Dr Richard Laing Respiratory Physician St Georges Hospital Christchurch 7:00 - 7:55 GSK Breakfast Session - Hot Topics in Airways Disease ...
←
→
Page content transcription
If your browser does not render page correctly, please read the page content below
Dr Richard Laing
Respiratory Physician
St Georges Hospital
Christchurch
7:00 - 7:55 GSK Breakfast Session - Hot Topics in Airways Disease
Asthma/Severe Asthma and BronchiectasisHot topics in Airways Disease:
Asthma/Severe Asthma and
Bronchiectasis
Dr Richard Laing
Respiratory Consultant
Canterbury District Health BoardConflict of Interest Employee of Canterbury District Health Board Member of the Thoracic Society of Australia and New Zealand I have not received any payment from GSK to conduct this talk. I am not GSK employee and do not hold shares in GSK. Any opinion expressed during this presentation is my own opinion and may not be that of GSK.
Overview Severe asthma or difficult to treat asthma How to identify When to refer What we can do Asthma and pregnancy Bronchiectasis what do I do in the absence of evidence?
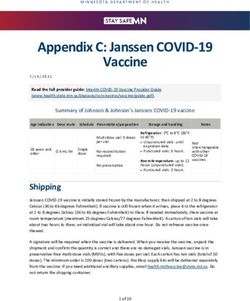
GINA – Stepwise escalation of
asthma therapy
Disease severity
Step 5
Step 4 Refer for
add-on
PREFERRED Step 3 Med/hig treatment
CONTROLLER Step 1 Step 2 h
e.g.
anti-lgE
CHOICE Low dose ICS/LAB
Low dose ICS ICS/LABA A
Med/High dose High dose
Other Consider Leukotriene receptor antagonists ICS Low dose ICS+LTRA Add low
controller low dose (LTRA) ICS+LTRA (or + dose OCS
options ICS Low dose theophylline* (or + theoph*) theoph*)
As-needed SABA or low dose
RELIEVER As-needed short-acting beta2-agonist (SABA)
ICS/formoterol**
Global Initiative for Asthma. Pocket Guide for Asthma Management and Prevention; 2016. Available from: https://www.ginasthma.org/. ICS, inhaled corticosteroid;
LABA, long-acting β-agonist; LTRA, leukotriene receptor antagonists; OCS, oral corticosteroid; SABA, short-acting β2-agonistWhat are your options when
uncontrolled on an ICS?
Asthma Symptoms not controlled on
Inhaled Corticosteroid (ICS)
OR
Option 2 (preferred).
Option 1.
Add long acting beta2
ICS dose agonist (LABA)
Global Initiative for Asthma. Pocket Guide for Asthma Management and Prevention; 2017. Available from: https://www.ginasthma.org/.Cross-priming of ICS and LABA for
a synergistic effect
Barnes PJ. Pharmaceuticals 2010, 3, 514-540; doi:10.3390/ph3030514Adding LABA is better than
increasing ICS1
60
*
(mean ± standard error l/min)
50
Seretide 250/50 bd
Change in morning PEF
40 * *
30
Flixotide 250mcg bd
20 Flixotide 500mcg bd
10
0
0 1 2 3 4 5 6
*pIs it difficult to treat asthma or is it
severe asthma?GINA – Stepwise escalation of
asthma therapy
Disease severity
Step 5
Step 4 Refer for
add-on
PREFERRED Step 3 Med/hig treatment
CONTROLLER Step 1 Step 2 h
e.g.
anti-lgE
CHOICE Low dose ICS/LAB
Low dose ICS ICS/LABA A
Med/High dose High dose
Other Consider Leukotriene receptor antagonists ICS Low dose ICS+LTRA Add low
controller low dose (LTRA) ICS+LTRA (or + dose OCS
options ICS Low dose theophylline* (or + theoph*) theoph*)
As-needed SABA or low dose
RELIEVER As-needed short-acting beta2-agonist (SABA)
ICS/formoterol**
Global Initiative for Asthma. Pocket Guide for Asthma Management and Prevention; 2016. Available from: https://www.ginasthma.org/.
ICS, inhaled corticosteroid; LABA, long-acting β-agonist; LTRA, leukotriene receptor antagonists; OCS, oral corticosteroid; SABA, short-acting β2-agonistDifficult Asthma – Not Just Biology
Tay et al MJA 2018GP assessment
Adherence
Knowledge
Cost
Sustained therapy
Inhaler Technique
Spacer, ease of use, patient preference etc
Smoking cessation
Investigations
Spirometry
Serum IgE
Serum eosinophil count
What is abnormal?Who to refer?
Many definitions
Uncontrolled vs high intensity treatment to maintain control
Recognise at risk patients – who to refer?
Frequent exacerbations
2 or more courses OCS(/yr)
Severe exacerbation
Hospitalisation (ICU)
Long term OCS use
>50% previous year
Obesity + asthma
Abnormal spirometry
Diagnostic uncertainty
High B-agonist use despite reported ICS use
Prevalence – depends on definition
?400-500 patients in CDHB = 2-3/GPSpecialist Contribution
Changing landscape
Severe asthma clinics
Systematic assessment
Multidisciplinary approach
SLT
Physiotherapy
ENT
Dieticians/Bariatric surgeons
Clinical psychology
Immunologist/Allergist
Targeted therapies
Therapeutic knowledge/adherence
Address comorbidities
Increasing range of pharmacotherapy available
Two way referral pathway
For both primary and secondary careAdapted from http://ccn.health.nz/FocusAreas/ServiceLevelAlliances/Pharmacy/tabid/1347/ArticleID/1307/Funded-Inhalers-in-New-Zealand-2016.aspx (accessed 20/03/2017) ICS = inhaled corticosteroid; LABA = long acting beta2 agonist; LAMA = long acting muscarinic antagonist
Omalizumab
Mepolizumab
Mr X 59yrs
OP rv 2009
Asthma since early 20’s – on 5mg prednisone for many months
Atopy / Nasal polyps
6 yrs of worsening symptoms, more pronounced past 6/12
FEV1 – 19%! / IgE 2000+ / ANCA –ve / Eosins 1.3
No apparent salicylate intolerance (no aspirin challenge)
Significant improvement with sustained course steroids
2015
Rx 3/12 for ABPA – good response
2017
Frequent exacerbation -Further Rx ABPA
Requiring sustained low dose prednisone (5mg)
On tiotropium/montelukast
Allergist rv - silver birch immunotherapy
Eosin 0.8 / IgE 3028 / FeNO 84
2018
Jan commenced Mepolizumab
Improved lung function
ACQ5 – dropped from 15 1 ( >2 = uncontrolled asthma)Summary
We need to get excited about treating asthma…….
Still a cause of significant morbidity and mortality
Stepwise escalation of therapy based off symptom control
Identify your difficult asthmatics and get busy!
Compliance
Comorbidities
Refer if struggling to gain controlQuestions…..
Changes in asthma severity Adapted from: http://www.aafa.org/page/asthma-during-pregnancy.aspx (sourced: Aug 2018)
Asthma and Pregnancy What are the challenges? Variable disease Compliance with Rx Morbidity associated with pregnancy in people with asthma Impact on the child
Adherence
Woeful
Newcastle Study 3 cohort – 2004/2007/2013
Pregnant asthmatics on ICS 41%/29%/38%
40% non adherence
Perceived risk of drugs to foetus –major driver for reduced ICS use
Can impact on adherence through education
Antepartum - maximum increase achieved after 1 education
session around drug knowledge and inhaler technique
Post partum - sustained adherence only seen consistently in those
receiving the full 3 session education program
(Robijn et al J Asthma 2018)Effect on the child
Congenital malformations
Low birth weight – 50% increase if mother had
exacerbation during pregnancy
Prematurity
Small for gestational age (Placental insufficiency)
(Wiles et al, Obstetric Medicine 2013)
Barker hypothesis – events in pregnancy leads to chronic
disease for child later in life
Asthma pregnancy
Increased rates early childhood illness
Higher rates of bronchiolitis and subsequent childhood asthma
Titrating ICS using FeNO during pregnancy associated with
reduced rates of bronchiolitis in year 1
(Mattes J Thorax 2014)Getting pregnant Woman with asthma take longer to get pregnant Reduced IVF success Very rare to have success in woman with asthma > 35 years old
General Management Early review for pregnant woman with asthma Anticipate poor adherence and educate appropriately Treat comorbidities Gastro-oesophogeal reflux disease Sinusitis Obesity (preemptive)
Key points Asthma poses a significant issue for mum and child Exacerbation prevention is key Good management to achieve asthma control improves outcomes Education early in pregnancy is essential
Questions…..
Bronchiectasis
Clinical Assessment
Detection
Common
Chronic sputum production
Recurrent LRTI
Fatigue
Relapse post antibiotics
Haemoptysis
Chest pain
Investigation
Spirometry
CXR – very insensitive
CT ChestWhat do I do
History
Childhood events
Post menopausal
Risk factors
Level of morbidity
Investigation
Microbiology
Normal culture
AFB & culture
Immunoglobulins
ABPA Screen
IgE, serum eosinophils
Other – CF, Rh A, α-1 antitrypsinManagement of bronchiectasis
Main aim is to minimise bacterial load
Physio/Exercise
Aggressively manage upper airway pathology
Surgery for CRS
Saline rinses
Mucolytic/Anti inflammatory
Nebulised hypertonic saline
PO macrolides – azithromycin
Nebulised antibiotics
Exacerbation therapy
Antibiotics = cornerstone
Targeted when able
Minimum 2/52
Recommend continue until reach baseline symptoms then consolidate for a
further week(NB no evidence for this statement)
IV antibiotics via PICC line if patient does not settleSummary
In Summary…. Stepwise approach to treating asthma Difficult to treat asthma is not just about biology Severe asthma has a new bag of tricks Asthma poses a significant issue for mum and child with exacerbation prevention key Education early in pregnancy on the importance of asthma control is essential to help improve outcomes Main aim in bronchiectasis is to minimise bacterial load
Questions…..
Nucala® (mepolizumab 100mg) is a Prescription Medicine. Nucala is indicated as an add-on treatment for severe refractory eosinophilic asthma in patients 12 years and over. Precautions: Should not be used to treat acute asthma exacerbations. Asthma-related adverse events or exacerbations may occur during treatment. Patients should seek medical advice if asthma remains uncontrolled or worsens after initiation. Abrupt discontinuation of corticosteroids after initiations is not recommended. Acute and delayed systemic reactions, including hypersensitivity reaction (urticaria, angioedema, rash, bronchospasm, hypotension) have occurred following administration, some had a delayed onset (i.e. days). Pre-existing helminth infections should be treated prior to Nucala therapy. Opportunistic infection from herpes zoster. Pregnancy: Effect on human pregnancy is unknown. There is no data available for lactation and fertility in humans. Paediatric use: Safety and efficacy in children under 12 years of age has not been established. Interactions: No formal interaction studies have been performed with Nucala. Adverse reactions: Headache, injection site reactions, back pain, fatigue, influenza, urinary tract infection, upper abdominal pain, pruritus, eczema, muscle spasms, pharyngitis, lower respiratory tract infections, nasal congestion, dyspnoea, skin rash, fever, dizziness, nausea, vomiting, infection with herpes zoster. This is not a full list, please see full Data Sheet. Immunogenicity: Patients may develop antibodies to mepolizumab following treatment. Neutralising antibodies were detected in one subject in clinical trials. Dosage and Administration: Patients should have a blood eosinophil count of ≥150 cells/µl at initiation of treatment or ≥300 cells/µl in the prior 12 months. Adults and adolescents (12 years and older). Nucala should be reconstituted by a healthcare professional (see full Data Sheet) and administered as a subcutaneous injection (e.g. upper arm, thigh or abdomen) once every four weeks. Safety and efficacy not established in adolescents weighing less than 45kg. Not recommended in children below 12 years. Before prescribing Nucala, please review the Data Sheet at www.medsafe.govt.nz. Nucala is a registered trade mark of the GlaxoSmithKline group of companies. Marketed by GlaxoSmithKline NZ Limited, Auckland. Adverse events involving GlaxoSmithKline products should be reported to GSK Medical Information on 0800 808 500.
Flixotide® (fluticasone propionate inhaler; 50, 125 or 250mcg per actuation and Accuhaler® 50, 100 or 250mcg per actuation) is a Prescription Medicine. Flixotide is indicated for the prophylactic management of mild, moderate and severe asthma. Flixotide Inhalers and Accuhalers are fully funded medicines, normal pharmacy fees apply. Dosage: 16 years and older: 100mcg to 1000mcg twice daily. Children over 4 years: 50mcg to 200mcg twice daily. Children aged 1 to 4 years (for Flixotide Inhaler only): 100mcg twice daily administered via a paediatric spacer device with a face mask. This medicine has risks and benefits. Contraindications: Hypersensitivity to any ingredient in the preparation. Common Side Effects: Candidiasis of the mouth and throat (thrush), hoarseness, cutaneous hypersensitivity reactions. Paradoxical bronchospasm may occur. Warnings and Precautions: Not for use in acute attacks; a fast and short-acting bronchodilator is required. Avoid concomitant use with ritonavir. Care when co- administering CYP3A4 inhibitors (e.g. ketoconazole). Do not discontinue abruptly. Special care in patients with active or quiescent pulmonary tuberculosis. Before prescribing Flixotide, please review the Data Sheet at www.medsafe.govt.nz. Flixotide is a registered trade mark of the GlaxoSmithKline group of companies. Marketed by GlaxoSmithKline NZ Limited, Auckland. Adverse events involving GlaxoSmithKline products should be reported to GSK Medical Information on 0800 808 500.
Seretide® (fluticasone propionate/salmeterol xinafoate inhaler 50/25 or 125/25mcg per actuation and Accuhaler® 100/50, 250/50mcg per actuation) is a Prescription Medicine. Seretide is indicated for the treatment of children (4 years and older) and adults with reversible obstructive airway disease (ROAD) including asthma, and for the treatment of adults with chronic obstructive pulmonary disease (COPD). Seretide is a fully funded medicine. Seretide 250/25mcg inhaler is a private purchase medicine; a prescription charge will apply. Maximum Daily Dose: Metered Dose Inhaler (MDI) 2 puffs twice daily, Accuhaler 1 inhalation twice daily. Maintenance Dose: Titrate to lowest effective dose 1-2 times daily. This medicine has risks and benefits. Warnings and Precautions: Not for relief of acute symptoms. Do not discontinue abruptly. Use care when co-administering strong CYP3A4 inhibitors (e.g. ketoconazole) or in patients with pulmonary tuberculosis or thyrotoxicosis. Common Side Effects: Hoarseness/dysphonia, throat irritation, headache, oral candidiasis and palpitations. Paradoxical bronchospasm may occur. Avoid beta-blockers if possible. Before prescribing Seretide, please review the Data Sheet at www.medsafe.govt.nz. Seretide and Accuhaler are registered trade marks of the GlaxoSmithKline group of companies. Marketed by GlaxoSmithKline NZ Limited, Auckland. Adverse events involving GlaxoSmithKline products should be reported to GSK Medical Information on 0800 808 500. TAPS DA1852JS/18AU/AST/0003/18
You can also read