Studies of Offspring of Parents With Bipolar Disorder
←
→
Page content transcription
If your browser does not render page correctly, please read the page content below
American Journal of Medical Genetics Part C (Semin. Med. Genet.) 123C:26 – 35 (2003)
A R T I C L E
Studies of Offspring of Parents With
Bipolar Disorder
KIKI CHANG,* HANS STEINER, AND TERENCE KETTER
Children and adolescents who are the biological offspring of individuals with bipolar disorder (BD) (bipolar
offspring) represent a population rich in potential for revealing important aspects in the development of BD.
Multiple cross-sectional assessments of psychopathology in bipolar offspring have confirmed high incidences of
BD, as well as mood and behavioral disorders, and other psychopathology in this population. Longitudinal studies
of offspring have begun to shed light on precursors of BD development. Other assessments of bipolar offspring
have included dimensional reports of psychiatric and psychosocial functioning, temperament assessments, and
descriptions of family environments and parenting styles. Neurobiological studies in bipolar offspring are just
beginning to yield findings that may be related to the underlying neuropathophysiology of BD. The future holds
promise for longitudinal studies of bipolar offspring incorporating all of these facets, including genetic analyses,
to further elucidate the factors involved in the evolution of BD. ß 2003 Wiley-Liss, Inc.
KEY WORDS: bipolar disorder; bipolar offspring; attention deficit hyperactivity disorder
INTRODUCTION vs. state determinations of any biological and other characterization of bipolar
findings. offspring, report on the few neurobio-
Children and adolescents who are the
The ultimate reason for studying logical studies in bipolar offspring, and
biological offspring of individuals with
bipolar offspring may be for early inter- propose future directions for research in
bipolar disorder (BD) (hereafter referred
vention and prevention purposes. The this area.
to as bipolar offspring) represent a
concept of kindling in affective disor-
population rich in potential for revealing
ders, as proposed by Post [1992], argues
important aspects in the development of RETROSPECTIVE DATA OF
for the need for such early identification
BD. Bipolar offspring are at relatively EARLY-ONSET SYMPTOMS
of individuals at high risk for developing
high genetic risk for development of BD, OF BD
BD. The kindling theory suggests that
as well as other psychopathology. There-
mood disorders are created by an inter- Retrospective reports of childhood dis-
fore, a greater understanding of familial
play between a susceptible genetic dia- orders in adults with BD provide insight
transmission of BD can be gained
thesis and environmental stressors that into possible early expressions of BD. In a
through studying bipolar offspring.
causes biological changes at the genetic questionnaire-based study, support
Furthermore, through having a parent
level, which over time lead to the cros- group members with BD reported
with BD who may have had significant
sing of a neurobiological threshold for a symptoms of depressed mood, hyper-
mood episodes that impacted the child,
mood episode. With the onset of each activity, suicidality, and manic behavior
environment–gene interactions can be
successive episode of mania or depres- occurring before their first manic epi-
evaluated. Their status as at risk for de-
sion, these biological changes accrue, sode. Thirty-one percent of respondents
veloping BD also allows for study of trait
leading to more frequent and sponta- described experiencing these symptoms
neous episodes. If applicable to BD, in before the age of 15 years and 17% before
order to lessen future morbidity, it is the age of 10 years [Lish et al., 1994].
important to intervene at as early a stage Similarly, in a study of adults hospitalized
as possible in bipolar development. in New York for their first psychotic
Dr. Kiki Chang is Assistant Professor and
Director, Pediatric Mood Disorders Clinic. Therefore, studies of populations at high episode, 67% of those with BD reported
Dr. Hans Steiner is Professor, Director of risk for developing BD are necessary to childhood-onset psychiatric distur-
Residency Training. inform researchers and clinicians as to bance, with 21% having disruptive
Dr. Terence Ketter is Associate Professor,
Chief of the Bipolar Disorders Clinic.
the most appropriate individuals in behavioral disorders [Carlson et al.,
*Correspondence to: Dr. Kiki Chang, which to institute early intervention. 2000].
Division of Child and Adolescent Psychiatry, This review will summarize the evi- These retrospective data point to
Stanford University School of Medicine, 401
Quarry Road, Stanford, CA 94305. dence establishing bipolar offspring as a possible early stages in BD development.
E-mail: kchang88@stanford.edu high-risk group, discuss the extant Collection of prospective data would
DOI 10.1002/ajmg.c.20011 studies of psychiatric phenomenology provide more reliable data, but in order
ß 2003 Wiley-Liss, Inc.ARTICLE AMERICAN JOURNAL OF MEDICAL GENETICS (SEMIN. MED. GENET.) 27
to collect relevant data, a sample at high 772 children with a bipolar parent and bipolar I or II disorder. Soutullo [2000]
risk for BD development would need to 626 children of healthy parents included reported that 50% of 24 bipolar offspring
be studied. in the meta-analysis. Over half (52%) had a bipolar spectrum disorder, com-
of the bipolar offspring met Diagnostic pared to 9% of 13 healthy controls. It is
and Statistical Manual (DSM)-III or unclear whether this increase in BD in-
PHENOMENOLOGICAL DSM-III-R criteria for a psychiatric cidence in bipolar offspring is due simply
STUDIES OF BIPOLAR disorder, compared to 29% of the to the widening of the bipolar spectrum
OFFSPRING children of healthy parents. Relative in DSM-IV or to other factors, such as
risk analysis revealed bipolar offspring more accurate diagnoses through struc-
The heritability of BD may be 40–70%,
to be more than 2.5 times as likely tured interviews geared toward child-
based on both studies of relatives of
to develop a psychiatric disorder hood affective disorders [for discussion,
bipolar probands and twin concordance
see DelBello and Geller, 2001]. It is also
studies [for review, see Craddock and
possible that familial BD incidence is
Jones, 1999]. Therefore, offspring of
growing due to genetic or environmen-
parents with BD should be at high risk Over half (52%) of the bipolar
tal influences.
themselves for BD development. Formal offspring met Diagnostic A study from the Netherlands of a
studies of children with manic-depres-
and Statistical Manual Dutch cohort gives a perspective differ-
sive parents were not conducted until the
ent from the North American studies
1970s. Kestenbaum [1979] reported that (DSM)-III or DSM-III-R discussed above [Wals et al., 2001]. In
13 children with a bipolar parent had a
preponderance of temper tantrums, dy- criteria for a psychiatric this study, only 3% of 140 bipolar of-
fspring had a lifetime diagnosis of BD.
sphoric symptoms, obsessive and com- disorder, compared The authors proposed that the relatively
pulsive tendencies, hyperactivity, mood
to 29% of the children of low incidence might be due to less pre-
lability, and impulsivity. McKnew et al.
healthy parents. scribing of potentially mania-inducing
[1997] found over half of 30 children of
antidepressants or stimulants to children
inpatients with affective disorder (uni-
in Europe compared to the United
polar or bipolar) to have depressive
States.
disorders themselves.
and 4.0 times more likely to develop an Externalizing and behavioral disor-
affective disorder than the control group. ders also have been increasingly recog-
Furthermore, 5.4% of bipolar offspring nized in bipolar offspring. Attention
The heritability of BD may were diagnosed with BD, compared to deficit hyperactivity disorder (ADHD)
be 40–70%, based on both 0% of the control group [Lapalme et al., was first reported in bipolar offspring in
1997]. As all of these studies except three 1983 [Decina et al., 1983]. Since 1988,
studies of relatives of bipolar were cross-sectional, the number of of- ADHD or significant behavioral or
probands and twin fspring developing BD may eventually attention problems have been reported
be higher, given that many of the bipolar in approximately 27% of bipolar off-
concordance studies. offspring would not yet have been at spring studied (Table I).
the most common age of onset of BD, ADHD in children with strong
between 15 and 19 years [Goodwin and family histories of BD may be the first
Phenomenological bipolar off- Jamison, 1990]. sign of a developing BD. Family studies
spring studies published between 1983 Studies conducted after this meta-
and 1993 [Kuyler et al., 1980; Waters and analysis have reported about a 50% in-
Marchenko-Bouer, 1980; LaRoche cidence of some psychiatric disorder in
et al., 1981, 1985, 1987; Decina et al., cross-sectional assessments of child and ADHD in children with
1983; Gershon et al., 1985; Kashani adolescent bipolar offspring [Duffy et al., strong family histories of BD
et al., 1985; Klein et al., 1985; Hammen 1998; Chang et al., 2000; Soutullo,
et al., 1987, 1990; Weintraub, 1987; 2000]. BD itself has been increasingly
may be the first sign of a
Zahn-Waxler et al., 1988; Nurnberger diagnosed in bipolar offspring, perhaps developing BD. Family
et al., 1988b; Grigoroiu-Serbanescu in part due to the inclusion of BD not studies of probands with
et al., 1989; Radke-Yarrow et al., 1992; otherwise specified (NOS) and bipolar
Carlson and Weintraub, 1993] were II disorder in DSM III-R and DSM-IV ADHD and BD have
analyzed in a meta-analysis [Lapalme [American Psychiatric Association, supported this comorbidity
et al., 1997] (Table I). Of these 17 1994]. Duffy et al. [1998] found five of
studies, 11 also included a comparison 36 bipolar offspring to have bipolar as representing a familial
group of offspring of parents with spectrum disorders, and Chang et al. type of early-onset BD.
no major mental disorder. There were [2000] found nine of 60 offspring to have28 AMERICAN JOURNAL OF MEDICAL GENETICS (SEMIN. MED. GENET.) ARTICLE
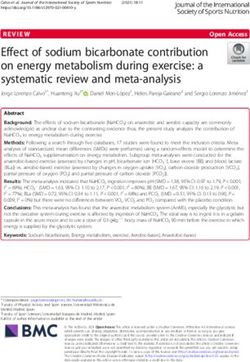
TABLE I. Phenomenological Studies of Bipolar Offspring*
N % with % with
First author (Year) (Families) BD % with ADHD any Dx Ratinga Comments
McKnew [1979] 30 (13) 16 ** Depression was only diagnosis found
Kuyler et al. [1980] 49 (27) 0 0 22 (45%) **
Laroche et al. [1981] 17 (10) 0 0 0 (0%) **
Cytryn [1982] 19 (13) 11/13 ***** Same cohort as McKnew [1979],
families but with blinded raters and
control group
Decina et al. [1983] 31 (18) 0 (5) 2 (6%) 16 (52%) ****1/2 Children interviewed with the
Mental Health Assessment form
Gershon et al. [1985] 29 1 (3%) 4 (14%) 21 (72%) **** control group 8 children had atypical depression,
included, but which included cyclothymic
unclear if blinded disorder
interviewers
Kashani et al. [1985] 9 (5) 0 1 (11%) ? ***1/2 Parent not Bipolar offspring not significantly
assessed directly different from unipolar offspring
Klein et al. [1985] 37 (24) 10 (27%) 16 (43%) **** Subjects 15–21 years old. Parents
not interviewed about children
LaRoche et al. 39 0 0 9 (23%) **1/2 13% with cyclothymic personality
[1985] traits
Weintraub [1987] 134 (58) 27 (20%) *** Subjects assessed at age >18 years
Nurnberger et al. 53 (32) ? ? 38 (72%) **** Subjects 15–25 years old
[1988a]
Zahn-Waxler [1988] 7 (7) 0 2 (29%) 6 (86%) **** Children assessed at age 6 years
Grigoroiu-Serba- 72 (47) 1 (1%) 15 (21%) 44 (61%) ****1/2 Parents interviewed clinically.
nescu et al. [1989] Controls with 25%
psychopathology
Hammen [1990] 18 (14) 0 1 (6) 13 (72%) ***** All mothers with BD. 82% of
unipolar comparison group with
psychopathology
Radke-Yarrow 44 (22) (56%) ****1/2 Results from subjects 8–11 years old
[1992] reported here
Carlson and 128 6/125 (5%) 39 (30%) ? ***** Longitudinal follow-up at over age
Weintraub [1993] (at baseline) 18 years
Duffy et al. [1998] 36 (23) 5 (14%) 1 (3%) 19 (53%) *** Subjects 10–25 years old
Soutullo [1999] 24 12 (50%) 16 (67%) ? ***** High rate of BP and ADHD in
controls (9%, 18%)
Chang et al. [2000] 60 (37) 8 (13%) 16 (27%) 31 (52%) **** Parents with retrospective ADHD
more likely to have offspring with
BD
Wals et al. [2001] 140 (86) 4 (3%) 7 (5%) 61 (44%) **** Netherlands, age 12–21, 27% had a
mood disorder
*Reproduced with permission from Chang and Steiner [2003].
a
Ratings guidelines
**Offspring interviewed with semi-structured interviews (children directly interviewed).
***Offspring interviewed with semi-structured interviews, parents interviewed about children.
****Parents and offspring interviewed with semi-structured interviews, parents interviewed about children, children directly interviewed.
*****Parents and offspring interviewed with semi-structured interviews, parents interviewed about children, children directly
interviewed, interviewers blinded to parental status, control group assessed.
BP, bipolar spectrum disorders (bipolar I, II, or NOS, or cyclothymia); ADHD, attention-deficit/hyperactivity disorder; Dx, diagnosis; ?,
not reported. Blank cells indicate uncertainty whether interview used allowed for possibility of such a diagnosis.ARTICLE AMERICAN JOURNAL OF MEDICAL GENETICS (SEMIN. MED. GENET.) 29
of probands with ADHD and BD vioral disorders such as oppositional OTHER
have supported this comorbidity as defiant disorder and conduct disorder CHARACTERIZATIONS
representing a familial type of early- have high comorbidity with BD (up to OF BIPOLAR OFFSPRING
onset BD [Faraone et al., 1997a,b]. 71% and 54%, respectively) [Kovacs
Furthermore, Chang et al. [2000] found and Pollock, 1995; Geller et al., 2000] CBCL
that seven of eight offspring with BD had and are present in bipolar offspring
Besides making categorical diagnoses,
first met criteria for ADHD. Also in this [Chang et al., 2000]. It is possible that
another way of characterizing bipolar
study, parents with BD who retrospec- the presence of any early psychopathol-
offspring is by a dimensional approach,
tively reported a history of ADHD ogy in bipolar offspring could result
which does not rely only on DSM-IV
during their own childhood were more in increased experienced stress, thus
criteria and clusters disturbances in
likely to have children already with BD increasing the likelihood of BD devel-
several independent and interrelated
than bipolar parents without a history of opment in an individual already at
domains. One frequently used example
ADHD. Thus, it is possible that this genetic risk.
of the dimensional approach is the Child
increase in the prevalence of ADHD in It should be noted that the afore-
Behavior Checklist (CBCL) [Achen-
bipolar offspring may actually reflect an mentioned studies of bipolar offspring
bach and Edelbrock, 1983; Achenbach,
overall increase in early forms of evol- usually did not take into account the
1991], a standardized format for report-
ving BD. presence of comorbid disorders in the
ing the behavioral problems and com-
One longitudinal study that sup- bipolar parent or psychiatric disorders in
petencies of children ages 4–18 as
ports this link between behavioral dis- the spouse. That is, these cohorts may
reported by their parents or guardians
orders and BD in children at risk for BD have been contaminated by the pre-
[Bird et al., 1987]. Three studies have
followed 134 bipolar offspring and 108 sence of multiple psychiatric conditions
used the CBCL to differentiate between
healthy controls from childhood to early on either parent’s side. For example,
BD and ADHD in children [Biederman
adulthood. At baseline, 27.6% of bipolar the presence of unipolar depression in
et al., 1995; Geller et al., 1998; Hazell
offspring had behavioral problems, and these genealogies may account for some
et al., 1999]. Wals et al. [2001] reported
30.4% had attention problems, as de- amount of mood disorder development
on CBCL scores in a population of
fined by various rating scales. Upon and psychosocial morbidity of the off-
bipolar offspring, finding that girls
reassessment after age 18 years, beha- spring. A few studies of bipolar off-
scored higher on eight of the 11 clinical
vioral or attention problems in child- spring included a comparison group of
scales and boys scored higher on four
hood were found to be associated with children with a parent with unipolar
of the 11 clinical scales than a group
development of a mood disorder in major depressive disorder. While two of
of healthy controls. However, CBCL
young adulthood only in the bipolar these studies reported no differences
scores were not stratified by different
offspring. This was the first study to in amount of psychopathology in uni-
diagnostic groups within the offspring
make such a link between behavioral polar compared to bipolar offspring
group.
disorders and later development of mood [Kashani et al., 1985; Weintraub,
disorders in a population at high risk 1987], two others reported that children
for BD. with unipolar parents had higher rates
While ADHD has been established of psychopathology. Therefore, the These studies, conducted in
as a precursor for early-onset BD, other presence in bipolar offspring lineages
bipolar offspring from infancy to
diagnoses that have a high comorbidity of disorders other than BD may ac-
with pediatric BD, including anxiety count for some of the findings discussed adolescence, indicate a
disorders, may precede full BD devel- here. tendency of bipolar offspring
opment. In one outpatient sample, only Data from these phenomenological
23.5% of children and adolescents with studies support bipolar offspring as a to possess temperaments that
bipolar I or II disorder did not have a cohort at high risk for development may result in less than
comorbid anxiety disorder [Masi et al., of numerous psychiatric disorders, spe-
2001]. Several bipolar offspring studies cifically ADHD, depression, and BD.
optimal reactions to
reported the presence of anxiety dis- However, it may be difficult to disen- psychosocial stressors and
orders, predominantly separation anxi- tangle the effects of genetics from the predispose them to
ety and generalized anxiety, in offspring effects of parenting and other environ-
who did not yet meet the criteria for BD mental factors in the etiology of development of affective
[Cytryn et al., 1982; Decina, 1983; this increased risk. Furthermore, addi- psychopathology.
Hammen, 1987, 1990; Radke-Yarrow, tional longitudinal studies are needed
1992; Chang, 2000]. Thus, early symp- to delineate the significance of these
toms of anxiety in some offspring may disorders in bipolar offspring as they In an offspring cohort with a higher
represent another pathway toward later relate to future psychopathology and incidence of psychopathology than that
BD development. Similarly, other beha- functioning. of Wals et al. [2001], Dienes et al.30 AMERICAN JOURNAL OF MEDICAL GENETICS (SEMIN. MED. GENET.) ARTICLE
[2002] found that bipolar offspring had pared to depressed or healthy mothers,
elevated scores on every clinical scale of However, specific mothers with BD were found to be more
the CBCL. Bipolar offspring with BD negative in their interactions with their
psychopathology in the
were more pervasively disturbed than children [Inoff-Germain et al., 1992]. In
the offspring with other disorders. How- bipolar offspring could not be a study of 39 bipolar offspring, presence
ever, compared to the ADHD group, predicted based on a particular of offspring psychopathology was cor-
the BD group scored higher only on related with levels of marital discord and
the Withdrawn, Anxious/Depressed, family environment profile. exposure of offspring to parental illness
and Aggressive Behavior subscales of before age 3 years [LaRoche et al., 1985].
the CBCL. In a past study of a clinical In a study using the Family Environ-
cohort not selected for offspring suffering of others.’’ These children mental Scale, families with a bipolar
status, children with ADHD had lower also had problems socializing appropri- parent were found to have less cohesion
scores than children with mania on the ately with peers, less inclination to share, and organization and more conflict than
Delinquent Behavior, Aggressive Beha- and more aggression toward both peers families from a national, unscreened
vior, Withdrawn, Somatic Complaints, and adults. Similarly, Gaensbauer et al. sample. However, specific psychopatho-
Anxious/Depressed, and Thought Pro- [1984] studied seven male bipolar off- logy in the bipolar offspring could not be
blems subscales [Biederman et al., 1995]. spring infants (12–18 months old) and predicted based on a particular family
It is possible that Dienes et al. [2002] may noted that compared to infants of environment profile. Other investigators
have detected a group of offspring with nondisordered parents, the bipolar off- have suggested correlations between
ADHD with early symptoms of BD, spring showed more negative effects and pathological family environments and
leading to a greater similarity between less ability to self-soothe when upset. severity of illness in bipolar offspring
offspring with BD and those with only These studies, conducted in bipolar [Kuyler et al., 1980; Grigoroiu-Serba-
ADHD than found in previous studies of offspring from infancy to adolescence, nescu et al., 1989]. These findings are
nonbipolar offspring. indicate a tendency of bipolar offspring interesting and suggest that detailed
to possess temperaments that may result studies of shared and nonshared envir-
in less than optimal reactions to psycho- onmental characteristics should shed
Temperament
social stressors and predispose them to further light on the relative contribu-
Temperament characterizations of bipo- development of affective psychopathol- tions to BD development in bipolar of-
lar offspring strive to assess inborn ogy. Further studies of temperament in fspring. An interesting candidate would
patterns of behavior and mood present bipolar offspring, preferably in labora- be the expressed emotion construct,
since an early age, which may be gene- tory situations and at very young ages, which has been shown to contribute to
tically determined and avoid some con- are necessary to clarify the importance of relapse in studies of other psychoses
tamination from environmental factors. inborn traits to this area of study. [Vaughn and Leff, 1976] and more
However, it is often difficult to discern recently in bipolar adults [Miklowitz
temperament in the context of long- et al., 1988]. Therefore, parental and
Family Environment
standing psychopathology. Neverthe- extended familial interactions with
less, laboratory measures or parental The characterization of the immediate bipolar offspring may have a critical role
report of temperament at very young social environments of bipolar children in development of BD as well.
ages could offer valuable insights. Chang and offspring has received some atten-
et al. [2003b] compared parental reports tion. The impact of parental psycho-
Psychosocial Functioning
of temperament in bipolar offspring to pathology in general on their children
national means on the Dimensions of has been long established as significant. Regardless of specific psychopatho-
Temperament Survey-Revised (DOTS- Bipolar offspring often demonstrate logy, bipolar offspring may represent
R). Offspring with already syndromal disordered functioning in domains that a population at risk for poor psychoso-
BD had higher levels of general activity, have been shown to be strongly influ- cial functioning. In one controlled
less ability to stay on task, and lower enced by deficient parenting, such as study, bipolar offspring were found to
flexibility or adaptability. This charac- aggressive behavior [Patterson et al., have a relatively weak social support
terization resembles the temperament 1989]. Furthermore, the question of group with an absence of a best friend
construct of behavioral disinhibition, the precise importance of environmental [Pellegrini et al., 1986]. One of the few
which has been linked to the develop- stressors in the precipitation of the prospective longitudinal studies of bipo-
ment of disruptive behavioral disorders disorder itself [Post, 1992] makes this a lar offspring is being conducted at the
[Hirshfeld-Becker et al., 2002]. relevant area of study. National Institute of Mental Health
Zahn-Waxler et al. [1984] noted Several studies are examining the (NIMH) by Radke-Yarrow and collea-
that 2-year-old children of bipolar pa- impact of parent-child interaction and gues, comparing offspring of mothers
rents showed ‘‘heightened distress and the structural characteristics of the family with BD to offspring of depressed or
preoccupation with the conflicts and environment of bipolar offspring. Com- healthy mothers. At older ages, but notARTICLE AMERICAN JOURNAL OF MEDICAL GENETICS (SEMIN. MED. GENET.) 31
have not yet been investigated in this ing marked melatonin suppression.
Regardless of specific group as a whole. There may be a correlation between
the degree of melatonin suppression and
psychopathology, bipolar
genetic loading for BD [Nurnberger
offspring may represent a Psychological and
et al., 1988b], as 91% of a sample of
Biological Markers
population at risk for poor adults with BD also were reported to
Presence of identifiable biological traits have marked melatonin suppression
psychosocial functioning. In in bipolar offspring could lead to early [Lewy et al., 1985]. However, further
one controlled study, bipolar identification of those at highest risk for studies investigating melatonin reactivity
BD development and to a better under- in bipolar offspring have not since been
offspring were found to have a standing of the pathophysiology of BD conducted.
relatively weak social support development. Therefore, some effort The development of relatively safe
group with an absence of a has been made to identify such biological and noninvasive magnetic resonance
markers. IQ testing of bipolar offspring, imaging (MRI) technologies has led to
best friend. an indirect indicator of neurobiology, increased neuroimaging studies of chil-
has had mixed results, including findings dren, including studies of bipolar off-
of decreased [McDonough-Ryan et al., spring. DelBello et al. [2000] reported
younger ages, bipolar offspring reported 2000], normal [Waters et al., 1981], and increased hippocampal size in bipolar
suicidal ideation more often than chil- increased IQ scores [as reported by offspring who did not meet criteria for
dren of healthy mothers. Presence of Kestenbaum, 1980; Decina et al., BD, but who ranged from symptom-free
hypomanic symptoms or a mother with 1983]. Furthermore, one study reported to mood disordered. Using magnetic
past suicide attempts correlated with some increased incidence of a verbal– resonance spectroscopy (MRS), Chang
suicidal ideation in adolescent offspring performance IQ split in bipolar off- et al. [2003a] reported decreased N-
of bipolar mothers [Klimes-Dougan spring, with verbal scores higher than acetylaspartate (NAA)/creatine ratios
et al., 1999]. Notably, in the same cohort performance scores [McDonough- in right dorsolateral prefrontal cortex
at 3-year follow-up, significantly more Ryan et al., 2002]. However, in this of bipolar offspring with BD. It remains
offspring of affectively-ill parents had study other signs of nonverbal learning
developed depressive and behavioral disorders, including worse mathematics
problems. performance, were not found. Eye- DelBello et al. reported
Another study measured externa- tracking abnormalities have been
lizing and internalizing behaviors, reported in offspring of parents with increased hippocampal
school performance, and behavior in schizophrenia [Erlenmeyer-Kimling, size in bipolar offspring
class, finding offspring of depressed 2000], but no such abnormalities have
mothers to have worse overall psycho- been found in bipolar offspring [Rosen- who did not meet criteria
social functioning than offspring of berg et al., 1997]. A study of electro- for BD, but who ranged from
bipolar, medically ill, or healthy mothers dermal activity in bipolar offspring
symptom-free to mood
[Anderson and Hammen, 1993]. In a compared to healthy controls did not
previously mentioned study, a cohort of find any differences at rest [Zahn et al., disordered. Using magnetic
60 bipolar offspring had a mean Global 1989]. However, when performing a resonance spectroscopy,
Assessment of Functioning (GAF) of mental arithmetic task, bipolar offspring
76 12, indicating fairly good function- showed higher electrodermal activity, Chang et al. reported decreased
ing. Scores on the Wide Range correlating with a higher self-report of N-acetylaspartate (NAA)/
Achievement Test, Third Edition anxiety [Zahn et al., 1991]. Another
(WRAT-3) an indicator of academic study examined melatonin suppression
creatine ratios in right
achievement, were also all at or above by light of 25 bipolar offspring 15–25 dorsolateral prefrontal
grade level. However, bipolar offspring years old and 20 healthy controls cortex of bipolar offspring
with psychopathology compared to [Nurnberger et al., 1988b]. Bipolar
those without psychopathology had offspring showed significantly higher with BD.
lower GAF scores but did not have suppression of melatonin levels after
differing levels of academic achievement bright light exposure than controls.
[Chang and Steiner, 2003]. Furthermore, the group of seven off- to be seen whether offspring without
Bipolar offspring, particularly those spring with two bipolar parents had the BD, or with other psychopathology, have
who develop psychopathology, appear at highest percentage of subjects (57%) similarly decreased prefrontal NAA.
risk for poor psychosocial and academic with marked melatonin suppression, Neuroimaging studies in adults and
functioning. However, psychosocial with only 21% of controls and 33% of children with BD have revealed findings
interventions, including psychotherapy, offspring with one bipolar parent show- that could guide future study in bipolar32 AMERICAN JOURNAL OF MEDICAL GENETICS (SEMIN. MED. GENET.) ARTICLE
offspring. Volumetric MRI studies over- cyclothymia or BD NOS [Findling familial incidence, twin, and adoption
all suggest that patients with BD may et al., 2000]. This study of 60 bipolar studies [for review, see Craddock and
have prefrontal, temporal, cerebellar, offspring has recently been completed Jones, 1999]. However, linkage studies
ventricular, and deeper structural (stria- and data analysis is pending. have implicated different chromosomal
tum and amygdala) volume changes, as These two studies represent the regions and association studies have been
well as white matter abnormalities as possibility of early intervention in chil- equivocal. The heterogeneity of BD may
indicated by white matter hyperinten- dren at high risk for BD. However, be partially responsible for this difficulty
sities [for reference, see Strakowski et al., nonpharmacologic intervention strate- in isolating consistent gene regions
2000, 2002]. Results from positron gies could also prove useful. For exam- associated with BD and replicating
emission tomography (PET) studies of ple, group cognitive therapy was more positive findings. Therefore, genetic
bipolar patients have been varied; per- effective than no specific intervention in factors that contribute to BD develop-
haps the most consistent findings have reducing depressive symptoms of ado- ment may be better identified through
been decreased blood flow in the pre- lescent offspring of depressed parents more homogenous cohorts within the
frontal cortex during bipolar depressed [Clarke et al., 2001]. Similarly, psychoe- bipolar spectrum. Bipolar offspring who
states and a general implication of the ducation sessions for families with a already exhibit early or fully developed
prefrontal cortex (DLPFC, ACC, and depressed parent may be effective in BD would represent such a cohort.
orbitofrontal cortex), limbic structures reducing problematic behaviors of the However, most genetic studies have
(amygdala, insula), striatum, and thala- children in the household [Beardslee targeted bipolar adult probands and their
mus in the neuropathophysiology of BD and Gladstone, 2001]. These novel ap- families; there are currently no published
[Blumberg et al., 2002]. Studies of adults proaches to prevention of depression genetic studies that have concentrated
with familial BD have reported abnorm- could be similarly applied to bipolar on affected bipolar offspring in this
alities in the subgenual prefrontal cortex offspring. manner.
[Drevets et al., 1997; Ongur et al., 1998], It remains to be definitively seen Genetic anticipation has also been
cerebellum (particularly the cerebellar whether these intervention strategies reported in BD cohorts. Anticipation
vermis), and lateral ventricles [Brambilla can treat bipolar offspring more effec- refers to the phenomenon of a disease
et al., 2001]. These brain regions may tively than conventional treatment stra- state occurring in successive generations
have structural or functional alterations tegies, or whether BD development can with earlier ages of onset and/or higher
in familial BD and therefore could be be halted by these interventions. Further severity. In other neurological disorders
reasonably investigated in bipolar off- with anticipation, trinucleotide repeat
spring. Additional volumetric, spectro- sequences have been found to expand in
scopic, and functional MRI studies of It remains to be definitively number of repeats with each generation
bipolar offspring would aid in further [for review, see Goossens et al., 2001].
identifying neurobiological char- seen whether these intervention An increase in mean CAG repeat length
acteristics that could represent strategies can treat bipolar was associated with a diagnosis of BD
vulnerability traits or early stages of [Lindblad et al., 1995; O’Donovan et al.,
BD development. Currently, however,
offspring more effectively 1996] and with anticipation of BD in a
there are no reliable biological markers than conventional treatment few studies of families with BD [Men-
correlated with risk for development strategies, or whether BD dlewicz et al., 1997; Lindblad et al.,
of BD. 1998]. However, there have been no
development can be halted by replications of these studies and several
these interventions. negative reports [Craddock et al., 1997;
EARLY INTERVENTION
Li et al., 1998; Zander et al., 1998;
STUDIES
Meira-Lima et al., 2001]. Furthermore,
Researchers have begun to investigate these repeat sequences have not been
studies, perhaps better informed by
pharmacologic interventions in bipolar successfully linked to meaningful gene
using yet to be discovered biological
offspring who have subsyndromal and regions. Families with reported antici-
markers, and incorporating placebo
therefore possibly prodromal forms of pation from affected parent to affected
arms and longitudinal assessments, will
BD. Seventy-eight percent of a cohort of offspring are a natural choice for inves-
help to identify the appropriate treat-
23 bipolar offspring with mood or tigation for the presence of such repeat
ments for individuals at high risk for BD
behavioral disorders and at least mild sequences. Prospective studies in off-
development.
affective symptoms were reported to spring cohorts that combine genetic
improve clinically after a 12-week open analyses with phenomenological assess-
trial of divalproex [Chang et al., 2003c]. ment would help decrease ascertainment
GENETICS
In a placebo-controlled study, research- and recall biases and possibly clarify
ers are investigating the efficacy of The genetic basis of BD has been well the genetic influences on anticipation
divalproex in bipolar offspring with established through pedigree analysis, in BD.ARTICLE AMERICAN JOURNAL OF MEDICAL GENETICS (SEMIN. MED. GENET.) 33
CONCLUSIONS future prospects. Biol Psychiatry 49:1101– American Academy of Child Psychiatry
1110. 21:389–391.
Bipolar offspring have been well estab- Biederman J, Wozniak J, Kiely K, Ablon S, Decina P, Kestenbaum CJ, Farber S, Kron L,
lished as at high risk for the development Faraone S, Mick E, Mundy E, Kraus I. 1995. Gargan M, Sackeim HA, Fieve RR. 1983.
CBCL clinical scales discriminate prepuber- Clinical and psychological assessment of
of BD and other mood disorders. It tal children with structured interview- children of bipolar probands. Am J Psychia-
appears likely that family environment derived diagnosis of mania from those with try 140:548–553.
and psychosocial stressors interact with ADHD. J Am Acad Child Adolesc Psychia- DelBello MP, Geller B. 2001. Review of studies of
try 34:464–471. child and adolescent offspring of bipolar
genetic predisposition for affective ill- Bird HR, Canino G, Gould MS, Ribera J, Rubio- parents. Bipolar Disord 3:325–334.
ness to create such disorders in bipolar Stipec M, Woodbury M, Huertas-Goldman DelBello MA, Soutullo CA, Ryan P, Graman SM,
offspring. Temperament characteristics S, Sesman M. 1987. Use of the Child Zimmerman ME, Getz GE, Lake K,
Behavior Checklist as a screening instru- Strakowski SM. 2000. MRI analysis of
of high motor activity, low frustration ment for epidemiological research in child children at risk for bipolar disorder. Biol
tolerance, and emotional sensitivity may psychiatry: results of a pilot study. J Am Acad Psychiatry 47:43.
reflect inborn characteristics in bipolar Child Adolesc Psychiatry 26:207–213. Dienes KA, Chang KD, Blasey CM, Adleman
Blumberg HP, Charney DS, Krystal JH. 2002. NE, Steiner H. 2002. Characterization of
offspring that may predispose them to Frontotemporal neural systems in bipolar children of bipolar parents by parent report
BD development. Behavioral disorders disorder. Semin Clin Neuropsychiatry CBCL. J Psychiatr Res 36:337–345.
in this population such as ADHD 7:243–254. Drevets WC, Price JL, Simpson JR Jr, Todd RD,
Brambilla P, Harenski K, Nicoletti M, Mallinger Reich T, Vannier M, Raichle ME. 1997.
may also be early indicators of later AG, Frank E, Kupfer DJ, Keshavan MS, Subgenual prefrontal cortex abnormalities in
development of mood disorders. Deli- Soares JC. 2001. MRI study of posterior mood disorders. Nature 386:824–887.
neation of the nature of interaction be- fossa structures and brain ventricles in Duffy A, Alda M, Kutcher S, Fusee C, Grof P.
bipolar patients. J Psychiatr Res 35:313– 1998. Psychiatric symptoms and syndromes
tween environment and genetics needs 322. among adolescent children of parents with
to be accomplished. Future neurobiolo- Carlson GA, Weintraub S. 1993. Childhood lithium-responsive or lithium-nonrespon-
gical data, from neuroimaging, neuro- behavior problems and bipolar disorder– sive bipolar disorder. Am J Psychiatry
relationship or coincidence? J Affect Disord 155:431–433.
endocrine, or similar studies of bipolar 28:143–153. Erlenmeyer-Kimling L. 2000. Neurobehavioral
offspring, will help identify markers that Carlson GA, Bromet EJ, Sievers S. 2000. deficits in offspring of schizophrenic parents:
may signal higher risk for or describe Phenomenology and outcome of subjects liability indicators and predictors of illness.
with early- and adult-onset psychotic mania. Am J Med Genet 97:65–71.
etiological factors of BD development. Am J Psychiatry 157:213–219. Faraone SV, Biederman J, Mennin D, Wozniak J,
Such studies of bipolar offspring should Chang KD, Steiner H. 2003. Offspring studies in Spencer T. 1997a. Attention-deficit hyper-
ideally be longitudinal, in order to fully child and early adolescent bipolar disorder. activity disorder with bipolar disorder: a
In: Geller B, DelBello M, editors. Bipolar familial subtype? J Am Acad Child Adolesc
capture the process of bipolar develop- disorder in childhood and early adolescence. Psychiatry 36:1378–1387; discussion,
ment in at-risk individuals. Finally, New York: The Guilford Press. p 107–129. 1387–1390.
studies combining these biological find- Chang KD, Steiner H, Ketter TA. 2000. Psychia- Faraone SV, Biederman J, Wozniak J, Mundy E,
tric phenomenology of child and adolescent Mennin D, O’Donnell D. 1997b. Is comor-
ings with genetic data acquired from bipolar offspring. J Am Acad Child Adolesc bidity with ADHD a marker for juvenile-
bipolar offspring with full or prodromal Psychiatry 39:453–460. onset mania? J Am Acad Child Adolesc
BD are needed. The application of Chang K, Adleman N, Dienes K, Barnea-Goraly Psychiatry 36:1046–1055.
N, Reiss A, Ketter T. 2003. Decreased N- Findling RL, Gracious BL, McNamara NK,
modern techniques of DNA analysis acetylaspartate in children with familial Calabrese JR. 2000. The rationale, design,
and neuroimaging to populations at high bipolar disorder. Biol Psychiatry 53:1059– and progress of two novel maintenance
risk for BD development may help to 1065. treatment studies in pediatric bipolarity.
Chang KD, Blasey C, Ketter TA, Steiner H. Acta Neuropsychiatrica 12:136–138.
eventually reveal the genetic and neuro- 2003b. Temperament characteristics of Gaensbauer TJ, Harmon RJ, Cytryn L, McKnew
biological underpinnings of BD. bipolar offspring. J Affect Disord (in press). DH. 1984. Social and affective development
Chang KD, Dienes K, Blasey C, Steiner H, Ketter in infants with a manic-depressive parent.
TA. 2003c. Divalproex in the treatment of Am J Psychiatry 141:223–229.
REFERENCES bipolar offspring with mood and behavioral Geller B, Warner K, Williams M, Zimerman B.
disorders and at least mild affective symp- 1998. Prepubertal and young adolescent
Achenbach TM. 1991. Manual for the child toms. J Clin Psychiatry (in press). bipolarity versus ADHD: assessment and
behavior checklist/4–18 and 1991 profile. Clarke GN, Hornbrook M, Lynch F, Polen M, validity using the WASH-U-KSADS,
Burlington: University of Vermont Depart- Gale J, Beardslee W, O’Connor E, Seeley J. CBCL and TRF. J Affect Disord 51:93–
ment of Psychiatry. 2001. A randomized trial of a group cogni- 100.
Achenbach TM, Edelbrock C. 1983. Manual for tive intervention for preventing depression Geller B, Zimerman B, Williams M, Bolhofner K,
the child behavior checklist and revised in adolescent offspring of depressed parents. Craney JL, Delbello MP, Soutullo CA.
child behavior profile. Burlington: Univer- Arch Gen Psychiatry 58:1127–1134. 2000. Diagnostic characteristics of 93 cases
sity of Vermont Department of Psychiatry. Craddock N, Jones I. 1999. Genetics of bipolar of a prepubertal and early adolescent bipolar
American Psychiatric Association. 1994. Diag- disorder. J Med Genet 36:585–594. disorder phenotype by gender, puberty and
nostic and statistical manual of mental Craddock N, McKeon P, Moorhead S, Guy C, comorbid attention deficit hyperactivity
disorders (DSM-IV). Washington, DC: Harrison D, Mynett-Johnson L, Claffey E, disorder. J Child Adolesc Psychopharmacol
American Psychiatric Association. Feldman E, McGuffin P, Owen MJ, 10:157–164.
Anderson CA, Hammen CL. 1993. Psychosocial O’Donovan MC. 1997. Expanded CAG/ Gershon ES, McKnew D, Cytryn L, Hamovit J,
outcomes of children of unipolar depressed, CTG repeats in bipolar disorder: no correla- Schreiber J, Hibbs E, Pellegrini D. 1985.
bipolar, medically ill, and normal women: a tion with phenotypic measures of illness Diagnoses in school-age children of bipolar
longitudinal study. J Consult Clin Psychol severity. Biol Psychiatry 42:876–881. affective disorder patients and normal con-
61:448–454. Cytryn L, McKnew DH Jr. Bartko JJ, Lamour M, trols. J Affect Disord 8:283–291.
Beardslee WR, Gladstone TR. 2001. Prevention Hamovitt J. 1982. Offspring of patients Goodwin FK, Jamison KR. 1990. Manic-depres-
of childhood depression: recent findings and with affective disorders: II. Journal of the sive illness. New York: Oxford Press.34 AMERICAN JOURNAL OF MEDICAL GENETICS (SEMIN. MED. GENET.) ARTICLE
Goossens D, Del-Favero J, Van Broeckhoven C. 1987. Children of parents with manic- light in young people at high risk for
2001. Trinucleotide repeat expansions: do depressive illness: a follow-up study. Can J affective disorder. A preliminary report.
they contribute to bipolar disorder? Brain Psychiatry 32:563–569. Neuropsychopharmacology 1:217–223.
Res Bull 56:243–257. Lewy AJ, Nurnberger JI Jr, Wehr TA, Pack D, Nurnberger JI, Hamovit J, Hibbs ED, Pelligrini D,
Grigoroiu-Serbanescu M, Christodorescu D, Becker LE, Powell RL, Newsome DA. Guroff JJ, Maxwell ME. 1988b. A high-risk
Jipescu I, Totoescu A, Marinescu E, Arde- 1985. Supersensitivity to light: possible trait study of primary affective disorder: selection
lean V. 1989. Psychopathology in children marker for manic-depressive illness. Am J of subjects, initial assessment and 1- to 2-
aged 10–17 of bipolar parents: psycho- Psychiatry 142:725–727. year follow-up. In: Dunner DL, Gershon
pathology rate and correlates of the severity Li T, Vallada HP, Liu X, Xie T, Tang X, Zhao J, ES, Barrett JE, editors. Relatives at risk for
of the psychopathology. J Affect Disord O’Donovan MC, Murray RM, Sham PC, mental disorder. New York: Raven. p 161–
16:167–179. Collier DA. 1998. Analysis of CAG/CTG 177.
Hammen C, Gordon D, Burge D, Adrian C, repeat size in Chinese subjects with schizo- O’Donovan MC, Guy C, Craddock N, Bowen T,
Jaenicke C, Hiroto D. 1987. Maternal phrenia and bipolar affective disorder using McKeon P, Macedo A, Maier W, Wild-
affective disorders, illness, and stress: risk the repeat expansion detection method. Biol enauer D, Aschauer HN, Sorbi S, Feldman
for children’s psychopathology. Am J Psy- Psychiatry 44:1160–1165. E, Mynett-Johnson L, Claffey E, Nacmias B,
chiatry 144:736–741. Lindblad K, Nylander PO, De bruyn A, Sourey D, Valente J, Dourado A, Grassi E, Lenzinger E,
Hazell PL, Lewin TJ, Carr VJ. 1999. Confirma- Zander C, Engstrom C, Holmgren G, Heiden AM, Moorhead S, Harrison D,
tion that child behavior checklist clinical Hudson T, Chotai J, Mendlewicz J, Van Williams J, McGuffin P, Owen MJ. 1996.
scales discriminate juvenile mania from Broeckhoven C, Schalling M, Adolfsson R. Confirmation of association between
attention deficit hyperactivity disorder. J 1995. Detection of expanded CAG repeats expanded CAG/CTG repeats and both
Paediatr Child Health 35:199–203. in bipolar affective disorder using the repeat schizophrenia and bipolar disorder. Psychol
Hirshfeld-Becker DR, Biederman J, Faraone SV, expansion detection (RED) method. Neu- Med 26:1145–1153.
Violette H, Wrightsman J, Rosenbaum JF. robiol Dis 2:55–62. Ongur D, Drevets WC, Price JL. 1998. Glial
2002. Temperamental correlates of disrup- Lindblad K, Nylander PO, Zander C, Yuan QP, reduction in the subgenual prefrontal cortex
tive behavior disorders in young children: Stahle L, Engstrom C, Balciuniene J, in mood disorders. Proc Natl Acad Sci USA
preliminary findings. Biol Psychiatry 51: Pettersson U, Breschel T, McInnis M, Ross 95:13290–13295.
563–574. CA, Adolfsson R, Schalling M. 1998. Two Patterson GR, DeBaryshe BD, Ramsey E. 1989.
Inoff-Germain G, Nottelmann ED, Radke-Yar- commonly expanded CAG/CTG repeat A developmental perspective on antisocial
row M. 1992. Evaluative communications loci: involvement in affective disorders? behavior. Am Psychol 44:329–335.
between affectively ill and well mothers and Mol Psychiatry 3:405–410. Pellegrini D, Kosisky S, Nackman D, Cytryn L,
their children. J Abnorm Child Psychol Lish JD, Dime-Meenan S, Whybrow PC, Price McKnew DH, Gershon E, Hamovit J,
20:189–212. RA, Hirschfeld RM. 1994. The National Cammuso K. 1986. Personal and social
Kashani JH, Burk JP, Horwitz B, Reid JC. 1985. Depressive and Manic-Depressive Associa- resources in children of patients with bipolar
Differential effect of subtype of parental tion (DMDA) survey of bipolar members. J affective disorder and children of normal
major affective disorder on children. Psy- Affect Disord 31:281–294. control subjects. Am J Psychiatry 143:856–
chiatry Res 15:195–204. Masi G, Toni C, Perugi G, Mucci M, Millepiedi S, 861.
Kestenbaum CJ. 1979. Children at risk for manic- Akiskal HS. 2001. Anxiety disorders in Post RM. 1992. Transduction of psychosocial
depressive illness: possible predictors. Am J children and adolescents with bipolar dis- stress into the neurobiology of recurrent
Psychiatry 136:1206–1208. order: a neglected comorbidity. Can J affective disorder. Am J Psychiatry
Kestenbaum CJ. 1980. Adolescents at risk for Psychiatry 46:797–802. 149:999–1010.
manic-depressive illness. Adolesc Psychiatry McDonough-Ryan P, Shear PK, Ris D, DelBello Radke-Yarrow M, Nottelmann E, Martinez P,
8:344–366. M, Graman S, Rosenberg HL, Strakowski S. Fox MB, Belmont B. 1992. Young chldren
Klein DN, Depue RA, Slater JF. 1985. Cyclothy- 2000. IQ and achievement in children of of affectively ill parents: a longitudinal study
mia in the adolescent offspring of parents bipolar parents. Clin Neuropsychol 14:248. of psychosocial development. J Am Acad
with bipolar affective disorder. J Abnorm McDonough-Ryan P, DelBello M, Shear PK, Ris Child Adolesc Psychiatry 31:68–77.
Psychol 94:115–127. DM, Soutullo C, Strakowski SM. 2002. Rosenberg DR, Sweeney JA, Squires-Wheeler E,
Klimes-Dougan B, Free K, Ronsaville D, Stilwell Academic and cognitive abilities in children Keshavan MS, Cornblatt BA, Erlenmeyer-
J, Welsh CJ, Radke-Yarrow M. 1999. of parents with bipolar disorder: a test of the Kimling L. 1997. Eye-tracking dysfunction
Suicidal ideation and attempts: a long- nonverbal learning disability model. J Clin in offspring from the New York High-Risk
itudinal investigation of children of Exp Neuropsychol 24:280–285. Project: diagnostic specificity and the role of
depressed and well mothers. J Am Acad McKnew DH Jr, Cytryn L, Efron AM, Gershon attention. Psychiatry Res 66:121–130.
Child Adolesc Psychiatry 38:651–659. ES, Bunney WE Jr. 1979. Offspring of Soutullo C. 2000. Early mood symptoms in
Kovacs M, Pollock M. 1995. Bipolar disorder and patients with affective disorders. Br J children of bipolar parents vs. controls. In:
comorbid conduct disorder in childhood Psychiatry 134:148–152. Villani S, editor. 47th Annual Meeting of
and adolescence. J Am Acad Child Adolesc Meira-Lima IV, Zhao J, Sham P, Pereira AC, the American Academy of Child and
Psychiatry 34:715–723. Krieger JE, Vallada H. 2001. Association and Adolescent Psychiatry. New York: Amer-
Kuyler PL, Rosenthal L, Igel G, Dunner DL, linkage studies between bipolar affective ican Academy of Child and Adolescent
Fieve RR. 1980. Psychopathology among disorder and the polymorphic CAG/CTG Psychiatry. p 114.
children of manic-depressive patients. Biol repeat loci ERDA1, SEF2-1B, MAB21L Strakowski SM, DelBello MP, Adler C, Cecil
Psychiatry 15:589–597. and KCNN3. Mol Psychiatry 6:565–569. DM, Sax KW. 2000. Neuroimaging in
Lapalme M, Hodgins S, LaRoche C. 1997. Mendlewicz J, Lindbald K, Souery D, Mahieu B, bipolar disorder. Bipolar Disord 2:148–
Children of parents with bipolar disorder: a Nylander PO, De Bruyn A, Zander C, 164.
metaanalysis of risk for mental disorders. Engstrom C, Adolfsson R, Van Broeckho- Strakowski SM, Adler CM, DelBello MP. 2002.
Can J Psychiatry 42:623–631. ven C, Schalling M, Lipp O. 1997. Volumetric MRI studies of mood disorders:
Laroche C, Cheifetz PN, Lester EP. 1981. Expanded trinucleotide CAG repeats in do they distinguish unipolar and bipolar
Antecedents of bipolar affective disorders families with bipolar affective disorder. Biol disorder? Bipolar Disord 4:80–88.
in children. Am J Psychiatry 138:986–988. Psychiatry 42:1115–1122. Vaughn CE, Leff JP. 1976. The influence of family
LaRoche C, Cheifetz P, Lester EP, Schibuk L, Miklowitz DJ, Goldstein MJ, Nuechterlein KH, and social factors on the course of psychia-
DiTommaso E, Engelsmann F. 1985. Psy- Snyder KS, Mintz J. 1988. Family factors tric illness. A comparison of schizophrenic
chopathology in the offspring of parents and the course of bipolar affective disorder. and depressed neurotic patients. Br J Psy-
with bipolar affective disorders. Can J Arch Gen Psychiatry 45:225–231. chiatry 129:125–137.
Psychiatry 30:337–343. Nurnberger JI Jr, Berrettini W, Tamarkin L, Wals M, Hillegers MH, Reichart CG, Ormel J,
Laroche C, Sheiner R, Lester E, Benierakis C, Hamovit J, Norton J, Gershon E. 1988a. Nolen WA, Verhulst FC. 2001. Prevalence
Marrache M, Engelsmann F, Cheifetz P. Supersensitivity to melatonin suppression by of psychopathology in children of a bipolarARTICLE AMERICAN JOURNAL OF MEDICAL GENETICS (SEMIN. MED. GENET.) 35
parent. J Am Acad Child Adolesc Psychiatry genetic risk for affective disorder. Arch Gen Zahn-Waxler C, Mayfield A, Radke-Yarrow M,
40:1094–1102. Psychiatry 46:1120–1124. McKnew DH, Cytryn L, Davenport YB.
Waters BG, Marchenko-Bouer I, Smiley D. 1981. Zahn TP, Nurnberger JI Jr, Berrettini WH, 1988. A follow-up investigation of offspring
Educational achievement, IQ and affective Robinson TN Jr. 1991. Concordance be- of parents with bipolar disorder. Am J
disorder in the adult offspring of bipolar tween anxiety and autonomic nervous system Psychiatry 145:506–509.
manic-depressives. Br J Psychiatry 139:457– activity in subjects at genetic risk for affective Zander C, Schurhoff F, Laurent C, Chavand O,
462. disorder. Psychiatry Res 36:99–110. Bellivier F, Samolyk D, Leboyer M, Allilaire
Weintraub S. 1987. Risk factors in schizophrenia: Zahn-Waxler C, Cummings EM, McKnew DH, JF, Cann H, Neri C, Mallet J. 1998. CAG
the Stony Brook High-Risk Project. Schi- Radke-Yarrow M. 1984. Altruism, aggres- repeat sequences in bipolar affective dis-
zophr Bull 13:439–450. sion, and social interactions in young order: no evidence for association in a
Zahn TP, Nurnberger JI Jr, Berrettini WH. 1989. children with a manic-depressive parent. French population. Am J Med Genet 81:
Electrodermal activity in young adults at Child Dev 55:112–122. 338–341.You can also read