
Time and the patient-physician relationship. Journal theory and the facilitation of intrinsic motivation,
of General Internal Medicine, 14(Suppl 1), S34-S40. social development and well-being. American
Doi: 10.1046/j.1525-1497.1999.00263.x Psychologist, 55, 68-78.
4. www.cdc.gov/nchs/data/ahcd/namcs_summary/2010_ 11. Deci, E. L., & Ryan, R. M. (2000). The ‘what’
namcs_web_tables.pdf and ‘why’ of goal pursuits: Human needs and the
5. www.ehcca.com/presentations/acosummit4/ self-determination of behavior. Psychological Inquiry,
bonnette_t4_1.pdf 11, 227-268.
6. Machlin, S.R. & Soni, A. (2013). Health care expendi- 12. Chua, H. F., Polk, T., Welsh, R., Liberzon, I., &
tures for adults with multiple treated chronic condi- Strecher, V. (2009). Neural responses to elements
tions: Estimates from the medical expenditure panel of a web-based smoking cessation program.
survey, 2009. Preventing Chronic Disease, 10, 120172. Studies in Health Technology and Informatics,
Doi: 10.5888/pcd10.120172. 144, 174-177.
7. Serxner, S., Anderson, D. R., & Gold, D. (2004). 13. Schwartz, S. M., Mason, S. T., Wang, C., &
Building program participation: Strategies for recruit- Pomana, L., Hyde-Nolan, M., & Carter, E. (2013).
ment and retention to worksite health promotion pro- Sustained economic value of a wellness and disease
grams. The Art of Health Promotion, March/April, 1-6. prevention program: An 8-year longitudinal evalua-
8. Volpp, K.G., et al. (2008). Financial incentive-based tion. Population Health Management. DOI: 10.1089/
approaches for weight loss: A randomized trial. Jour- pop.2013.0042. Schwartz, S. M., Day, B., Wildenhaus, K.,
nal of the American Medical Association, 300(22), Silberman, A., Wang, C., & Silberman, J. (2010). The
2631-2637. Volpp, K.G., et al. (2009). A randomized impact of an online disease management program on
controlled trial of financial incentives for smoking medical costs among health plan members. American
cessation. The New England Journal of Medicine, Journal of Health Promotion, 25(2), 126-133. Doi:
360(7), 699-709. 10.4278/ajhp.091201-QUAL-377.
Copyright © 2014 CCH Incorporated. All Rights Reserved.
Reprinted from Managed Care Outlook, August 1, 2014, Volume 27, Number 15, pages 1, 3, 5–8
with permission from Aspen Publishers, Wolters Kluwer Law & Business, New York, NY,
1-800-638-8437, www.aspenpublishers.comYou can also read