Reducing Disparities Using Telehealth Approaches for Postdelivery Preeclampsia Care
←
→
Page content transcription
If your browser does not render page correctly, please read the page content below
CLINICAL OBSTETRICS AND GYNECOLOGY
Volume 64, Number 2, 375–383
Copyright © 2021 Wolters Kluwer Health, Inc. All rights reserved.
Reducing Disparities
Using Telehealth
Approaches for
Postdelivery
Preeclampsia Care
ADINA KERN-GOLDBERGER, MD, MPH, and
ADI HIRSHBERG, MD
Department of Obstetrics & Gynecology, Maternal Child Health
Research Center, University of Pennsylvania Perelman School of
Medicine, Philadelphia, Pennsylvania
Abstract: The management of hypertensive disease Key words: telehealth, telemedicine, mobile health, pre-
of pregnancy presents an ongoing challenge after eclampsia, pregnancy-related hypertension, postpartum,
patients are discharged from delivery hospitaliza- fourth trimester, maternal morbidity, racial disparity
tions. Preeclampsia and other forms of postpartum
hypertension increase the risk for severe maternal
morbidity and mortality in the postpartum period,
and both hypertension and its associated adverse
events disproportionately affect black women. With
its ability to transcend barriers to health care access,
Racial Disparities in
telemedicine can facilitate high-quality postpartum Postpartum Preeclampsia
care delivery for preeclampsia management and
thereby reduce racial disparities in obstetric care
and outcomes. Here we discuss racial disparities in MATERNAL MORBIDITY IN THE
preeclampsia and the challenge of providing equi- FOURTH TRIMESTER
table postpartum preeclampsia care. We then de- Obstetric care during the postpartum period
scribe the utility of novel telemedicine platforms —also coined the “fourth trimester”—re-
and their application to combat these disparities in mains as essential as during the 3 trimesters
preeclampsia care.
of pregnancy. Many pregnancy complica-
tions, including preeclampsia, hemorrhage,
infection, and perinatal depression, can arise
Correspondence: Adi Hirshberg, MD, Hospital of the specifically in the postpartum setting. Crit-
University of Pennsylvania, 2nd Floor Silverstein Bldg,
Philadelphia, PA. E-mail: adi.hirshberg@pennmedicine. ical postpartum decisions, such as those
upenn.edu involving contraception and breastfeeding,
The authors declare that they have nothing to disclose. can have meaningful lifelong repercussions.
CLINICAL OBSTETRICS AND GYNECOLOGY / VOLUME 64 / NUMBER 2 / JUNE 2021
www.clinicalobgyn.com | 375
Copyright r 2021 Wolters Kluwer Health, Inc. All rights reserved.376 Kern-Goldberger and Hirshberg
As such, pregnancy research and obstetric postpartum clinic appointments.2 Fur-
professional organizations have centralized thermore, these challenges are particu-
the postpartum period as an opportunity to larly acute for women without childcare
optimize both short-term and long-term assistance or who are struggling with
maternal health. Comprehensive postpar- social or economic instability.3
tum care should involve chronic disease Understanding both the importance and
management and routine health mainte- the unique challenges of postpartum care is
nance, and surveillance and treatment of critical as trends in maternal morbidity
pregnancy-specific diseases, all of which continue to rise with a concomitant in-
have significant longitudinal implications crease in postpartum complications and
for a woman’s health.1 hospital readmissions. Research has dem-
Many obstetric complications have se- onstrated increased postpartum readmis-
quelae of lifelong disease states—for ex- sion rates from 1.72% in 2004 to 2.16% in
ample, preeclampsia and gestational 2011. These adverse events, many of which
diabetes are associated with chronic hyper- are related to preeclampsia, disproportion-
tension, cardiovascular disease, and type 2 ately affect publicly insured and black
diabetes mellitus—and timely screening women, and women with baseline comor-
and risk assessment in the postpartum bidities such as hypertension and diabetes.4
period could be advantageous for ultimate Efforts to reduce maternal morbidity are
risk reduction. The postpartum care set- therefore evolving to specifically address
ting is also a unique opportunity to opti- gaps in postpartum care with attention to
mize preventive health with vaccination the risk factors and etiologies of postpar-
and Pap smears, and to facilitate family tum complications and the patient groups
planning and pregnancy spacing. All of at highest risk.
this has ramifications for a woman’s gen-
eral health and the health of any future POSTPARTUM PREECLAMPSIA
pregnancies. Ultimately, assiduous post- Chronic hypertension and pregnancy-re-
partum care truly lays the foundation for a lated hypertension remain significant con-
woman’s healthy future. tributors to the overall burden of maternal
However, traditional postpartum care, morbidity, and this persists in the post-
which at a minimum involves an in- partum period as well. Postpartum onset
person visit 4 to 6 weeks after delivery, preeclampsia, defined as a new diagnosis
involves inherent barriers to accessing of preeclampsia between 2 days and 6
necessary health services. Most postpar- weeks postpartum, occurs most commonly
tum patients have new infants at home in women with the same risk profile as
requiring abundant care and attention, antepartum preeclampsia, including those
and this may limit their ability to attend with chronic hypertension, obesity, and
follow-up appointments or engage in advanced maternal age.5 As these risk
other health promotion activities. Post- factors increase, preeclampsia incidence
partum women may also be exhausted —both antepartum and postpartum—can
from the physical strain of labor and be expected to increase in parallel.
delivery and the erratic infant sleep sched- Hypertension manifesting in the post-
ule, and they may be recovering from partum period may be a continuation of
painful perineal trauma or cesarean sec- gestational hypertension or preeclampsia,
tion. This may further limit their ability to worsening or persistent chronic hyper-
participate in health care programs. For tension, or new postpartum preeclampsia.
these reasons, compliance with traditional However, the majority of patients read-
postpartum care is generally poor with mitted with postpartum hypertension
very low documented show rates for are experiencing progression of already
www.clinicalobgyn.com
Copyright r 2021 Wolters Kluwer Health, Inc. All rights reserved.Reducing Disparities Using Telehealth for Preeclampsia Care 377
diagnosed hypertensive disease rather hypertensive disorders, this should involve
than new onset preeclampsia in the post- blood pressure monitoring during the first
partum period, and are typically asymp- 72 hours postpartum followed by an addi-
tomatic, necessitating careful blood tional blood pressure assessment at 7 to
pressure monitoring even after hospital 10 days postpartum because of the in-
discharge.6 creased risk of preeclampsia complications
Hypertension is one of the most common in this time period, including strokes and
etiologies of postpartum readmission, and seizures.11 Effective management of pree-
women with pregnancy-associated hyperten- clampsia in the postpartum setting is ren-
sion are at the highest risk.7 Reducing dered ever more crucial by the association
hospital readmission is a quality improve- between preeclampsia and long-term car-
ment imperative for all health care institu- diovascular disease.
tions and is especially important in
obstetrics, where maternal readmission to RACIAL DISPARITIES IN
the hospital disrupts the care of a newborn PREECLAMPSIA
infant. As pregnancy-related hospital admis- Significant racial disparities across many
sion is the most frequently coded admission obstetric outcomes—including severe mor-
diagnosis in the United States, understand- bidity and mortality—have been demon-
ing patterns of readmission in order to strated between black and white women,
improve health care utilization and quality many which cannot be attributed to base-
has significant public health ramifications.8 line differences in socioeconomic status or
In addition, studies of postpartum readmis- underlying comorbidities. Differential ac-
sions have demonstrated disparities in dem- cess to care and implicit bias in the medical
ographics, with readmitted patients more establishment have been posited as possible
likely to be black, publicly insured, and have mechanisms, and many institutions and
a lower income, and higher rates of organizations have prioritized efforts to
comorbidities.9 Efforts to reduce postpartum alleviate these disparities.12 Black women
complications and hospital readmission are are specifically at higher risk of preeclamp-
therefore essential endeavors to promote sia and preeclampsia-related complications,
women’s health in general and the health and longitudinal cardiovascular disease,
and well-being of the most vulnerable which is a known downstream complica-
groups of postpartum patients in particular. tion of preeclampsia.13 They are also at
It is also critical that these strategies higher risk of preeclampsia-related hospital
specifically target risk-reduction for post- readmission.14 Although prediction and
partum hypertension complications. In prevention strategies for preeclampsia itself
fact, ~50% of maternal morbidity and are limited, the disease burden of short-
mortality takes place postpartum, one third term preeclampsia complications including
of which occurs within the first week.10 stroke and acute renal failure, and long-
This correlates with the time course of peak term complications such as cardiac disease
blood pressures, which typically occur in may be attenuated with appropriate clinical
the initial 3 to 6 days postpartum, usually care. For example, timely administration of
after patients have already been discharged antihypertensive medication is associated
from the hospital. Given the association of with a reduction in maternal stroke.15
adverse postpartum outcomes with hyper- Numerous studies have highlighted a
tensive disease, the American College of racial disparity in the disease burden of
Obstetricians and Gynecologists (ACOG) preeclampsia. Gyamfi-Bannerman et al16
recommends careful blood pressure surveil- demonstrated that among women with
lance in the postpartum setting. At a preeclampsia, non-Hispanic Black wom-
minimum, for women with known en were more likely to experience severe
www.clinicalobgyn.com
Copyright r 2021 Wolters Kluwer Health, Inc. All rights reserved.378 Kern-Goldberger and Hirshberg maternal morbidity and mortality than a postpartum follow-up appointment with non-Hispanic White women. Miller a women’s health provider and
Reducing Disparities Using Telehealth for Preeclampsia Care 379
the purpose of reporting results, manag- Telemedicine platforms designed for
ing medications, and confirming medical specific aspects of postpartum care have
appointments, among other uses. Current also been developed and found to be
iterations of mobile phones are also re- effective. Research from other developed
plete with direct-to-consumer health- countries has demonstrated patient and
relates applications (apps), an industry provider satisfaction with telephone
that is rapidly proliferating. The past and video conference-based consultations
decade has seen robust development in in the postpartum period to facilitate
the market of mobile applications for early hospital discharge and to support
women’s health and pregnancy, repre- new mothers in the home setting.25 It is
senting 7% of total “apps” in 2015.22 possible that routine postpartum care can
These phenomena have recast the mobile be comprehensively retooled into teleme-
telephone as an ideal tool for health care dicine platforms to increase access given
delivery. The vast majority of US adults, historically poor rates of postpartum fol-
especially those of reproductive age, own low-up in traditional settings.
a cellular phone, and use those for text
messaging. This pervasiveness enables HEALTH DISPARITIES AND
text message-based care delivery models TELEMEDICINE
to be convenient, economical, and patient- It is well-known that obstetric morbidity
centered. disproportionately affects women with
difficult access to care, including women
TELEMEDICINE IN OBSTETRICS from minority racial and ethnic back-
The utilization of telehealth and teleme- grounds and low socioeconomic status.
dicine in obstetrics is becoming increas- Telemedicine possesses a unique ability to
ingly widespread, improving access to transmit high-level care directly to pa-
care and providing health information tients in their own environments, circum-
for many women. Numerous such pro- venting the barriers and biases that can
grams have been implemented with suc- otherwise inhibit quality care. For exam-
cess across the country. For example, the ple, a study of the ANGELS obstetric
“OB Nest” program at the Mayo Clinic is telemedicine program in Arkansas found
a model of care for low-risk pregnant a significant decrease in the rate of very
women involving self-monitoring tools, low birth weight infants of patients with
a texting platform, and an online com- Medicaid insurance who delivered in hos-
munity of other pregnant patients to share pitals without an appropriate neonatal
experiences.23 Patients were provided intensive care unit.26 Telemedicine can
with self-monitoring equipment and re- similarly serve as a powerful tool to
ported that obtaining their own measure- alleviate other disparities in access to care
ments without the inconvenience of for vulnerable populations.
presenting to the clinic fostered increased
confidence and a sense of control during TELEMEDICINE IN THE
the pregnancy. The novel coronavirus MANAGEMENT OF POSTPARTUM
(COVID-19) pandemic has accelerated PREECLAMPSIA
the adoption of telemedicine-based ob- Numerous mobile phone telemedicine
stetric care to reduce the risk of exposure programs have been developed specifi-
to the virus and facilitate social distanc- cally around the postpartum management
ing. These programs have seen a rapid of hypertensive disorders of pregnancy.
uptake in hospital systems throughout the These have evolved to meet the need of
country with models for routine and high- the many postpartum women requiring
risk antenatal care.24 continued blood pressure monitoring
www.clinicalobgyn.com
Copyright r 2021 Wolters Kluwer Health, Inc. All rights reserved.380 Kern-Goldberger and Hirshberg
after discharge from the hospital, to blood pressure check in the clinic during
reduce morbidity related to underman- the first week postpartum) versus Heart
aged postpartum preeclampsia, and to Safe Motherhood, a 2-week test message-
prevent hospital readmissions. They also based surveillance program (see example
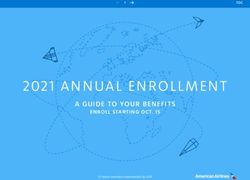
specifically address the problem of incon- in Fig. 1), and found a significantly higher
sistent postpartum outpatient follow-up, rate of follow-up, defined as having a
which can be critical and time-sensitive in recorded blood pressure in the medical
the setting of hypertensive disorders of record within the first 10 days postpartum.
pregnancy. As dangerous blood pressure
elevations are often asymptomatic, com- REDUCING DISPARITIES IN
pliance with ACOG’s recommended sur- POSTPARTUM PREECLAMPSIA WITH
veillance is essential. And as hospital TELEMEDICINE
readmission is extremely disruptive to As discussed above, Heart Safe Mother-
the mother-baby unit in the postpartum hood is the postpartum text message-based
period, an innovative approach to in-
creasing access to blood pressure surveil-
lance and management for this patient
population is essential.
Numerous studies have examined the
feasibility, acceptability, and clinical out-
comes of remote blood pressure monitor-
ing programs for postpartum women.
Hauspurg et al27 evaluated a quality im-
provement project designed for women
admitted to the postpartum unit of the
University of Pittsburg Medical Center
(UPMC Magee-Women’s Hospital) with
a diagnosis of pregnancy-specific or
chronic hypertension and involving a text
messaged-based blood pressure monitor-
ing program. The study found high rates of
patient engagement, retention, and satis-
faction with the program, and 88% com-
pliance with the recommended 6-week
postpartum office visit. The Blood Pres-
sure Self-Monitoring in Pregnancy obser-
vational study in the United Kingdom
collected qualitative data suggesting that
self-monitoring of blood pressure in preg-
nancy is acceptable and feasible for wom-
en and that participating in a remote
monitoring program increased awareness
of the risks of preeclampsia.28 It also
promoted patient empowerment and in-
creased reassurance. Hirshberg et al29 at
the Hospital of the University of Pennsyl-
vania (HUP) randomized 206 postpartum
patients with pregnancy-related hyperten- FIGURE 1. Example of patient text message
interface for Heart Safe Motherhood.
sion to routine care (involving an in-person
www.clinicalobgyn.com
Copyright r 2021 Wolters Kluwer Health, Inc. All rights reserved.Reducing Disparities Using Telehealth for Preeclampsia Care 381
FIGURE 2. Postpartum blood pressure attainment by race. Adapted from Hirshberg et al.29
Adaptations are themselves works protected by copyright. So in order to publish this adaptation,
authorization must be obtained both from the owner of the copyright in the original work and
from the owner of copyright in the translation or adaptation.
blood pressure surveillance program for non-Black and Black women was > 90%
women with hypertension in pregnancy at (Fig. 2). This represents a 50% reduction in
the HUP. Implementation of this program racial disparity (risk ratio 0.51, 95% con-
improved blood pressure control, reduced fidence interval, 0.33-0.78). No women in
readmissions, and improved patient and the telemedicine arm required hospital
provider satisfaction.30 Institutional data readmission compared with 4 in the con-
from HUP demonstrated that non-Black trol arm, 3 of whom were black.
women are twice as likely to return for an These data demonstrate that the use of a
in-person blood pressure check shortly text message-based monitoring system re-
after discharge compared with black wom- sulted in significantly higher compliance
en (42.5% vs 24.1% attendance rate, re- among all women with no differences in
spectively).30 To test the impact of a blood pressure capture by race as was
telemedicine-based follow-up program on observed with usual care. When imple-
postpartum blood pressure management, mented at another institution within the
women were randomized in a controlled same health system, blood pressure ascer-
trial to either 2 weeks of twice daily text tainment among Black and non-Black
message-based blood pressure surveillance women was again similar through use of
with home monitoring (Heart Safe Moth- the program, suggesting that reduction of
erhood) or traditional care with an in- racial disparities may be generalizable with
person office visit for blood pressure the implementation of similar remote
monitoring 4 to 6 days after discharge. monitoring interventions.31
Of 206 women in the trial, non-Black Given the slower decline in blood pres-
women in the traditional management arm sure among black women with hypertensive
had 70% compliance with care, compared disorders of pregnancy compared with non-
with 33% of Black women. In the tele- Black women, opportunities to reduce
medicine group, however, the rate of blood disparities in postpartum care have the
pressure measurement attainment in both potential to improve both short-term and
www.clinicalobgyn.com
Copyright r 2021 Wolters Kluwer Health, Inc. All rights reserved.382 Kern-Goldberger and Hirshberg
long-term morbidity related to preecla- 2. Wilcox A, Levi EE, Garrett JM. Predictors of
mpsia.19 Altogether, this suggests that tele- non-attendance to the postpartum follow-up visit.
medicine affords an innovative and success- Matern Child Health J. 2016;20(suppl 1):22–27.
3. Qafiti F, Kaur S, Bahado-Singh R. Development
ful platform to improve access to preecla- of a clinical risk assessment tool for 6-week
mpsia management in the critical postpar- postpartum visit nonadherence. Am J Perinatol.
tum window, during which time women 2018;35:688–694.
from minority groups face increased barriers 4. Clapp MA, Little SE, Zheng J, et al. A multi-
to accessing traditional care. It is critical, state analysis of postpartum readmissions in the
United States. Am J Obstet Gynecol. 2016;215:113
however, that implementation of telemedi- e111–113 e110.
cine avoid inadvertently widening racial 5. Redman EK, Hauspurg A, Hubel CA, et al.
disparities and that simple, affordable, and Clinical course, associated factors, and blood
accessible technology is prioritized. pressure profile of delayed-onset postpartum pre-
eclampsia. Obstet Gynecol. 2019;134:995–1001.
6. Hirshberg A, Levine LD, Srinivas SK. Clinical
factors associated with readmission for postpar-
Conclusions tum hypertension in women with pregnancy-
The immediate postpartum period— related hypertension: a nested case control study.
though fleeting—has many short-term J Perinatol. 2016;36:405–409.
and long-term implications for a woman’s 7. Belfort MA, Clark SL, Saade GR, et al. Hospital
readmission after delivery: evidence for an in-
health. It is a challenging time to access creased incidence of nonurogenital infection in
traditional care given the responsibilities the immediate postpartum period. Am J Obstet
of caring for a newborn, in addition to all Gynecol. 2010;202:35 e31–e37.
of the usual barriers to care that unduly 8. Agency for Healthcare Research and Quality
affect Black women. For women with HCUP fast stats. Healthcare Cost and Utilization
Project (HCUP); 2020. Agency for Healthcare
hypertensive disorders of pregnancy, the Research and Quality, Rockville, MD. Available
events that transpire in the first several at: www.hcup-us.ahrq.gov/faststats/national/inpatie
weeks postpartum can result in hospital ntcommondiagnoses.jsp; www.hcup-us.ahrq.gov/
readmission, severe morbidity including faststats/NationalDiagnosesServlet. Accessed August
stroke, and significant downstream car- 1, 2020.
diovascular disease. Leveraging the capa- 9. Aziz A, Gyamfi-Bannerman C, Siddiq Z, et al.
Maternal outcomes by race during postpartum
bilities of telecommunication technology readmissions. Am J Obstet Gynecol. 2019;220:484
to expand access to care for postpartum e481–484 e410.
preeclampsia has the potential to reduce 10. Creanga AA, Syverson C, Seed K, et al. Preg-
maternal morbidity and mortality, de- nancy-related mortality in the United States,
crease readmissions, improve the patient 2011-2013. Obstet Gynecol. 2017;130:366–373.
11. American College of Obstetricians, Gynecolo-
experience, and chip away at the racial gists, Task Force on Hypertension in Pregnancy.
disparities institutionalized by the health Hypertension in pregnancy. Report of the Amer-
care system. Continued investment in ican College of Obstetricians and Gynecologists’
growing, refining, and evaluating teleme- Task Force on Hypertension in Pregnancy. Obstet
dicine programs for postpartum hyper- Gynecol. 2013;122:1122–1131.
12. Jain J, Moroz L. Strategies to reduce disparities in
tension, with specific attention to their maternal morbidity and mortality: patient and pro-
ability to provide equitable care, is an vider education. Semin Perinatol. 2017;41:323–328.
important step to promote obstetric and 13. Shahul S, Tung A, Minhaj M, et al. Racial disparities
cardiovascular health for all women. in comorbidities, complications, and maternal and
fetal outcomes in women with preeclampsia/eclamp-
sia. Hypertens Pregnancy. 2015;34:506–515.
14. Wagner JL, White RS, Tangel V, et al. Socio-
References economic, racial, and ethnic disparities in postpar-
1. ACOG Committee. Opinion No. 736: optimizing tum readmissions in patients with preeclampsia: a
postpartum care. Obstet Gynecol. 2018;131: multi-state analysis, 2007-2014. J Racial Ethn
e140–e150. Health Disparities. 2019;6:806–820.
www.clinicalobgyn.com
Copyright r 2021 Wolters Kluwer Health, Inc. All rights reserved.Reducing Disparities Using Telehealth for Preeclampsia Care 383
15. Too G, Wen T, Boehme AK, et al. Timing and 24. Spiegelman JKN, Syeda S, Sutton D, et al. Rapid
risk factors of postpartum stroke. Obstet Gynecol. development and implementation of a Covid-19
2018;131:70–78. telehealth clinic for obstetric patients. NEJM
16. Gyamfi-Bannerman C, Pandita A, Miller EC, Catalyst 2020.
et al. Preeclampsia outcomes at delivery and race. 25. Lindberg ICK, Ohrling K. Parents’ experiences of
J Matern Fetal Neonatal Med. 2019;33:3619–3626. using videoconferencing as a support in early dis-
17. Miller EC, Zambrano Espinoza MD, Huang Y, charge after childbirth. Midwifery. 2009;25:357–365.
et al. Maternal race/ethnicity, hypertension, and 26. Kim EW, Teague-Ross TJ, Greenfield WW, et al.
risk for stroke during delivery admission. J Am Telemedicine collaboration improves perinatal
Heart Assoc. 2020;9:e014775. regionalization and lowers statewide infant mor-
18. Hauspurg A, Lemon L, Cabrera C, et al. Racial tality. J Perinatol. 2013;33:725–730.
differences in postpartum blood pressure trajecto- 27. Hauspurg A, Lemon LS, Quinn BA, et al. A
ries among women after a hypertensive disorder of postpartum remote hypertension monitoring pro-
pregnancy. JAMA Netw Open. 2020;3:e2030815. tocol implemented at the hospital level. Obstet
19. Lopes Perdigao J, Hirshberg A, Koelper N, et al. Gynecol. 2019;134:685–691.
Postpartum blood pressure trends are impacted 28. Hinton L, Tucker KL, Greenfield SM, et al.
by race and BMI. Pregnancy Hypertens. 2020;20: Blood pressure self-monitoring in pregnancy
14–18. (BuMP) feasibility study; a qualitative analysis
20. Chornock R, Iqbal SN, Kawakita T. Racial dispar- of women’s experiences of self-monitoring. BMC
ity in postpartum readmission due to hypertension Pregnancy Childbirth. 2017;17:427.
among women with pregnancy-associated hyperten- 29. Hirshberg A, Downes K, Srinivas S. Comparing
sion. Am J Perinatol. 2020. [Epub ahead of print]. standard office-based follow-up with text-based
21. Lewey J, Levine LD, Yang L, et al. Patterns of remote monitoring in the management of post-
postpartum ambulatory care follow-up care partum hypertension: a randomised clinical trial.
among women with hypertensive disorders of BMJ Qual Saf. 2018;27:871–877.
pregnancy. J Am Heart Assoc. 2020;9:e016357. 30. Hirshberg A, Sammel MD, Srinivas SK. Text
22. IMS Institute for Healthcare Informatics. Patient message remote monitoring reduced racial
adoption of mHealth: use, evidence and remain- disparities in postpartum blood pressure ascer-
ing barriers to mainstream acceptance; 2015. tainment. Am J Obstet Gynecol. 2019;221:
Available at: https://www.iqvia.com/-/media/iqvia/ 283–285.
pdfs/institute-reports/patient-adoption-of-mhealth. 31. Triebwasser JE, Janssen MK, Hirshberg A, et al.
pdf. Accessed August 1, 2020. Successful implementation of text-based
23. de Mooij MJM, Hodny RL, O’Neil DA, et al. OB blood pressure monitoring for postpartum
nest: reimagining low-risk prenatal care. Mayo hypertension. Pregnancy Hypertens. 2020;22:
Clin Proc. 2018;93:458–466. 156–159.
www.clinicalobgyn.com
Copyright r 2021 Wolters Kluwer Health, Inc. All rights reserved.You can also read