Can NBTXR3 turn anti-PD-1 non responders into responders and deepen anti-PD-1 response in naïve patients? - Nanobiotix
←
→
Page content transcription
If your browser does not render page correctly, please read the page content below
Can NBTXR3 turn anti-PD-1
non responders into responders
and deepen anti-PD-1 response in
naïve patients?
Study 1100 Virtual KOL Event
June 11,
1 2021Important Notice and Disclaimer
Information in this presentation, and the accompanying discussion, contains forward-looking statements. All statements other than statements of historical facts
regarding Nanobiotix S.A. and our subsidiaries (together, “Nanobiotix” or the “Company”) are forward looking statements. Forward-looking statements in this
presentation include, but are not limited to, statements about: the Company’s future prospects; clinical outcomes, which may materially change as patient
enrollment continues and more extensive and longer-term patient data become available; the timing and ability to progress the clinical trials of NBTXR3; the
potential benefits of NBTXR3, alone or in combination with other treatments; the Company’s overall development strategy, regulatory calendar and anticipated
milestones; opportunities presented by preclinical data; and financial opportunities and requirements.
Forward-looking statements reflect management’s current beliefs and expectations and are subject to a variety of risks and uncertainties that may cause the
Company’s actual results, levels of activity, performance, achievement or success to be materially different from those anticipated by the statements. These
factors may include risk and uncertainties that are not yet known or determinable. Accordingly, you should not place undue reliance on forward-looking
statements.
Caution should be exercised when interpreting results from separate trials involving separate product candidates. There are differences in the clinical trial
design, patient populations, and the product candidates themselves, and the results from the clinical trials of distinct product candidates may have no
interpretative value with respect to our existing or future results. Similarly, caution should be exercised when interpreting results relating to a small number of
patients or individually presented case studies.
The information presented today is provided as of the date of this Presentation only and may be subject to significant changes at any time without notice.
Except as required by law, Nanobitiotix declines any obligation to update any forward-looking statements, whether as a result of new information, future events
or otherwise.
Important additional information about the risks and uncertainties to which the Company is subject are discussed in greater detail in the information that
Nanobiotix has published in its Annual Report on Form 20-F filed with the U.S. Securities and Exchange Commission on April 7, 2021 and in its universal
registration document filed with the French Financial Markets Authority (Autorité des marchés financiers) under number D.21-0272 on April 7, 2021 (copies of
which are available on www.nanobiotix.com), as well as in any other reports filed with the SEC and the AMF.
This presentation is not, and should not be construed as, an offer of any securities and is not to be construed as providing investment advice. The information
is not directed to, or intended for use by, any citizen or resident of, or person located in, any jurisdiction where such direction or use would be contrary to law or
regulation or which would require any registration or licensing within such jurisdiction.
2Speaker Disclosures
Jared Weiss Colette Shen Tanguy Seiwert James Welsh
Employment: Employment: Employment: Employment:
University of North Carolina University of North Carolina Bloomberg-Kimmell Institute for University of Texas MD Anderson
Lineberger Comprehensive Cancer Lineberger Comprehensive IO/HNC Program, Johns
Founder: Healios Oncology,
Center Cancer Center Hopkins
MolecularMatch.com, OncoResponse
Equity and Other Ownership Equity Ownership: Alpine, Checkmate, Mavu,
Interests: Achilles Therapeutics, Research Support: Advisory role: Legion Healthcare Partners, MolecularMatch,
Nektar, Vesselon, Iovance NanoRobotix, OncoResponse, Reflexion
Biotherapeutics, Achilles Nanobiotix, AstraZeneca Nanobiotix, MSD/Merck,
Therapeutics, Nektar, Vesselon, Regeneron, Innate Pharma, Research Support: BMS, Incyte, GSK, Merck,
Iovance Biotherapeutics Bristol-Myers (BMS), eTheRNA, Mavu, CheckMate, Nanobiotix, Alkermes,
Surface Oncology Takeda, Varian
Research Support:
Advisor: Steering Committee: Trademarks: RadScopalTM
Merck, AstraZeneca/MedImmune,
Amgen, Carefusion, G1 Nanobiotix BioNTech, Nektar, Astra- Patents: MP470 (amuvatinib), MRX34
Therapeutics,Immunicum, Loxo/Lilly Zeneca regulation of PDL1, XRT technique to
overcome immune resistance
Research funding (PI):
Consulting or Advisory Role:
Joint steering committee: Nanobiotix
Jounce; MSD/Merck; Astra-
AstraZeneca, EMD Serono, Zeneca Advisor: Nanobiotix, Astra Zeneca, Merck,
Genentech, Inivata, Celgene, G1 BMS, Legions Healthcare partners
Therapeutics, Jounce Therapeutics, Trial funding (PI):
Abbvie, Rakuten, Nanobiotix, Azitra, Scientific Advisory Board: RefleXion Medical,
Bristol-Myers (BMS); Astra-
Eli Lilly, Blueprint Medicines, Pfizer, MolecularMatch, OncoResponse, CheckMate,
Zeneca; Nanobiotix,
Saatchi Wellness, Jazz Alpine, NanoRobotics, Xpheylum, GI
MSD/Merck, Cue Therapeutics
Pharmaceuticals, Boehringer Innovation, Mavu, Reflexion, Aileron
Ingelheim, Regeneron, Genmab, Therapeutics, Ventana
SDP Oncology
38:00 AM ET OPENING REMARKS
• Jeffrey Bockman, PhD, EVP, Oncology Practice Head, Cello Health BioConsulting
Agenda
8:05 AM ET NBTXR3 MODE OF ACTION
• Laurent Levy, PhD, CEO and Founder, Nanobiotix
OVERVIEW OF TREATMENT LANDSCAPE: PROMISE AND LIMITATIONS OF I/O, AND
8:10 AM ET RATIONAL FOR COMBINATION-BASED APPROACHES IN I/O
• Jared Weiss, MD, Associate Professor of Medicine, University of North Carolina Lineberger Comprehensive Cancer
Center
8:20 AM ET NANOBIOTIX STUDY 1100 SAFETY AND EFFICACY DATA PRESENTATION
•Colette Shen, MD, PhD, Assistant Professor, Radiation Oncology
University of North Carolina Lineberger Comprehensive Cancer Center
•Tanguy Seiwert, MD, Director, Head & Neck Cancer Oncology Disease Group, Co-Director Bloomberg-Kimmell Institute
for IO/HNC Program, Assistant Professor, Oncology, Johns Hopkins
NBTXR3 AS POTENTIAL COMBO AGNOSTIC PRODUCT, PRECLINICAL RATIONAL AND
8:40 AM ET FUTURE OPPORTUNITY
• James Welsh, MD, Associate Professor, University of Texas, MD Anderson Cancer Center
DISCUSSION AND Q&A- IMPLICATIONS OF STUDY 1100 IN HEAD AND NECK CANCER
8:50 AM ET SPACE
• ALL
9:10 AM ET SUMMARY CLOSE
• Jeffrey Bockman, PhD, EVP, Oncology Practice Head, Cello Health BioConsulting
4Nanobiotix Offers a Powerful Orthogonal Approach to
Modulate the TME & Augment CPIs & Other IO Agents
10NBTXR3 Mode of Action
LAURENT LEVY, PhD
CEO AND FOUNDER, NANOBIOTIX
11Radiation Remains the Most Widely Used Oncology Treatment
Radiotherapy Is the most
common treatment…
% RECEIVING RTX NUMBER OF PATIENTS
87% Breast cancer 1,800,000
77% Lung cancer 1,600,000
60% 74% H&N 700,000
18M
new patients
RTx 58% Prostate 740,000
60% Rectum 420,000
per year
diagnosed 49% Pancreas 225,000
with cancer 80% CNS 237,000
worldwide
… …
12
Source: * World Health Organization (2014); **RADIATION THERAPY EQUIPMENT – A global strategic business report 08/06 ; Delaney et al. 2015; Globocan 2018But Still Presents Significant Unmet Medical Needs
...But still presents significant
unmet medical needs
Inadequate local control
(Local invasion or systemic expansion)
60% Inadequate systemic control
18M
new patients
RTx
(metastatic patients)
per year Acute and long-term AEs
diagnosed
with cancer
(dose de-escalation/re-irradiation)
worldwide
13
Source: * World Health Organization (2014); **RADIATION THERAPY EQUIPMENT – A global strategic business report 08/06 ;NBTXR3: Potential First-In-Class, Tumor Agnostic, Combination
Agnostic Radioenhancer
Aqueous suspension of inorganic crystalline
hafnium oxide (HfO2) nanoparticles
Nanosized to enter the cell and designed to
strongly absorb ionizing radiation
Universal mode of action targeting all solid tumors
14NBTXR3: Potential First-In-Class, Tumor Agnostic, Combination
Agnostic Radioenhancer
One-time intratumoral administration
Remains in tumor
Integrates into current patient flow, uses standard
equipment and standard radiation therapy
15Radiotherapy (RT) NBTXR3
NBTXR3 Alone Activated by RT
Dose Dose
Hyper-
Focused Dose
Delivery in the
9X
dose* around
Usual nanoparticles
Heart of the dose
delivered
Cell Radiotherapy in the cell
X-Rays X-Rays Clusters of
Nanoparticles
Local absorption of
energy
*Dose enhancement determined by Monte Carlo simulation (CEA Saclay, France). In vitro data. In House Data.
161- physical destruction of cancer cell for local control
IRRADIATED lesion
Lesion Size
Injected lesion
Decrease
Direct Cell Death
X-Rays (apoptosis, necrosis)
Tumor
NBTXR3 antigen
Universal Dendritic cell
NON-IRRADIATED lesion
Systemic Effect activation
Mode of Action
Non-Injected
Local Effect
CD4 & CD8 T
cell activation
2- subsequent effect priming the immune response
Maggiorella et al. Future Oncol. 2012;8(9):1167-1181;
Thariat et al. aInt J Radiat Oncol Biol Phys. 2019;105(1S):E651. Abs 3513.;
Marill et al. Radiother Oncol. 2019;141:262-266;
Zhang et al. Int J Nanomedicine. 2020;15:3843-3850;
Shen et al. J Clin Oncol. 2020;38(15_suppl):TPS3173-TPS.
The scientific information discussed in this presentation related to NBTXR3 is preliminary and investigative. NBTXR3 is not approved by the U.S.
Food and Drug Administration; therefore, no conclusions can nor should be drawn regarding the safety or effectiveness of the investigational product. 17Proof-of-Concept Established in randomized PII/III
and EU Marketing Authorization Secured in Soft Tissue Sarcoma
Doubling of Pathological Complete Response in Phase II/III RESULTS
Pathological Complete Response • Achieved its primary endpoint of pathological CRR
Rate • Achieved its secondary endpoint in quality of
-ITT Full Analysis Set margins (R0)
• Demonstrated long-term persistent bioavailability
20 p-value 0.0448* • No impact on patient ability to receive planned
18 dose of RT
16
PUBLISHED IN LANCET ONCOL. 2019
14 16.1%
12
10
8
6
7.9%
4
2
0
NBTXR3 activated by RT RT alone (N=89)
(N=87)
18Focused Development Strategy
Leverage Proof of Concept in Soft Tissue Sarcoma
Secure Initial US Approval as a Single Agent in
01 Locally Advanced HNSCC
Establish NBTXR3 as a Pillar of Immunotherapy in
02 Combination with Anti-PD-1 Agents in Advanced Cancers
Expand Tumor-Agnostic and Combination-Agnostic
03 Approaches Through Key Strategic Alliances
19Evaluating Tumor Agnostic, Combination Agnostic NBTXR3
Capabilities
Strategic
Indication IND Phase I Phase II Phase III Post market Partner 2021 Milestones
Study 301: STS of Extremity & Trunk Wall
Soft Tissue Sarcoma
Study 401: STS of Extremity & Trunk Wall
Single Agent
Study 102: Locally Advanced H&N Expansion Data: Q2 21
Head & Neck
Nanoray 312: Locally Advanced H&N* Phase III Initiation: H2 21
Liver Study 103: Hepatocellular & Liver Mets
Pancreas Locally Adv. or Borderline Resectable
NSCLC Re-irradiation, Locoregional recurrence Expected Phase I Initiation: H1 21
Recurrent
Head & Neck, Lung or Study 1100: H&N, Lung or Liver Metastasis Data Update: Q2 21
Liver Metastasis
+Immunotherapy
Inoperable Locoregional Recurrent
Expected Phase I Initiation : H1 21
(Re-Irradiation)
Combination
Head & Neck
R/M with Limited PD-L1 Expression
or Refractory Expected Phase II Initiation : H1 21
Advanced Solid Tumors with Lung
Solid Tumors Or Liver Metastasis with anti-CTLA-4 Expected Phase I Initiation : H1 21
And Anti-PD-1/L1 plus RadScopalTM
Esophagus Adenocarcinoma Initiated Q1 21
+Chemo
Positive P1 Results and RP2D Reported at
Rectal Locally Advanced or Unresectable*
CONFIDENTIAL ASCO GI3 May 2021 20
*Phase I/II Study initiated by former partner, PharmaEngine. In conjunction with the termination of the license and collaboration agreement, PharmaEngine will implement the early termination and wind-down of this clinical trial in accordance with good clinical practice guidelines. The trial will be deemed completed when all enrolled
patients have reached “end-of-study” and PharmaEngine issues a final study report in accordance with good clinical practice guidelinesOverview of Treatment Landscape in HNSCC: Promise and
Limitations of IO
and
Rationale for Combination-Based Approaches
Jared Weiss, MD
Associate Professor of Medicine
University of North Carolina Lineberger Comprehensive Cancer Center
21The Promise and Limitations of IO Agents
IO has been practice changing and life changing for many ……….But continues to leave many patients out in the
patients with cancer “cold”
KEYNOTE-177 in mMSI-H/dMMR CRC (1) KEYNOTE-048 in R/M HNSCC (4)
Pembrolizumab
Chemotherapy Pembrolizumab alone
Cetuximab with chemotherapy
PFS (%)
PFS (%)
HR 0.6, 95% CI, 0.45-0.80), P=0.0002
HR 0.92, 95% CI, 0.77-1.10),
P=0.1697
No. at risk No. at risk
Pembrolizumab Pembrolizumab alone
Chemotherapy Cetuximab + CT
KEYNOTE-010 in 2L PD-L1+ adv. NSCLC (2) KEYNOTE-002 in mMelanoma (3) KEYNOTE-061 in 2L adv. Gastric (5) 4 Accelerated Approvals with IO agents see
Voluntary withdrawal- FDA
Pembrolizumab 2 mg/kg Pembrolizumab
Pembrolizumab 2 mg/kg* Paclitaxel
Pembrolizumab 10 mg/kg** Pembrolizumab 10 mg/kg
Docetaxel Chemotherapy
HR 1.27 (95% CI, 1.03-1.57)
• Nivolumab for mSCLC
PFS (%)
PFS (%)
* HR 0.59, 95% CI, 0.44-0.78, * HR 0.57, 95% CI, 0.45-0.73,
PFS (%)
P=0.0001
** HR 0.59, 95% CI, 0.45-0.78,
P=0.0001
** HR 0.50, 95% CI, 0.39-0.64,
• Durvalumab for LA/metastatic
P=0.0001 P=0.0001
urothelial carcinoma
• Pembrolizumab for treatment of
patients with mSCLC
No. at risk
Pembrolizumab 2 mg/kg
• Atezolizumab for LA or metastatic
No. at risk
Pembrolizumab 2 mg/kg
Pembrolizumab 10 mg/kg
No. at risk
urothelial carcinoma
Chemotherapy Pembrolizumab
Pembrolizumab 10 mg/kg
Paclitaxel
Docetaxel
(1) André et al. NEJM 2020; (2) Herbst et al. Lancet 2015 (3) Ribas et al. Lancet Oncol 2015; (4) Burness et al. Lancet 2019; (5) Shitara et al. Lancet 2018. 22
PFS = progression-free survivalEven Among “Hot” Tumor Types, Most Patients Experience
Primary or Secondary Resistance
KEYNOTE-048 in R/M HNSCC
12-mo rate
19.6%
11.9%
Primary resistant patients
Median (95% CI)
24-mo rate 3.2 mos (2.2-3.4)
11.2% 5.0 mos (4.8-5.8)
5.4%
Secondary resistant patients
Long term responders
Months
*Burtness B, et al. “Pembrolizumab alone or with chemotherapy versus cetuximab with chemotherapy for recurrent or metastatic squamous cell carcinoma of the head and neck 23
(KEYNOTE-048): a randomized, open-label, phase 3 study.” Lancet. 2019 Nov 23;394(10212):1915-1928.Less than 13% of eligible patients respond to checkpoint inhibitors
24
JAMA Network Open. 2019;2(5):e192535. doi:10.1001/jamanetworkopen.2019.2535 (Downloaded From: https://jamanetwork.com/ on 04/29/2021)New IO Trials in combination with RT in HNSCC show no improvement in
outcome
PEMBRORAD STUDY (1) JAVELIN STUDY (2) MSKCC: NIVO vs NIVO+SBRT (3)
Pembro-RT does not improve outcome vs cetux-RT Addition of avelumab to CRT does not improve outcome Addition of RT to nivo does not improve OS
OS
OS PFS
OS
Overall Survival
LRC PFS
Progression Free survival (%)l
1. Yao et al. Pembrolizumab versus cetuximab, concomitant with radiotherapy (RT) in LA-HNSCC: Results of the GORTEC 2015-01 “PembroRad” randomized trial Annals of Oncology
(2020) 31 (suppl_4): S1142-S1215.
2. Avelumab plus standard-of-care chemoradiotherapy versus chemoradiotherapy alone in patients with locally advanced squamous cell carcinoma of the head and neck: a randomised, double-blind, 25
placebo-controlled, multicentre, phase 3 trial
3. McBride S. et al.. A Randomized Phase II Trial of Nivolumab With SBRT Versus Nivolumab Alone in Metastatic Head and Neck Squamous Cell Carcinoma J Clin Oncol 39:30-37. 2020The Unique Potential of NBTXR3
Illustrative Purposes Only PMID: 19707528
NBTXR3 designed to addresses both local and distant
control
26Rationale for combining NBTXR3 with immunotherapy
cGAS-STING A primary physical MOA that is tumor agnostic
micronuclei IFNb
Triggering subsequent multiple biological
TAA release pathways for priming adaptative immune
response
ATP ICD
Physical priming: potential CPi agnostic agent
HMGB1
There is a high unmet need and NBTXR3 may:
▪ Enhance the therapeutic index of radiotherapy
Calreticuline maximizing local effect,
▪ Increase the local efficacy of immunotherapy, and
Immunopeptidome ▪ Improve distant tumor control via a systemic effect
Other ▪ Potential long-term effect with memory t-cells
IO= immuno-oncology; RT = radiotherapy. 27
1. Sharma et al., Cell. 2015. 2. Hwang Wl et al., Nat Rev Clin Oncol. 2018. 3. Postow MA, et al., N Engl J Med. 2012Starting the IO Fire with NBTXR3
“Cold” Tumor Add in IO No Change
“Spark” with NBTXR3 and RT Add in IO “Hot” Tumor
28Study 1100: Overall Results
Colette Shen, MD, PhD
Assistant Professor, Radiation Oncology
University of North Carolina Lineberger Comprehensive Cancer Center
29Study 1100
Phase I study of intratumoral NBTXR3 in
combination with
Anti-PD-1 in patients with advanced cancers
Colette Shen1, Jessica Frakes2, Jiaxin Niu3, Jared Weiss1, Jimmy Caudell2, Katherine
Jameson4, Patricia Said4, Tanguy Seiwert5
1-University of North Carolina School of Medicine, Chapel Hill, North Carolina, USA; 2-Moffitt Cancer Center, Tampa, Florida, USA; 3-Banner
MD Anderson Cancer Center, Gilbert Arizona, USA; 4-Nanobiotix, Paris, France; 5-Johns Hopkins Medicine, Baltimore, Maryland, USA
30Study 1100
Study 1100:
A phase I study of NBTXR3 activated by radiotherapy for patients with advanced cancers treated with an Anti-PD-1 therapy.
Head and –Neck
HNSCC Cohort 1
cancers Mets – Cohort 2
Lung mets Mets – Cohort 3
Liver mets
Liver
• Inoperable LRR or R/M HNSCC • Cancer metastasized to the lung • Cancer metastasized to the liver
• Tumor in previously irradiated field • Tumor not previously irradiated • Tumor not previously irradiated
• Amenable to re-irradiation • Indicated to receive Anti-PD-1 • Indicated to receive Anti-PD-1
• Anti-PD-1 naïve or non-responder • Anti-PD-1 naïve or non-responder • Anti-PD-1 naïve or non-responder
31Study 1100: Phase I Basket Trial of NBTXR3 in Combination with
Anti-PD-1 Checkpoint Inhibitors
Patients with recurrent head & neck cancer or with lung or liver metastases from any primary
cancer eligible for anti-PD-1 therapy
1
LRR or R/M HNSCC
35Gy will be delivered in
Key Inclusion Criteria 5 fractions of 7Gy Endpoints
• Anti-PD-1 Naïve; or • Primary: Recommended
• Anti-PD-1 Resistant: 2 Phase 2 Dose
Anti-PD-1
• meets criteria Lung Metastases
consistent with anti-PD-
washout for • Secondary: ORR, Safety
45Gy will be delivered in
1 primary resistance , or non- 5 fractions of 9Gy
and Feasibility, and Body-
responders Kinetics
• meets criteria
consistent with anti-PD- • Exploratory: Survival
1 secondary resistance 3 Outcomes, Duration of
Response, and
Liver Metastases Biomarkers of Response
45Gy will be delivered in
3 fractions of 15Gy
32Study 1100: Graphical Study Design
Screening Treatment period Follow-up
Anti-PD-1 washout for non- NBTXR3 injection, RT activation, and anti-PD-1 combination Continued anti-PD-1 for all
responders
Cohort 1: LRR or R/M HNSCC
35Gy will be delivered in 5 fractions of 7Gy
Cohort 2: Lung Metastases
45Gy will be delivered in 5 fractions of 9Gy
Cohort 3: Liver Metastases
45Gy will be delivered in 3 fractions of 15Gy
Radiation Radiation
Inclusion/Exclusion, Therapy Therapy
Tumor volume Planning Radiation Therapy Recovery
5-14d total 5-15d total 4w total
D -28 D1 D2 D7-16 D13-32 D40-59
NBTXR3 Administration PD-1 administration EoT Visit
NBTXR3 visualization
3316 Patients Treated Across 3 Cohorts
Cohort 1 (H&N Re-Irradiation) Cohort 2 (Lung Mets) Cohort 3 (Liver Mets)
n=16
Patient No. A D F J K L N B C E H O P G I M
Primary
H&N H&N H&N H&N H&N H&N H&N H&N Lung H&N Lung H&N H&N H&N Lung H&N
Tumor
Prior
Naïve 1° NR Naïve Naïve Naïve 1° NR Naïve 2° NR 1° NR 1° NR 1° NR Naïve 1° NR 2° NR 1° NR Naïve
Anti-PD-1
PD-L1
Unk Unk Unk Neg Pos Neg Pos Unk Pos Unk Neg Pos Unk Pos Neg Neg
Expression
Study 1100
CR SD* Unk PR N/A SD SD PR PR SD PD PR Unk CR SD SD
BOR
Study 1100
1 4 2 0 1 0 0 0 0 2 6 0 0 0 0 0
SAEs
*Patient D is classified SD as per RECIST 1.1 but had a complete pathological response based on a biopsy sample located in target lesion 34
Source: NBTXR3-1100 - Cut-off date:23Apr2021AE Profile Has Not Differed in Type Or Grade From What Is
Expected with RT or Anti-PD-1 Agents
SAE NBTXR3 or injection-related event, by PT and worst NCI-CTCAE grade – All treated population
Level 1 (22%) Level 2 (33%)
Cohort 1 Cohort 2 Cohort 3 Cohort 2
Cohort/# Patients HNSCC Lung Mets Liver Mets Lung Mets Overall
N=7 N=4 N=3 N=2 N=16
Grade Grade Grade Grade Grade Grade Grade Grade Grade Grade
Preferred Term
1-2 3+ 1-2 3+ 1-2 3+ 1-2 3+ 1-2 3+
Fall 0 0 0 1 0 0 0 0 0 1
Hyperglycemia 0 1 0 0 0 0 0 0 0 1
Pneumonitis 0 1 0 0 0 0 0 0 0 1
Soft Tissue Necrosis 0 1 0 0 0 0 0 0 0 1
Note: Incidence is calculated as the number of patients with at least an AE in a given category (PT, grade) on the total number of
patients, by level and cohort or overall.
*1 HNSCC anti-PD-1 naïve patient (cohort 1) died from pneumonitis ~2 months post-NBTXR3 injection, related to anti-PD-1 and possibly related to NBTXR3 35
Source: NBTXR3-1100 - Cut-off date:23Apr202110 Out of 13 Evaluable Patients Had Tumor Regression
Regardless of Prior Anti-PD-1 Exposure
Best Observed Response by RECIST 1.1 as per Investigator Assessment
By Primary Tumor By Previous Exposure to Anti-PD-1 Therapy
HNSCC NSCLC Anti-PD-1 naïve Anti-PD-1 non-responder
40 40
PD PD
All target lesions sum of diameters
All target lesions sum of diameters
20 20
change from baseline (%)
change from baseline (%)
0 0
SD SD
-20
-20 * *
-40 -40
-60 -60
PR PR
-80 -80
** ** CR
-100 CR -100
Patient: H I M N L D E J C B O A G Patient: H I M N L D E J C B O A G
*patient D: pCR based on biopsy sample located in the target lesion; **Unconfirmed Response 36
Source: NBTXR3-1100 - Cut-off date:23Apr2021Tumor Regression in 76.9% of Evaluable Patients Regardless of
Prior Anti-PD-1 Exposure
*Of which 1 pCR based on biopsy sample located in the target lesion (patient D)
**Clinically meaningful regression defined as > 10% regression in all target lesions from baseline
1. Ott PA, Bang YJ, Piha-Paul SA, Razak ARA, Bennouna J, Soria JC, et al. T-Cell-Inflamed Gene-Expression Profile, Programmed Death Ligand 1 Expression, and Tumor 37
Mutational Burden Predict Efficacy in Patients Treated With Pembrolizumab Across 20 Cancers: KEYNOTE-028. J Clin Oncol. 2019;37(4):318-27. 2.Gong J, Chehrazi-Raffle A,
Reddi S, Salgia R. Development of PD-1 and PD-L1 inhibitors as a form of cancer immunotherapy: a comprehensive review of registration trials and future considerations. J
Source: NBTXR3-1100 - Cut-off date:23Apr2021 Immunother Cancer. 2018;6(1):8.Study 1100: Response by Prior Anti-PD-1 Exposure
Tanguy Seiwert, MD
Director, Head & Neck Cancer Oncology Disease Group,
Co-Director Bloomberg-Kimmell Institute for IO/HNC Program,
Assistant Professor, Oncology, Johns Hopkins
38Deep Responses Maintained Over Time Regardless of Anti-PD-1
Exposure
PD-1 Naive (ASCO 2021
Anti-PD-1 Data)
Naïve
All target lesions sum of diameters
50
change from baseline (%)
PD A
20 J
0 M
SD
N
-30 O
-50
PR
-100 CR
0 100 200 300 400 500 600 700
Study Day
• 4 of 5 evaluable patients had tumor regression
• 60% (3/5) of patients had investigator-assessed
objective response, including 1 CR by RECIST 1.1
39
Source: NBTXR3-1100 - Cut-off date:23Apr2021Deep Responses Maintained Over Time Regardless of Anti-PD-1
Exposure
PD-1 Anti-PD-1
Non-Responders (ASCO 2021 Data)
Non-Responders
All target lesions sum of diameters
50
change from baseline (%)
PD B
20 C
0 SD D
E
-30 G
-50 * H
PR
I
CR L
-100
0 100 200 300 400
Study Day
• 6 of 8 evaluable patients had tumor regression
• 50% (4/8) had investigator-assessed objective
response (1 CR and 2 PR by RECIST 1.1, and 1 pCR)
*Patient D: pathological CR (pCR) based on biopsy sample located in the target lesion 40
Source: NBTXR3-1100 - Cut-off date:23Apr2021Possible Immune Response and Abscopal Effect?
Stage IV NSCLC – Stage IV NSCLC – Stage IV HNSCC – Stage IV HNSCC – naïve (J)
non responder (C) non responder (I) non responder (L) PD-L1 expression is equal to 0% by TPS at baseline
14 months ongoing survival 9 months ongoing survival 4 months ongoing survival 4 months ongoing survival
Baseline%(%)
Baseline%(%)
%(%)
Non-NBTXR3-Injected lesions
Change,(%)
%
Baseline
are Non-Target lesions
from Change,
50
fromChange,
from Baseline
50
fromChange,
50 50 50 50
Best Overall Change, %
Best Overall Change, %
50 NBTXR3 Injecte
Best Overall Change, %
PD PD PD NBTXR3 Injected
PD NBTXR3 Injected PD PD Injected
NBTXR3 PD
PD
20 20 20 Non-NBTXR3-Injected 20 20 Non-NBTXR3-Injected 20 Non-NBTXR3-In
20 Non-NBTXR3-Injected
Lesions
Lesions
Lesions
0 0
Lesions
SD 0 0 Non-NBTXR3-Injected
SD 0 Non-NBTXR3-Injected 0
SD SD 0 SD Non-NBTXR3-Injected SD SD SD
Change
Change
Change
-30 -30 -30 -30 -30 -30
Change
-30
All Measurable
All Measurable
All Measurable
-50
All Measurable
-50 -50 -50 -50 -50 -50
PR PR PR PR PR PR
PR PR
Diameters
Diameters
Diameters
Diameters
CR CR-100CR CR CR CR
-100-100 -100 CR -100 CR -100
0 0 100 -100
0 100 100 200 0 100 0 100 0 100
Study Day Study Day 0 100
Study Day Study Day Study Day Study Day
Study Day
3/4 NR patients experienced tumor 1/1 naïve patient experienced tumor
reduction in lesions that did not receive reduction in lesions that did not receive
NBTXR3* NBTXR3
*lesion may have received low-dose radiation due to vicinity to targeted treatment area 41
Source: NBTXR3-1100 - Cut-off date:23Apr2021Possible Immune Response and Abscopal Effect?
Stage IV NSCLC – Stage IV NSCLC –
non responder (C) non responder (C)
All target lesions sum of diameters
Baseline%(%)
Non-NBTXR3-Injected lesions
are Non-Target lesions *
change from baseline (%)
from Change,
0 50 50
PD PD NBTXR3 Injected PD
20 20
20 Non-NBTXR3-Injected
Lesions
0 0
SD 0 SD Non-NBTXR3-Injected SD
Change
30 -30 -30
All Measurable
0 -50
PR -50
PR PR
Diameters
0 CR CR
-100 CR
0 100 200 0 100 200
-100
Study Day Study Day 0 100 200
Study Day
NR patient experienced tumor reduction in Treatment changed dynamic of all lesions
lesions that did not receive NBTXR3** from progression to regression
*RT activation ; **lesion may have received low-dose radiation due to vicinity to targeted treatment area 42
Source: NBTXR3-1100 - Cut-off date:23Apr2021Possible Immune Response and Delayed Complete Response?
Stage II HNSCC – non Stage IV HNSCC – non
All target lesions sum of diameters
responder (D) responder (G)
All target lesions sum of diameters
50
change from baseline (%)
50
change from baseline (%)
PD PD
20 20
0 0 SD
SD
-30 -30
** -50
-50
PR PR
CR -100 CR
-100
0 100 200 300 400 0 100 200 300
Study Day Study Day
1 NR patient had delayed 1 NR patient had durable
tumor regression 5-6 months deepening of response with
after treatment, then pseudo- unconfirmed CR
progression followed by pCR**
*Patient D: pathological CR (pCR) based on biopsy sample located in the target lesion 43
Source: NBTXR3-1100 - Cut-off date:23Apr2021Sustained Response in Anti-PD-1 Naïve Patients
Complete Response
K, Cohort 1 Partial Response
Stable Disease
F, Cohort 1 Progressive Disease
On-Study Survival
Off-Study Survival
O, Cohort 2
Death
N, Cohort 1
M, Cohort 3
J, Cohort 1
A, Cohort 1
0 3 6 9 12 15 18 21
Months since NBTXR3 Injection
44
Source: NBTXR3-1100 - Cut-off date:23Apr2021
Cohort 1: H&N, Cohort 2: Lung, Cohort 3: LiverSustained Response in Anti-PD-1 Non-Responder Patients
Complete Response
P, Cohort 2
Partial Response
H, Cohort 2 Stable Disease
Progressive Disease
I, Cohort 3 On-Study Survival
Off-Study Survival
E, Cohort 2 Death
L, Cohort 1
B, Cohort 2
C, Cohort 2
G, Cohort 3
D, Cohort 1 *
0 3 6 9 12 15 18 21
Months since NBTXR3 Injection
*Patient D: pCR based on biopsy sample located in the target lesion 45
Source: NBTXR3-1100 - Cut-off date:23Apr2021
Cohort 1: H&N, Cohort 2: Lung, Cohort 3: LiverTransforming Non-Responders into Responders
ILLUSTRATIVE
NR who responded 4 / 8*
NR who experienced
clinically meaningful° 6/8
tumor reduction
NR with reduction in 3 / 4**
non-injected lesions
Naïve patients who 3/5
responded
Months
*Of which 1 pCR based on biopsy sample located in the target lesion (patient D), **Of which 1 subject with reduction in non-target lesions 46
°Clinically meaningful regression defined as > 10% regression in all target lesions from baseline
Source: NBTXR3-1100 - Cut-off date:23Apr2021Conclusions
• NBTXR3 administration by intratumoral injection was feasible and well tolerated in all patients
• AE profile has not differed in type or grade from what is expected with RT or anti-PD-1 agents
• Regardless of prior anti-PD-1 exposure, 10 out of 13 patients evaluable for tumor response on
study had tumor regression
• These data support continued development of NBTXR3/RT in combination with anti-PD-1 across
multiple tumor types regardless of prior IO exposure
• This study suggests that the combination of NBTXR3/RT and anti-PD-1 can yield a sustained
response in both anti-PD-1 naïve patients and patients having progressed on prior anti-PD-1
therapy
• NBTXR3/RT could be a promising next step after anti-PD-1/ICI resistance
• NBTXR3/RT has demonstrated potential to stimulate an immune response and to turn anti-PD-1
non-responders into responders
47
Source: NBTXR3-1100 - Cut-off date:23Apr2021NBTXR3 as potential combo agnostic product, preclinical rational
and future opportunity
James Welsh, MD
Professor, University of Texas,
MD Anderson Cancer Center
48Pre-Clinical Models: NBTXR3 ability to provide
Systemic Responses
Antitumor Immune
Response
RadScopal™ + anti-PD1 +
anti-CTLA4
Abscopal Effect
49Anti-tumor immune response without Cpi - Abscopal effect
CT26
Colon (mouse)
***
*
ImmunoRad 2018 Cumul of 2 independent experiments 50
SITC 2018Anti-tumor immune response (In vivo – Priming)
CT26
Colon (mouse)
ImmunoRad 2017 51Immune checkpoint inhibitors reactivate anti-tumor immune
response
Tumor cells can escape the immune Immuno-therapy strategy is to
system by expressing surface receptors reactivate the immune system by
that act as switch to stop the immune relieving this brake → anti-PD(L)-1
response
PD-1 = programmed cell death 1; PD-L1 = programmed cell death ligand 1
52
Cancer immunotherapy: PD-1 and beyond. www.smartpatients.com/targets/PD-1. Accessed October 12, 2020.
Jordan BR, Med Sciences, 2016Anti-tumor immune response - Abscopal effect
Combination with anti-PD1
Mouse lung cancer anti-PD1 resistant cell line
Cell line: 344SQ-R
Treatment with NBTXR3,
radiation (XRT), and anti-PD1
delays the growth of primary
and secondary tumors,
improves survival rates, and
reduces the number of
spontaneous lung metastases
in 344SQR model.
53
Submitted articleAnti-tumor immune response - Abscopal effect
Combination with anti-PD1
Mouse lung cancer anti-PD1 resistant cell line NanoString on secondary
tumor
Cell line: 344SQ-R
NBTXR3 regulates the expression of
immune-related genes in the secondary
tumors against cancer cells.
54
Submitted articleAnti-tumor immune response - Abscopal effect
Combination with anti-PD1
Mouse lung cancer anti-PD1 resistant cell line NanoString on secondary
tumor
NBTXR3 regulates the
Cell line: 344SQ-R
expression of immune-
related genes in the
secondary tumors against
cancer cells
55
Submitted articleAnti-tumor immune response - Abscopal effect
Combination with anti-PD1
Mouse lung cancer anti-PD1 resistant cell line
Cell line: 344SQ-R
Can we improve
response by avoiding
CD8 exhaustion? Same
experiment performed
with addition of anti-
LAG3+anti-TIGIT
56
Submitted articleAnti-tumor immune response - Abscopal effect
Combination with anti-PD1+anti-TIGIT+anti-LAG3
Mouse lung cancer anti-PD1 resistant cell line
Cell line: 344SQ-R
57
AACR RSM 2021Anti-tumor immune response - Abscopal effect
Combination with anti-PD1+anti-TIGIT+anti-LAG3
Mouse lung cancer anti-PD1 resistant cell line
Cell line: 344SQ-R
Cured mice rechallenge experiment (tumor engraftment):
Combination therapy of NBTXR3+XRT+anti-PD1+anti-LAG3+anti-TIGIT produces a robust long-term anti-tumor immune
response and memory.
58
AACR RSM 2021Anti-tumor immune response - Abscopal effect
Combination with anti-PD1+anti-TIGIT+anti-LAG3
Mouse lung cancer anti-PD1 resistant cell line
Cell line: 344SQ-R
Cured mice rechallenge experiment (flow cytometry analysis):
Combination therapy of NBTXR3+XRT+anti-PD1+anti-LAG3+anti-TIGIT produces a robust long-term anti-tumor immune
response
59
AACR RSM 2021Conclusion
▪ NBTXR3 +RT has an anti-tumor immune response and triggers an abscopal effect
independent of checkpoint inhibitors
▪ Adding NBTXR3 (a radiation enhancer), to the combination of radiotherapy and anti-PD1
significantly improves abscopal effect
▪ The combination therapy of NBTXR3+XRT+anti-PD1+anti-LAG3+anti-TIGIT (Combo) significantly
promotes the proliferation activity of CD8+ T cells, improves tumor control, produces a long-
term anti-tumor immune response and increases survival rate
▪ The anti-tumor efficacy of the NBTXR3+XRT+anti-PD1+anti-LAG3+anti-TIGIT combination is
heavily dependent on CD4+ and CD8+ T cells
▪ The survivor mice from the group treated with the Combo therapy are immune to re-injection of
tumor cells
▪ Combo therapy maintains a significantly higher percentage of memory CD4+ and CD8+ T cells as
well as stronger anti-tumor immune activities than the control. This results in a long-term anti-
tumor immune response
60Discussion and Q&A
Jared Weiss, MD
Tanguy Seiwert, MD
Colette Shen, MD, PhD
James Welsh, MD
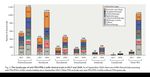
61Outlook of Best % Change from Baseline in HNSCC Trials:
Anti-PD-1 Naïve (Literature Data)
PD-1 Naïve Trials
Feladilimab + Pembro Eftilagimod + Pembro
INDUCE 1 – Anti-PD-1 Naïve TACTI-002 – Anti-PD-1 Naïve
Best Observed Response by RECIST 1.1 as per
Investigator Assessment
By Previous Exposure to Anti-PD-1 Therapy
Anti-PD-1 naïve Anti-PD-1 non-responder
All target lesions sum of diameters
40
PD
change from baseline (%)
20
0
SD
-20 *
-40
-60
PR
-80
T VEC + Pembro
-100 *** CR MASTERKEY-232 – 2L Naïve
Patient:H I M N L D E J C B O A G
*patient D: pCR based on biopsy sample located in the target lesion; **Unconfirmed Response
62
Source: Literature data and NBTXR3-1100 - Cut-off date: 23Apr2021Outlook of Best % Change from Baseline in HNSCC Trials:
Anti-PD-1 Non-Responders (Literature Data)
Anti-PD-1 Non-Responders Trials
Nivolumab Eganelisib + Nivo
Best Observed Response by RECIST 1.1 as per CHECKMATE 141 – Anti-PD-1 NR MARIO 1 – CPI NR
Investigator Assessment
By Previous Exposure to Anti-PD-1 Therapy
Anti-PD-1 naïve Anti-PD-1 non-responder
All target lesions sum of diameters
40
PD
change from baseline (%)
20
0
SD
-20 *
-40
-60
PR
Monalizumab + Cetux Debio + Anti-PD-1
Previous Anti-PD-1 Previous Anti-PD-1
-80
-100
** CR
Patient:H I M N L D E J C B O A *G
*
*patient D: pCR based on biopsy sample located in the target lesion; **Unconfirmed Response
63
Source: Literature data and NBTXR3-1100 - Cut-off date: 23Apr2021Study 1100: Patient Case Studies
64Study 1100:
NBTXR3 +
Checkpoint
Inhibitors
Preliminary
Anti-PD-1 Naïve Patients
Results
@
ASCO
2021
NOTE: Ongoing study /
Data subject to change
NR = non-responder 65
In house data. Date data Censored (October 09 2020)Study 1100 – Cohort 1 (H&N Re-Irradiation)
Baseline%(%)
50
Dose Level 1: 22% PD
Change,
20
0 SD
from
~2 years ongoing survival
Overall
-30
BestChange
-50
PR
Diameters
Initiated treatment in June 2019 at UNC
Patient No. A
Patient is still in follow-up with nearly 2y ongoing survival CR
-100
0 100 200 300 400 500 600 700
Primary
H&N Stage III H&N with LRR in lymph node Study Day
Tumor
Prior
Naïve No prior IO, but patient has had prior CRT
Baseline (%)
Anti-PD-1
%
50
Baseline,
PD-L1 NBTXR3 Injected
Unk PD-L1 expression is unknown
Expression
from
0
Study 1100 Patient has had a durable ~2y confirmed CR that has deepened over time
from
CR
BOR Note lesion injected is lymph node
Change
Change
-50
Diameters
Best
-100 66
Source: NBTXR3-1100 - Cut-off date:23Apr2021Study 1100 – Cohort 1 (H&N Re-Irradiation)
50
Best Overall Change, %
PD
Dose Level 1: 22%
(%)%
20
Change,
50 050
from Baseline
Best Overall Change, %
PD SD NBTXR3 Injected
PD
20 -3020 Non-NBTXR3-Inje
4 months ongoing survival
Lesions
0 SD -50 0 SD
PR
Change
-30 -30
Measurable
Initiated treatment in December 2020 at Chicago -50 -50 CR
Patient No. J -100
Patient is still in follow-up with 4m ongoing survival PR PR
Diameters
0 100
Study Day CR
Primary -100
H&N Stage IV p16– HNSCC with LRR in lymph node
-100 CR
Tumor
All
0 100
0 100
Study Day
(%)%
Prior
Naïve
No prior IO, Study Day
Anti-PD-1 but patient has had prior induction chemo followed by concomitant TFHX 50
Baseline,
NBTXR3 Injected
from Baseline
PD-L1
Non-NBTXR3-Injected
Neg PD-L1 expression is equal to 0% by TPS
Expression 0
Changefrom
Study 1100 Patient had unconfirmed PR (-31%) at 2nd post-treatment scan to date
PR
BOR Note lesion injected and non-injected are both lymph nodes
Best Change
-50
Diameters
-100
67
Source: NBTXR3-1100 - Cut-off date:23Apr2021Study 1100:
NBTXR3 +
Checkpoint
Inhibitors
Preliminary
Anti-PD-1 Non-Responders
Results
@
ASCO
2021
NOTE: Ongoing study /
Data subject to change
NR = non-responder 68
In house data. Date data Censored (October 09 2020)Study 1100 – Cohort 2 (Lung Mets)
%(%)
50
Did Not Receive Full Dose:Study 1100 – Cohort 1 (H&N Re-Irradiation)
All target lesions sum of diameters
50
50
(%)%
Dose Level 1: 22% PD
PD
Change,
20
baseline
20
0 SD
0 SD
Overall
-30
13 months ongoing survival *
-50
-30
from
PR
Best
-50
change
-100 CR PR
Initiated treatment in March 2020 at Moffitt 0 100 200 300 400
Patient No. D Study Day CR
Patient is still in follow-up with 13m ongoing survival -100
0 100 200 300 400
Primary
H&N Stage II p16+ HNSCC with LRR in BOT
Study Day
Tumor *pCR based on biopsy sample located in the target lesion
Prior
1° NR 4 months of nivo in 2019 with a BOR of SD and prior CRT
Anti-PD-1
%
Baseline (%)
50
Baseline,
PD-L1 NBTXR3 Injected
Unk PD-L1 expression is unknown
Expression
0
from
Patient has had varied SD response (-28% to 20% to -24%)
Study 1100
from
CR Technically PD by RECIST, but consistent with pseudoprogression
BOR
Change
Recently iSD then iCR by iRECIST
Change
-50
Diameters
Best
-100 70
Source: NBTXR3-1100 - Cut-off date:23Apr2021Study 1100 – Cohort 2 (Lung Mets)
50
Dose Level 1: 22%
Best Overall Change, %
(non-target lesions)
(%) %
PD
Change,
50 (non-target lesions)
20
50
Best Overall Change, %
PD NB
from Baseline
0 PD
20 20 SD No
14 months ongoing survival
Lesions
0 SD -300
SD No
-30 -50
-30
Change
PR
Measurable
Initiated treatment in January 2020 at UNC -50 -50
Patient No. C PR
Patient withdrew consent due to travel concerns with 14m ongoing survival PR
CR
AllDiameters
-100
CR 0 100 200
Primary
Lung
-100
Stage IV NSCLC with lung mets as well as mets to APW and inguinal lymph nodes -100 CR
Tumor 0 100 200 Study Day
0 100 200
Study Day Study Day
Prior
1° NR 6 months of pembro (single agent and with chemo) in 2019 with a BOR of PD
Anti-PD-1
%
Baseline (%)
50
Baseline,
PD-L1 NBTXR3 Injected
Pos PD-L1 expression is equal to 65%
Expression Non-NBTXR3-Injected
(non-target lesions)
0
from
Patient had confirmed 4m PR (-46%) at injected lesion
Study 1100
from
PR and confirmed CR at non-injected sites (non-target lymph nodes)
BOR
Change
Of note – response was ongoing when patient came off-study
Change
-50
Diameters
Best
-100 71
Source: NBTXR3-1100 - Cut-off date:23Apr2021Study 1100 – Cohort 1 (H&N Re-Irradiation)
50
%
Dose Level 1: 22%
(%) %
PD
Change,
50
Change,
50
20
Best Overall Change, %
PD NBTXR3 Inj
from Baseline
PD
20 0 SD
4 months ongoing survival 20 Non-NBTXR
Lesions
0
Overall
SD -300
SD Non-NBTXR
-30 -50
Change
-30 PR
DiametersBest
All Measurable
-50
Initiated treatment in December 2020 at Hopkins -50
Patient No. L
Patient is still in follow-up with 4m ongoing survival PR CRPR
-100
0 100
Primary CR
H&N Stage IV p16+ HNSCC with LRR in lymph node
-100 Study Day CR
Tumor -100
0 100 0 100
Prior Study Day Study Day
1° NR 3 months of pembro in 2020 with a BOR of PD and prior CRT
Anti-PD-1
%
Baseline (%)
50
Baseline,
PD-L1 NBTXR3 Injected
Neg PD-L1 expression isStudy 1100 – Cohort 3 (Liver Mets)
% (%)
50
Dose Level 1: 22%
Baseline
PD
Change,
20
0
Change from
SD
10 months ongoing survival
Best Overall
-30
-50
PR
Diameters
Initiated treatment in June 2020 at UNC
Patient No. G
Patient is still in follow-up with 10m ongoing survival CR
-100
0 100 200 300
Primary
H&N Stage IV p16+ HNSCC with liver mets Study Day
Tumor
1 year of pembro from May 2019 to May 2020 with a BOR of 1m CR
Prior
2° NR followed by PD
Anti-PD-1
%
Baseline (%)
Also had prior EXTREME chemo
50
Baseline,
NBTXR3 Injected
PD-L1
Pos PD-L1 expression is equal to 50%
Expression
0
from
from
Study 1100 Patient has had a durable 8m response (PR then unconfirmed CR)
CR
Change
BOR Note response has deepened over time (-41% to -100%)
Change
-50
Diameters
Best
-100 73
Source: NBTXR3-1100 - Cut-off date:23Apr2021Study 1100 – Cohort 3 (Liver Mets)
50
Dose Level 1: 22%
Best Overall Change, %
PD
%
20
Change, (%)
50
0 50
from Baseline
Best Overall Change, %
PD SDPD NBTXR3 Injecte
9 months ongoing survival 20
-30 20 Non-NBTXR3-In
Lesions
0 SD -50 0 SD Non-NBTXR3-In
PR
Diameters Change
-30
Initiated treatment in August 2020 at Banner -30
Patient No. I
Measurable
Patient came off study for PD, but is still alive with 9m -50
ongoing survival -50 CR
PR -100
PR
0 100
Primary
Lung Stage IV NSCLC with lung and liver mets CR Study Day
Tumor -100 CR
-100
0 100
All
0 100
Prior
1° NR 3 months of pembro with chemo in 2020 with a BOR of SD thenStudy
PD Day Study Day
Anti-PD-1
%
Baseline (%)
50
fromBaseline,
PD-L1 NBTXR3 Injected
Neg PD-L1 expression isStudy 1100 – Cohort 2 (Lung Mets)
% (%)
50
Dose Level 1: 22%
Baseline
PD
Change,
20
0
Change from
SD
Best Overall
-30
-50
PR
Diameters
Initiated treatment in May 2020 at Moffitt
Patient No. E
Patient passed away 3m after study start due to disease progression CR
-100
0 100
Primary
H&N Stage IV p16– HNSCC with lung mets Study Day
Tumor
Prior
1° NR 2,3 months of pembro in 2020 with a BOR of PD and prior CRT
Anti-PD-1
%
Baseline (%)
50
Baseline,
PD-L1 NBTXR3 Injected
Unk PD-L1 expression is unknown
Expression
0
from
Study 1100
from
SD Patient had unconfirmed SD (-29%) at only post-treatment scan
BOR
ChangeChange
-50
Diameters
Best
-100 75
Source: NBTXR3-1100 - Cut-off date:23Apr2021Study 1100 – Cohort 2 (Lung Mets)
% (%)
50
Dose Level 1: 22%
Baseline
PD
Change,
20
0
Change from
SD
10 months ongoing survival
Best Overall
-30
-50
PR
Diameters
Initiated treatment in July 2020 at Banner
Patient No. H
Patient came off study for PD, but is still alive with 10m ongoing survival CR
-100
0 100
Primary Stage IV NSCLC with lung mets in lymph nodes and left pericardium
Lung Study Day
Tumor as well as bone mets
Prior
1° NR 3,7 months of pembro in 2020 with a BOR of SD then PD
Anti-PD-1
%
Baseline (%)
50
fromBaseline,
PD-L1 NBTXR3 Injected
Neg PD-L1 expression isYou can also read