Child Life Services - American Academy of Pediatrics
←
→
Page content transcription
If your browser does not render page correctly, please read the page content below
POLICY STATEMENT Organizational Principles to Guide and Define the Child Health
Care System and/or Improve the Health of all Children
Child Life Services
Barbara Romito, MA, CCLS,a Jennifer Jewell, MD, FAAP,b Meredith Jackson, MD, FAAP,b AAP COMMITTEE ON HOSPITAL CARE;
ASSOCIATION OF CHILD LIFE PROFESSIONALS
Child life programs are an important component of pediatric hospital-based abstract
care; they address the psychosocial concerns that accompany hospitalization
and other health care experiences. Child life specialists focus on the optimal a
Child Life Program, The Bristol-Myers Squibb Children’s Hospital at
development and well-being of infants, children, adolescents, and young adults Robert Wood Johnson University Hospital, New Brunswick, New Jersey;
and bThe Barbara Bush Children’s Hospital at Maine Medical Center,
while promoting coping skills and minimizing the adverse effects of Portland, Maine
hospitalization, health care encounters, and/or other potentially stressful
Ms Romito provided the benchmarking data and the majority of the
experiences. In collaboration with the entire health care team and family, child writing; Dr Jewell designed the outline for the policy, noted and
life specialists provide interventions that include therapeutic play, expressive updated information that was irrelevant since the last revision,
provided assistance with the writing, and presented the content to the
modalities, and psychological preparation to facilitate coping and Committee on Hospital Care; Dr Jackson provided technical assistance,
draft review, and content expertise for the portions related to medical
normalization at times and under circumstances that might otherwise prove education; and all authors approved the final manuscript as
overwhelming for the child. Play and developmentally appropriate submitted.
communication are used to (1) promote optimal development, (2) educate Policy statements from the American Academy of Pediatrics benefit
from expertise and resources of liaisons and internal (AAP) and
children and families about health conditions, (3) prepare children and external reviewers. However, policy statements from the American
partner with families for medical events or procedures, (4) plan and rehearse Academy of Pediatrics may not reflect the views of the liaisons or the
organizations or government agencies that they represent.
useful coping and pain-management strategies with patients and families, (5)
The guidance in this statement does not indicate an exclusive course
help children work through feelings about past or impending experiences, and of treatment or serve as a standard of medical care. Variations, taking
(6) partner with families to establish therapeutic relationships between into account individual circumstances, may be appropriate.
patients, siblings, and caregivers. Child life specialists collaborate with the All policy statements from the American Academy of Pediatrics
automatically expire 5 years after publication unless reaffirmed,
entire interdisciplinary team to promote coping and enhance the overall revised, or retired at or before that time.
health care experience for patients and families.
DOI: https://doi.org/10.1542/peds.2020-040261
Address correspondence to Barbara Romito, MA, CCLS.
E-mail: Barbara.Romito@rwjbh.org
CHILD LIFE INTERVENTIONS: PSYCHOLOGICAL PREPARATION PEDIATRICS (ISSN Numbers: Print, 0031-4005; Online, 1098-4275).
This document is copyrighted and is property of the American
Preparing children for hospitalization, clinic visits, surgeries, and Academy of Pediatrics and its Board of Directors. All authors have filed
diagnostic and/or therapeutic procedures is essential during a child’s conflict of interest statements with the American Academy of
Pediatrics. Any conflicts have been resolved through a process
hospitalization and an important element of a child life program. It is approved by the Board of Directors. The American Academy of
estimated that 50% to 75% of children develop significant fear and Pediatrics has neither solicited nor accepted any commercial
involvement in the development of the content of this publication.
anxiety before surgery; recognized risk factors include age, temperament,
baseline anxiety, past medical encounters, and caregiver anxiety.1 FINANCIAL DISCLOSURE: The authors have indicated they have no
financial relationships relevant to this article to disclose.
Children’s anxiety in the perioperative environment is associated with
impaired postoperative behavioral and clinical recovery, including
increased analgesic requirements and delayed discharge from the To cite: Romito B, Jewell J, Jackson M, AAP COMMITTEE ON
recovery room.2,3 Preparation can reduce anxiety and distress before HOSPITAL CARE; ASSOCIATION OF CHILD LIFE PROFESSIONALS.
Child Life Services. Pediatrics. 2021;147(1):e2020040261
surgery and/or during mask induction and may also decrease emergence
Downloaded from www.aappublications.org/news by guest on September 22, 2021
PEDIATRICS Volume 147, number 1, January 2021:e2020040261 FROM THE AMERICAN ACADEMY OF PEDIATRICSdelirium after surgery.4–7 More than stay, a clearer understanding of Child life specialists can effectively
50 years of research and experience procedures, and a more positive provide developmentally appropriate
supports 3 key elements of the physical recovery as well as nonpharmacologic pain management
preparation process: (1) the provision posthospital adjustment for children and provide coaching and support to
of developmentally appropriate enrolled.16 Patients spent less time on patients and caregivers before,
information, (2) the encouragement narcotics, the length of stay was during, and after medical
of questions and emotional slightly reduced, and caregivers were procedures.40,41 They can also
expression, and (3) the formation of more satisfied. In other studies, provide valuable education and
a trusting relationship with a health researchers have found that child life training to nurses, physicians,
care professional.3 A recent interventions play a major role in students, and other personnel,
systematic review of preparation calming children’s fears and result in supporting health care team member
effectiveness evidence concluded that higher parent satisfaction ratings of competencies in the provision of
children who were psychologically the entire care experience.8,17,18 developmentally appropriate,
prepared for surgery experienced psychosocially sound care.42,43
fewer negative symptoms than did Multifaceted institution-wide
children who did not receive formal CHILD LIFE INTERVENTIONS: protocols, such as the Ouchless Place
preparation.3 Findings included PAIN-MANAGEMENT AND COPING and other similar programs,
a decrease in posttraumatic stress, STRATEGIES incorporate the standard use of both
lower levels of fear and anxiety, When combined with preparation and pharmacologic and
increased cooperative behaviors, and appropriate pharmacologic nonpharmacologic techniques,
better long-term coping and interventions, nonpharmacologic preparation of the patient and family,
adjustment to future medical pain- and distress-management environmental considerations, and
challenges. Research also strategies have proven successful in training of all health care team
demonstrates that preparation and terms of patient and family members.44,45
coping facilitation interventions experience, staff experience, and cost- Research has demonstrated that
decrease the need for sedation in effectiveness.17,19,20 Strategies such children are less fearful and
procedures such as MRI and as swaddling, oral sucrose, vibratory distressed when positioned for
radiotherapy, resulting in lower risks stimulation, breathing techniques, medical procedures in a sitting
for the child and cost savings in relaxation, and guided imagery have position rather than supine.46 Child
personnel, anesthesia, and been shown to decrease behavioral life specialists are often involved in
throughput-related expenses.8–12 distress and pain experience in facilitating the use of “comfort holds,”
Preparation techniques, materials, children during invasive medical techniques for positioning children in
and language must be adapted to the procedures.21–25 a parent or caregiver’s lap or other
developmental level, personality, and comforting position. In addition to
Distraction strategies have been reducing the child’s distress and
unique experiences of each child and
highly effective in reducing reported gaining cooperation, these techniques
family. Learning is enhanced with
and observed pain and distress in generally require fewer staff to be
hands-on methods versus exclusively
children in inpatient, emergency present in the room, facilitate safe
verbal explanations. Photographs,
department (ED), and clinic and effective accomplishment of the
diagrams, tours of surgical or
settings.26–32 The emergence of medical procedure, decrease parent
treatment areas, actual and pretend
virtual reality, Internet technology, anxiety, and increase parent
medical equipment, and various
and electronic and digital devices has satisfaction.47,48 With a goal to
models (dolls, puppets) are used to
been found to be an effective means severely limit the use of papoose
reinforce learning and actively engage
of distraction in reducing pain.7,33–38
the child.1,13 Caregivers should be boards and eliminate the practice of
Child life specialists may also multiple staff members holding
included in the preparation process
develop comfort kits for use in a child down, these techniques
because this can decrease parental
treatment areas to include age- provide a viable and more humane
anxiety and allow them to provide
appropriate distraction items, such alternative in most cases.
essential family-centered
as bubbles, pop-up and sound books,
support.14,15
light-up toys, and other visual or
An experimental evaluation of one auditory tools.39 Distraction CHILD LIFE INTERVENTIONS: THE
child life program model revealed techniques have also been shown to THERAPEUTIC VALUE OF PLAY
that child life interventions resulted be successful in lowering a parent’s Therapeutic play during health care
in less emotional distress, better fear and distress during an invasive experiences is essential and a major
overall coping during the hospital procedure.27 component of a child life program and
Downloaded from www.aappublications.org/news by guest on September 22, 2021
2 FROM THE AMERICAN ACADEMY OF PEDIATRICSof the child life professional’s role. reason video games are so popular is easily transmitted to the patient.64
Play is crucial to a child’s social, with this age group56). Patients in this Child life specialists help facilitate the
emotional, and cognitive age group also benefit from activities family’s adjustment to the child’s
development and is even more that allow them to maintain illness and health care experience by
critical during adversity or stress relationships with peers and establish providing psychosocial support and
points in a child’s life.49 In addition to new connections through, for coping strategies for caregivers. They
its developmentally supportive example, online networking and the can help family members understand
benefits and as a normalizing activity availability of teen-aged activity their child’s response to treatment
for children and youth of all ages, play rooms in the hospital setting.57 and support caregiving roles by
is particularly valuable for children promoting parent-child play sessions
Auxiliary programs, such as animal-
who are anxious or struggling to cope and sharing strategies for comforting
assisted therapy, infant massage
with stressful circumstances of or coaching their children during
instruction, therapeutic clowning,
hospitalization, illness, or grief.50 Erik medical procedures. In addition, child
performing arts, and artist-in-
Erikson51 writes, “To play out is the life specialists play a pivotal role in
residence programs, often used in
most natural auto-therapeutic encouraging and facilitating family
conjunction with child life services and
measure childhood affords. Whatever involvement in the patient’s care as
incorporated into child life
other roles play may have in the well as promoting communication
departments, provide additional
child’s development…the child uses it between family members, providers,
outlets for patients of all ages and
to make up for defeats, sufferings, and and the interdisciplinary team.
their families.58–60 Live, interactive
frustrations.” Play in the health care
programming using closed-circuit
setting is adapted to address unique Siblings of pediatric patients present
television systems and studios can be
needs on the basis of developmental with their own unique anxieties and
a particularly effective way to engage
level, self-directed interests, medical psychosocial needs, not often
patients restricted to their rooms for
condition and physical abilities, assessed or addressed. Siblings, much
infection-control or medical reasons.
psychosocial vulnerabilities, and like children of adult patients, can be
Other interactive technology, such as
setting (eg, bedside, playroom, clinic). helped to comprehend a family
video conferencing, can help patients
Play as a therapeutic modality, member’s illness via therapeutic play
engage with people outside the
including health care play or “medical and educational interventions or by
hospital, including their peers, the
play,” has been found to reduce offering support during hospital
community, and their schools. The
children’s emotional distress and help visits, including diagnoses, critical
ability to connect with a child’s school,
them cope with medical care, and end-of-life situations.65,66
community, and home helps normalize
experiences.52 Research has revealed Although sibling support is essential
the experience by minimizing
that physiologic responses, such as in all areas, a critical care
disruption of usual routines.
palm sweating, excessive body hospitalization in the neonatal or
Expressive therapies, such as those
movement, tachycardia, and pediatric ICU presents additional
provided by distinctly certified play
hypertension, can be reduced with stressors for the entire family, and
therapists, music therapists, and art
therapeutic play interventions.53 child life interventions are often
therapists, can be offered to
focused on the siblings’ psychosocial
Play can be adapted to address the complement child life programs and to
needs. Sibling support may include
developmental and psychosocial needs provide support for particularly
preparing the sibling(s) for an initial
of patients in every pediatric age vulnerable patients.26,61,62
visit and providing ongoing emotional
group. For example, infants and
support throughout the patient’s
toddlers benefit from exploratory and CHILD LIFE INTERVENTIONS: hospital stay. Child life specialists are
sensorimotor play, and preschoolers PARTNERING WITH FAMILIES TO often involved in providing
enjoy fantasy play and creative art PROVIDE SUPPORT bereavement support to patients as
activities.54 Opportunities for parents
The presence and participation of and well as siblings and other family
to engage in play activities with their
partnership with family members is members. Grief support and legacy
young children are beneficial to both
a fundamental component of patient- activities, such as hand molds or
the patient and family, alleviating some
and family-centered care and has memory boxes for siblings and family
feelings of helplessness that can be
a significant positive effect on members, are often provided at the
common in caregivers and assisting in
a child’s adjustment to the health care end of life for both pediatric and adult
the child’s adjustment to the hospital.55
experience.63 When parents or other patients throughout the hospital. In
School-aged children and adolescents family members are highly anxious conjunction with the interdisciplinary
seek play that contributes to feelings about the child’s illness or diagnostic team, child life specialists are critical
of mastery and achievement (one and treatment regimens, such anxiety in helping all family members
Downloaded from www.aappublications.org/news by guest on September 22, 2021
PEDIATRICS Volume 147, number 1, January 2021 3understand how to support children using the shift length as the The remaining 3 areas, inpatient acute
in age-appropriate ways during end- denominator, additional nonpatient care, outpatient ambulatory clinics,
of-life events. care responsibilities are accounted for and critical care units, all have similar
in the productivity calculation, productivity, with approximately 1
including such things as meetings, patient encounter per hour, or 8 in an
RECENT BENCHMARKING DATA committee work, student and staff 8-hour shift.
In 2016, the Association of Child Life education, and donor events.67
The productivity data allow
Professionals (ACLP) constructed the
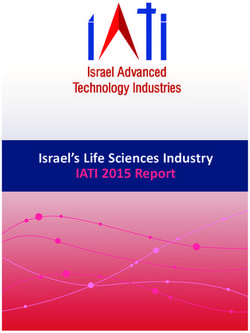
Figure 1 identifies the total number of participating hospitals to clearly
Child Life Professional Data Center
individual patient and family identify how their program compares
(CLPDC), an online database to house
encounters an individual child life to the national average or similar
comprehensive child life program data
specialist provides in an 8-hour shift hospitals on the basis of median
and metrics, including staffing models,
in each of the 6 service areas. In scores. The data also serve as a tool to
staffing ratios, budget allocation data,
support appropriate staffing during
and hospital descriptors.67 Using radiology, the median productivity is
0.74 patient encounters per hour, or hospital program growth by offering
a systematic and evidence-based
approximately 6 encounters in an 8- a benchmark to adjust staffing
approach to measure the impact of
hour day. Of all 6 areas of service, depending on changes in patient
psychosocial services provided to
radiology encounters trend the longest volumes.
pediatric patients and families, this
database has synthesized information because radiologic procedures often Although these ratios establish
from more than 160 child life require significant preparation and national benchmarking and staffing
programs. In addition, the ACLP support during the procedures, which trends, other factors should influence
established a productivity metric may be lengthy. Child life specialists in staffing allocations. Child life services
measuring the number of patient and presurgery and the ED have the should be available to meet identified
family encounters a child life specialist highest median productivity, with an patient and family needs 7 days per
provides in a specified setting within average of 1.2 patient encounters week. Staffing plans should be
the hospital during a shift. Currently, every hour, roughly 10 patients seen sufficient to meet fluctuations in
more than 50 programs have per 8-hour shift in each of these areas. anticipated and unanticipated staff
participated in the productivity data absences, seasonal swings in the
collection. The productivity metric is patient census, and nonclinical
a numerical indicator of the number of Radiology community activities (such as school
patient and family encounters that can Presurgery programming, outreach events, and
be expected during the child life increased visits and in-kind donations
specialist’s shift. This measure of ED during the holiday season). Child
productivity is collected for 6 distinct Inpaent variables (such as age, temperament,
areas of service: (1) inpatient acute coping style, and cognitive abilities),
care units, (2) critical care, (3)
Outpaent family variables (such as caregiver
radiology, (4) presurgery, (5) Crical care anxiety, presence, and involvement)
outpatient ambulatory care, and (6) and diagnosis and treatment variables
the ED. These 6 distinct areas are (acute versus chronic, repeat
being used to collect and segment data
10 admissions, number of invasive
because the type and length of child 8 procedures) are known to affect
life intervention can depend on which psychosocial vulnerability and, thus,
medical service is being provided. A 6 influence the child’s particular child
patient encounter is defined as a child life needs.68 A combination of
life specialist–provided interaction 4 psychosocial risk assessment, medical
with a patient, sibling, or caregiver, and/or treatment variables (eg, the
and this serves as the numerator of 2 proportion of patients on isolation
the productivity metric. The precautions and the volume of patient
denominator is the length of the child 0 and family teaching needs), and the
life specialist’s shift (eg, 8 hours). The Paent Encounters per 8-Hour time requirements associated with
final metric given is the measure of Shi particular interventions directly affect
patient and family encounters per operational staff-to-patient ratios in
hour. These metrics account for FIGURE 1 both inpatient and outpatient settings
Average patient/family encounters per 8-hour
nondirect patient care activities and shift for child life specialists in various hospital and could necessitate a lower ratio of
direct patient care interventions. By settings. patients to child life specialist.69,70
Downloaded from www.aappublications.org/news by guest on September 22, 2021
4 FROM THE AMERICAN ACADEMY OF PEDIATRICSIn addition to establishing a CCLS; and passing a standardized The scope of child life programs has
a benchmarking standard for child certification examination.71 Ongoing developed beyond pediatric inpatient
life specialist and patient encounters, and future requirements for the CCLS acute care settings to include
the CLPDC houses multifaceted credential are determined by the Child outpatient and other areas in which
information, such as types of Life Certification Commission of child life expertise can be effectively
organizations in which child life the ACLP. applied to support children and
specialists work, staffing, program families in stressful situations. Child
funding, reporting structure, services In some settings, child life services are life specialists provide services to
provided, and special services. The augmented by child life assistants (or presurgery and surgical centers,
CLPDC should be used as a resource activity coordinators, child life radiology and imaging departments,
for programs and hospitals in technicians, etc). Child life assistants dialysis centers, ambulatory clinics,
evaluation and continuous are typically required to have core NICUs, urgent care centers,
performance improvement of child college coursework, such as an psychiatric units, hospice programs,
life programming. associate degree in child development, camps for children with chronic
and experience with children in group illness, rehabilitation settings, and
settings. They generally focus on the some outpatient dental and physician
CHILD LIFE STAFFING AND ROLES normalization of the health care offices.76 Because the majority of
experience, providing play activities, children with medical complexities
Child life specialists are part of an coordinating special events
interdisciplinary, patient- and family- are being treated on an outpatient
(community visitors, holiday basis, child life services are
centered model of care, collaborating celebrations, etc), and maintaining the
with the family, physicians, advanced increasingly common outside the
playroom environment. Both child life hospital.77 Increasingly, CCLSs are
practice providers, nurses, social specialists and assistants actively
workers, and other members of the also part of interdisciplinary health
participate in the orientation, training, care teams, including palliative care,
health care team to develop and supervision of volunteers, thereby
a comprehensive plan of care. Child behavioral health, trauma, and child
contributing to volunteer effectiveness, protective services. In cases of
life contributions to this plan are satisfaction, and retention. This
based on the patient’s and family’s hospitalized or ill adults, child life
collaboration enables the child life specialists may be consulted to work
psychosocial needs, cultural heritage, specialist to conduct an assessment
and responses to the health care with children of adult patients,
and delegate as appropriate, allowing particularly in end-of-life, trauma,
experience. Child life specialists can patients with varying degrees of
participate in the care plan by, for and critical care situations.
psychosocial vulnerability and activity
example, teaching a child coping levels to be supported by the team Child life programs continue to evolve
strategies for adjusting to a life- member whose skills and knowledge and adapt to meet the changing health
changing injury, promoting coping are most closely aligned with patient care needs of patients and families.
with examinations for alleged abuse, and family needs. Although volunteers Children with special health care
assisting families in talking to their are a valuable supplement, they can needs now represent 18.8% of all
children about death, facilitating never be considered an adequate children, up from 12.8% in 2001.78
nonpharmacologic pain-management replacement for CCLSs. Specifically, the increase in patients
techniques, preparing and educating
with a diagnosis of autism spectrum
children about their medical care in
disorder presents opportunities for
age-appropriate ways, and EVOLUTION OF CHILD LIFE SERVICES child life specialization in supporting
communicating the child’s
The provision of child life services is this population in medical
developmental and individual needs
a quality benchmark of an integrated settings.36,79,80 In addition, the
and perspective to others. These
patient- and family-centered health number of children with mental health
interventions are most effective when
care system, a recommended and developmental disabilities
delivered in collaboration with the
component of medical education, and conditions is increasing, either alone
entire health care team.
an indicator of excellence in pediatric or comorbid with a physical health
The credentials of a certified child life care.72–74 There are more than 430 condition.81,82 Hospitals are also
specialist (CCLS) currently include the child life programs in operation in admitting children with more complex
minimum of a bachelor’s degree in North America75; most are located in medical conditions, with rates
child life, child development, or freestanding children’s hospitals, doubling between 1991 and 2005, and
a closely related field; the successful children’s hospitals within hospitals, may need greater individualization of
completion of a 600-hour child life community hospitals with pediatric care from the CCLS.83,84 The numbers
internship under the supervision of units, and EDs. of children with disabilities and
Downloaded from www.aappublications.org/news by guest on September 22, 2021
PEDIATRICS Volume 147, number 1, January 2021 5medical complexities are increasing, Although evidence supports the value from the hospital to the home setting
likely because of the increases in of child life services, financial less disruptive. Child life specialists
technology that ensures the survival of pressures in many health care also provide services outside
patients with previously lethal settings have threatened the growth hospital-based settings, including
conditions.85 Given the increasing and sustainability of child life private practice, community agencies,
survival rate of patients with cystic services. In addition to contributions and hospice care, and are becoming
fibrosis, cardiac conditions, spina to the patient experience, the increasingly involved in providing
bifida, short gut, cancer, and other literature has also demonstrated support to children and families
chronic illnesses, more teenagers and financial benefits of child life during catastrophic events.
young adults face the challenging interventions, including reduced
transition to adult health care.86 sedation-related costs, and increased For hospitals or other health care
Acknowledging team goals to compliance during procedures, settings considering the initiation or
normalize the transition process and resulting in procedure expansion of child life services, the
address patient and family anxieties or completion.8–12 A child life program ACLP offers a consultation service to
questions, child life specialists can improves quality and decreases costs support existing program review and
assist in this transition by providing and, therefore, should be included in development, new program startup,
education and helping patients to the value-added equation and interdisciplinary education, and
communicate their needs, fears, hopes, discussion of health care cost, written practice guidelines.94 In
and expectations.87–89 including with payers. community hospital settings with few
pediatric beds and minimal pediatric
In recent years, patient experience outpatient or ED visits, the provision
and/or patient satisfaction has ADDITIONAL CONSIDERATIONS of full-time child life services may not
become a key quality and Child life services contribute to an be financially feasible. In such cases,
performance indicator. Although the organization’s efforts to meet the part-time or consultative services of
definition of patient experience standards set forth by The Joint a CCLS may be obtained to assist in
continues to be explored and honed Commission and other accreditation the ongoing education of staff,
by health care leaders, there is agencies, including effective students, and volunteers as well as to
common agreement that when communication, patient- and family- advise on a psychosocially sound,
evaluating health care quality, patient centered care, age-specific developmentally appropriate patient-
satisfaction is an important metric competencies, and cultural and family-centered approach to care.
that translates to health care ratings competence.92 Child life specialists’ The advancement of telemedicine
and payment.90 Family-centered care psychosocial and developmental also presents an opportunity for child
is a core principle for child life expertise and their keen awareness of life specialists to intervene when they
specialists; the recent emergence of the benefits of patient- and family- cannot be on-site. Advocating for
the patient experience as a key centered care provide a useful child life services as an essential part
quality indicator has resulted in child perspective at a systems level. Child of the interdisciplinary team is
life specialists often taking the lead in life input is often incorporated into a responsibility of health care
family-centered care and patient hospital committees, such as ethics, organizations to ensure it is
experience initiatives. Research family-centered care, patient a standard of pediatric care and
studies have demonstrated the experience, safety, environmental should occur on local and national
positive impact of child life design, bereavement, and strategic levels as well as in regulatory and
intervention on patient and parent planning. Child life expertise has accrediting organizations.
perception and evaluation of the applications beyond conventional
hospital experience, which is hospital care. Interventions can help
increasingly important for incentive- children transition back to their CONCLUSIONS
based reimbursement, accreditation, homes, schools, communities, and Child life services are associated with
marketing, and public reporting of medical homes.11,93 Child life improved quality, outcomes, and
outcomes.8,17,34,67,91 Health care specialists often collaborate with patient and family experiences as well
professionals and organizations local school districts to arrange as decrease costs in pediatric care.
acknowledge the significant impact hospital or homebound education, There is evidence that child life
child life specialists have on the and hospital-based teachers may be services help to contain costs by
patient experience as well as the role incorporated into child life program reducing the length of stay,
child life plays in helping the concept administration. These interventions decreasing the need for sedation and
of patient experience continue to help provide continued normalization analgesics, and increasing patient
evolve and grow.80 and help make the transition to and satisfaction ratings. Patient
Downloaded from www.aappublications.org/news by guest on September 22, 2021
6 FROM THE AMERICAN ACADEMY OF PEDIATRICSexperience data and interdisciplinary 4. Child life services staffing must be AAP COMMITTEE ON HOSPITAL CARE,
team member feedback further individualized to address the 2018–2019
confirm the positive effects of child needs of specific inpatient and Jennifer Jewell, MD, FAAP, Chairperson
life programs on children, families, outpatient areas. The ratio of child Kimberly Ernst, MD, MSMI, FAAP
and staff. It remains essential for life specialist to patient should be Vanessa Hill, MD, FAAP
Benson Hsu, MD, FAAP – Section on
child life services to adapt and grow adjusted to account for the
Critical Care
with the changing health care patient’s medical, psychosocial, Vinh Lam, MD, FAAP
delivery system in support of the and developmental complexity and Melissa Mauro-Small, MD, FAAP – Section on
highest possible quality of care for vulnerability as well as family Hospital Medicine
children and their families. needs and preferences. Child life Charles Vinocur, MD, FAAP
services need to continuously
RECOMMENDATIONS evolve to meet the changing needs FORMER COMMITTEE ON HOSPITAL CARE
in pediatric health care, including MEMBER, 2017–2018
1. Child life collaboration with the
the significant increases in Daniel A. Rauch, MD, FAAP
entire interdisciplinary team is
children with disabilities and
essential to meeting the overall
medical complexity.
health care needs of children and LIAISONS
families. 5. Child life services optimize
Karen Castleberry – Family Representative
pediatric health care and, Nancy Hanson – Children’s Hospital
2. Child life services are part of an
therefore, should be included in Association
integrated patient- and family-
the hospital operating budget; they Kristin Hittle Gigli, PhD, RN, CPNP-AC, CCRN
centered model of care and can be – National Association of Pediatric Nurse
cannot solely rely on contingency
used as a quality measure in the Practitioners
or philanthropic funding.
delivery of health care services for Michael S. Leonard, MD, MS, FAAP –
children and families. 6. Legislative advocacy of child life Representative to The Joint Commission
services by pediatricians and other Barbara Romito, MA, CCLS – Association of
3. Child life services, provided directly Child Life Professionals
stakeholders is recommended at
by CCLSs, are recommended in
the state and federal levels.
pediatric inpatient units, EDs,
7. Additional research is needed to STAFF
chronic care centers, and other
diagnostic and treatment areas to further identify the impact of child S. Niccole Alexander, MPP
the extent appropriate for the life services on patient care
population served. In hospitals outcomes, including patient
with a small number of inpatient or experience, cost-effectiveness, and ABBREVIATIONS
outpatient pediatric visits, ongoing quality and safety measures.
ACLP: Association of Child Life
consultation with a CCLS is needed Professionals
to educate health care team CCLS: certified child life specialist
members and support LEAD AUTHORS CLPDC: Child Life Professional
developmentally appropriate Barbara Romito, MA, CCLS Data Center
patient- and family-centered Jennifer Jewell, MD, FAAP ED: emergency department
practice. Meredith Jackson, MD, FAAP
FUNDING: No external funding.
POTENTIAL CONFLICT OF INTEREST: The authors have indicated they have no potential conflicts of interest to disclose.
REFERENCES
1. William Li HC, Lopez V, Lee TLI. Effects of Anesthesiol Clin North Am. 2005;23(4): research-ebp/ebp-statements.pdf?
preoperative therapeutic play on 597–614, vii sfvrsn=2. Accessed November 5, 2020
outcomes of school-age children
3. Koller D. Child Life Council Evidence- 4. Vantaa Benjaminsson M, Thunberg G,
undergoing day surgery. Res Nurs
Based Practice Statement: Preparing Nilsson S. Using picture and text
Health. 2007;30(3):320–332
Children and Adolescents for Medical schedules to inform children: effects on
2. Kain ZN, Caldwell-Andrews AA. Procedures. Rockville, MD: Child Life distress and pain during needle-related
Preoperative psychological preparation Council; 2009. Available at: https://www. procedures in nitrous oxide sedation.
of the child for surgery: an update. childlife.org/docs/default-source/ Pain Res Treat. 2015;2015:478503
Downloaded from www.aappublications.org/news by guest on September 22, 2021
PEDIATRICS Volume 147, number 1, January 2021 75. Brewer S, Gleditsch SL, Syblik D, Tietjens procedural anxiety and behavioral 25. Lipsitz JD, Gur M, Albano AM, Sherman
ME, Vacik HW. Pediatric anxiety: child life distress. Epilepsy Behav. 2013;27(1): B. A psychological intervention for
intervention in day surgery. J Pediatr 169–173 pediatric chest pain: development and
Nurs. 2006;21(1):13–22 15. He HG, Zhu L, Chan SWC, Klainin-Yobas P, open trial. J Dev Behav Pediatr. 2011;
Wang W. The effectiveness of therapeutic 32(2):153–157
6. Fortier MA, Bunzli E, Walthall J, et al.
Web-based tailored intervention for play intervention in reducing
26. Nguyen TN, Nilsson S, Hellström AL,
preparation of parents and children for perioperative anxiety, negative
Bengtson A. Music therapy to reduce
outpatient surgery (WebTIPS): formative behaviors, and postoperative pain in
pain and anxiety in children with cancer
evaluation and randomized controlled children undergoing elective surgery:
undergoing lumbar puncture:
trial. Anesth Analg. 2015;120(4):915–922 a systematic review. Pain Manag Nurs.
a randomized clinical trial. J Pediatr
2015;16(3):425–439
7. Lan YP, Huang ZH, Finley GA, Zuo YX. Oncol Nurs. 2010;27(3):146–155
Effects of the combination of mask 16. Wolfer J, Gaynard L, Goldberger J,
Laidley LN, Thompson R. An experimental 27. Burgess S, Nativio DG, Penrose JE.
preconditioning with midazolam Quality improvement project to reduce
evaluation of a model child life program.
pretreatment on anxiety and mask pain and distress associated with
acceptance during pediatric inhalational Child Health Care. 1988;16(4):244–254
immunization visits in pediatric primary
induction and postoperative mask fear 17. Gursky B, Kestler LP, Lewis M. care. J Pediatr Nurs. 2015;30(2):294–300
in children. [published correction Psychosocial intervention on procedure-
appears in Chin Med J (Engl). 2016; related distress in children being 28. Canbulat N, Inal S, Sönmezer H. Efficacy
129(12):1463]. Chin Med J (Engl). 2012; treated for laceration repair. J Dev of distraction methods on procedural
125(11):1908–1914 Behav Pediatr. 2010;31(3):217–222 pain and anxiety by applying distraction
cards and kaleidoscope in children.
8. Törnqvist E, Månsson Å, Hallström I. 18. Madhok M, Milner D, Teele M, Finkelstein
Asian Nurs Res (Korean Soc Nurs Sci).
Children having magnetic resonance M. Child life services and patient
2014;8(1):23–28
imaging: a preparatory storybook and satisfaction in emergency department
audio/visual media are preferable to [abstract]. Pediatr Emerg Care. 2007; 29. Hedén L, VON Essen L, Ljungman G.
anesthesia or deep sedation. J Child 23(10):764 Randomized interventions for needle
Health Care. 2015;19(3):359–369 19. Cohen LL. Behavioral approaches to procedures in children with cancer. Eur
anxiety and pain management for J Cancer Care (Engl). 2009;18(4):
9. Khan JJ, Donnelly LF, Koch BL, Curtwright
pediatric venous access. Pediatrics. 358–363
LA, Dickerson JM, Hardin JL. A program
to decrease the need for pediatric 2008;122(suppl 3):S134–S139 30. Inal S, Kelleci M. Distracting children
sedation for CT and MRI. Appl Radiol. 20. Eldridge C, Kennedy R. during blood draw: looking through
2007;36(4):30–33 Nonpharmacologic techniques for distraction cards is effective in pain
10. Scott MT, Todd KE, Oakley H, et al. distress reduction during emergency relief of children during blood draw. Int
Reducing anesthesia and health care medical care: a review. Clin Pediatr J Nurs Pract. 2012;18(2):210–219
cost through utilization of child life Emerg Med. 2010;11(4):244–250 31. Sadeghi T, Mohammadi N, Shamshiri M,
specialists in pediatric radiation 21. Srouji R, Ratnapalan S, Schneeweiss S. Bagherzadeh R, Hossinkhani N. Effect of
oncology. Int J Radiat Oncol Biol Phys. Pain in children: assessment and distraction on children’s pain during
2016;96(2):401–405 nonpharmacological management. Int intravenous catheter insertion. J Spec
11. Grissom S, Boles J, Bailey K, et al. Play- J Pediatr. 2010;2010:474838 Pediatr Nurs. 2013;18(2):109–114
based procedural preparation and 22. Uman LS, Chambers CT, McGrath PJ, 32. Ha YO, Kim HS. The effects of audiovisual
support intervention for cranial Kisely S. Psychological interventions for distraction on children’s pain during
radiation. Support Care Cancer. 2016; needle-related procedural pain and laceration repair. Int J Nurs Pract. 2013;
24(6):2421–2427 distress in children and adolescents. 19(suppl 3):20–27
12. Durand DJ, Young M, Nagy P, Tekes A, Cochrane Database Syst Rev. 2006;(4):
CD005179 33. Brown NJ, Kimble RM, Rodger S, Ware
Huisman TAGM. Mandatory child life
RS, Cuttle L. Play and heal: randomized
consultation and its impact on pediatric 23. Baxter AL, Cohen LL, McElvery HL, controlled trial of DittoTM intervention
MRI workflow in an academic medical Lawson ML, von Baeyer CL. An efficacy on improving re-epithelialization
center. J Am Coll Radiol. 2015;12(6): integration of vibration and cold relieves in pediatric burns. Burns. 2014;40(2):
594–598 venipuncture pain in a pediatric 204–213
13. Goldberger J, Mohl AL, Thompson R. emergency department. Pediatr Emerg
Care. 2011;27(12):1151–1156 34. Shahid R, Benedict C, Mishra S, Mulye M,
Psychological Preparation and Coping.
Guo R. Using iPads for distraction to
In: Thompson RH, ed. The Handbook of 24. Berberich FR, Landman Z. Reducing
reduce pain during immunizations. Clin
Child Life: A Guide for Pediatric immunization discomfort in 4- to 6-year-
Psychosocial Care, 1st ed. Springfield, IL: Pediatr (Phila). 2015;54(2):145–148
old children: a randomized clinical trial.
Charles C Thomas; 2009:160–198 Pediatrics. 2009;124(2). Available at: 35. Nilsson S, Renning AC. Pain management
14. Benore E, Enlow T. Improving pediatric www.pediatrics.org/cgi/content/full/124/ during wound dressing in children. Nurs
compliance with EEG: decreasing 2/e203 Stand. 2012;26(32):50–55
Downloaded from www.aappublications.org/news by guest on September 22, 2021
8 FROM THE AMERICAN ACADEMY OF PEDIATRICS36. Isong IA, Rao SR, Holifield C, et al. 47. Stephens BK, Barkey ME, Hall HR. 57. Nicholas DB, Darch J, McNeill T, et al.
Addressing dental fear in children with Techniques to comfort children during Perceptions of online support for
autism spectrum disorders: stressful procedures. Adv Mind Body hospitalized children and adolescents.
a randomized controlled pilot study Med. 1999;15(1):49–60 Soc Work Health Care. 2007;44(3):
using electronic screen media. Clin 205–223
48. Sparks LA, Setlik J, Luhman J. Parental
Pediatr (Phila). 2014;53(3):230–237 holding and positioning to decrease IV 58. Rollins JA. The Arts in Children’s
37. Borges L, Huber D, Lugo S. Harnessing distress in young children: Health-Care Settings. In: Rollins JA, Bolig
the power of digital devices. Pediatr a randomized controlled trial. J Pediatr R, Mahan C, eds. Meeting Children’s
Nurs. 2011;37(2):88 Nurs. 2007;22(6):440–447 Psychosocial Needs Across the
Health-Care Continuum, 1st ed. Austin,
38. Nilsson S, Finnström B, Kokinsky E, 49. Yogman M, Garner A, Hutchinson J,
TX: Pro-Ed; 2005:119–174
Enskär K. The use of virtual reality for Hirsh-Pasek K, Golinkoff RM; Committee
needle-related procedural pain and on Psychosocial Aspects of Child and 59. Kaminski M, Pellino T, Wish J. Play and
distress in children and adolescents in Family Health; Council on pets: the physical and emotional impact
a paediatric oncology unit. Eur J Oncol Communications and Media. The power of child-life and pet therapy on
Nurs. 2009;13(2):102–109 of play: a pediatric role in enhancing hospitalized children. Child Health Care.
development in young children. 2002;31(4):321–335
39. Blaine S. The where, why and how: Pediatrics. 2018;142(3):e20182058
60. Heilbrunn BR, Wittern RE, Lee JB, Pham
coping kits and distraction. Child Life
50. Brown CD. Therapeutic Play and Creative PK, Hamilton AH, Nager AL. Reducing
Focus. 1999;1(1):1–6
Arts: Helping Children Cope with Illness, anxiety in the pediatric emergency
40. Bandstra NF, Skinner L, Leblanc C, et al. Death, and Grief. In: Armstrong-Dailey A, department: a comparative trial.
The role of child life in pediatric pain Zarbock S, eds. Hospice Care for J Emerg Med. 2014;47(6):623–631
management: a survey of child life Children, 3rd ed. New York, NY: Oxford
61. Avers L, Mathur A, Kamat D. Music
specialists. J Pain. 2008;9(4):320–329 University Press; 2009:305–338
therapy in pediatrics. Clin Pediatr
41. Heckler-Medina GA. The importance of 51. Erikson EH. Studies in the interpretation (Phila). 2007;46(7):575–579
child life and pain management during of play: clinical observation of play
62. Councill T. Medical Art Therapy with
vascular access procedures in disruption in young children. Genet
Children. In: Malchiodi C, ed. Handbook
pediatrics. Journal of the Association Psychol Monogr. 1940;22:557–671
of Art Therapy, 1st ed. New York, NY:
for Vascular Access. 2006;11(3):144–151 52. Fereday J, Darbyshire P. Making the wait Guilford Press; 2003:207–219
42. Lawes C, Sawyer L, Amos S, Kandiah M, easier: evaluating the role of supervised
63. Committee on Hospital Care, American
Pearce L, Symons J. Impact of an play in a surgical admission area.
Academy of Pediatrics. Family-centered
education programme for staff working Neonatal, Paediatric and Child Health
care and the pediatrician’s role.
with children undergoing painful Nursing. 2008;11(1):4–9
Pediatrics. 2003;112(3, pt 1):691–697
procedures. Paediatr Nurs. 2008;20(2): 53. Koller D. Child Life Council Evidence-
64. Lewindowski L, Baranowski MV.
33–37 Based Practice Statement: Therapeutic
Psychological aspects of acute trauma:
Play in Pediatric Health Care: The
43. Pederson C. Nonpharmacologic intervening with children and families in
Essence of Child Life Practice. Rockville,
interventions to manage children’s pain: the inpatient setting. Child Adolesc
MD: Child Life Council; 2009. Available at:
immediate and short-term effects of Psychiatr Clin N Am. 1994;3(3):513–529
https://www.childlife.org/docs/default-
a continuing education program.
source/research-ebp/ebp-statements. 65. Gursky B. The effect of educational
J Contin Educ Nurs. 1996;27(3):131–140
pdf?sfvrsn=2. Accessed November 5, interventions with siblings of
44. Schechter NL. From the ouchless place 2020 hospitalized children. J Dev Behav
to comfort central: the evolution of Pediatr. 2007;28(5):392–398
54. Hughes FP. Children, Play, and
a concept. Pediatrics. 2008;122(suppl 3): Development, 4th ed. Thousand Oaks, CA: 66. Prchal A, Graf A, Bergstraesser E,
S154–S160 SAGE Publications, Inc; 2010 Landolt MA. A two-session psychological
45. Leahy S, Kennedy RM, Hesselgrave J, intervention for siblings of pediatric
55. Melnyk BM, Alpert-Gillis L, Feinstein NF,
Gurwitch K, Barkey M, Millar TF. On the cancer patients: a randomized
et al. Creating opportunities for parent
front lines: lessons learned in controlled pilot trial. Child Adolesc
empowerment: program effects on the
implementing multidisciplinary Psychiatry Ment Health. 2012;6(1):3
mental health/coping outcomes of
peripheral venous access pain- critically ill young children and their 67. Association of Child Life Professionals.
management programs in pediatric mothers. Pediatrics. 2004;113(6). Child Life Professional Data Center.
hospitals. Pediatrics. 2008;122(suppl 3): Available at: www.pediatrics.org/cgi/ Available at: https://www.childlife.org/
S161–S170 content/full/113/6/e597 resources/for-child-life-specialists/child-
life-professional-data-center. Accessed
46. Lacey CM, Finkelstein M, Thygeson MV. 56. Olson CK. Children’s motivations for
May 1, 2018
The impact of positioning on fear during video game play in the context of normal
immunizations: supine versus sitting up. development. Rev Gen Psychol. 2010; 68. Koller D. Child Life Council Evidence-
J Pediatr Nurs. 2008;23(3):195–200 14(2):180–187 Based Practice Statement: Child Life
Downloaded from www.aappublications.org/news by guest on September 22, 2021
PEDIATRICS Volume 147, number 1, January 2021 9Assessment: Variables Associated With Available at: http://community.childlife. approaches. Pediatrics. 2002;110(6, pt
a Child’s Ability to Cope with org. Accessed May 1, 2018 2):1315–1321
Hospitalization. Rockville, MD: Child Life 76. Hicks M, ed.. Child Life Beyond the
Council; 2009. Available at: https://www. 87. Cooley WC, Sagerman PJ; American
Hospital, 1st ed. Rockville, MD: Child Life Academy of Pediatrics; American
childlife.org/docs/default-source/ Council; 2008
research-ebp/ebp-statements.pdf? Academy of Family Physicians; American
sfvrsn=2. Accessed November 5, 2020 77. Berry JG, Hall M, Neff J, et al. Children College of Physicians; Transitions
with medical complexity and Medicaid: Clinical Report Authoring Group.
69. Turner JC, Fralic J. Making explicit the Supporting the health care transition
spending and cost savings. Health Aff
implicit: child life specialists talk about from adolescence to adulthood in the
(Millwood). 2014;33(12):2199–2206
their assessment process. Child Youth medical home. Pediatrics. 2011;128(1):
Care Forum. 2009;38:39–54 78. Centers for Disease Control and
182–200
Prevention. National survey of children
70. Hollon E, Skinner L. Assessment and
with special health care needs. Available 88. Transitioning Youth to an Adult Health
Documentation in Child Life. In:
at: https://www.cdc.gov/nchs/slaits/ Care Clinician. Available at: https://
Thompson R, ed. The Handbook of Child
cshcn.htm. Accessed October, 2018 gottransition.org/six-core-elements/
Life: A Guide for Pediatric Psychosocial
Care, 1st ed. Springfield, IL: Charles C 79. Seid M, Sherman M, Seid AB. transitioning-youth-to-adult/. Accessed
Thomas; 2009:116–135 Perioperative psychosocial interventions November 5, 2020
for autistic children undergoing ENT 89. Orkoskey N. Transitioning Patients with
71. Child Life Council, Child Life Certifying
surgery. Int J Pediatr Otorhinolaryngol.
Committee. Child Life Professional Cystic Fibrosis from Pediatric to Adult
1997;40(2–3):107–113
Certification Candidate Manual. Care: A Lifelong Process. Rockville, MD:
Rockville, MD: Child Life Council; 2011. 80. The Beryl Institute. What patient Child Life Council; 2009
Available at: https://www.childlife.org/ experience can learn from child life.
docs/default-source/certification/ Available at: https://www. 90. Wolf JA, Niederhauser V, Marshburn D,
candidate-manual.pdf?sfvrsn=10. theberylinstitute.org/store/ViewProduct. LaVela SL. Defining patient experience.
Accessed November 5, 2020 aspx?id=11084124. Accessed May 1, 2018 Patient Exp J. 2014;1(1):7–19
72. National Association of Children’s 81. Perou R, Bitsko RH, Blumberg SJ, et al.; 91. Tyson ME, Bohl DD, Blickman JG. A
Hospitals and Related Institutions. Centers for Disease Control and randomized controlled trial: child
Pediatric Excellence in Health Delivery Prevention (CDC). Mental health life services in pediatric imaging.
Systems. Alexandria, VA: National surveillance among children–United Pediatr Radiol. 2014;44(11):1426–
Association of Children’s Hospitals and States, 2005-2011. MMWR Suppl. 2013; 1432
Related Institutions; 1996:9–10 62(2):1–35
92. The Joint Commission. Advancing
73. Accreditation Council for Graduate 82. Houtrow AJ, Larson K, Olson LM, Effective Communication, Cultural
Medical Education. Program Newacheck PW, Halfon N. Changing Competence, and Patient- and Family-
Requirements for Graduate Medical trends of childhood disability, 2001-2011. Centered Care: A Roadmap for
Education in Pediatrics. Chicago, IL: Pediatrics. 2014;134(3):530–538 Hospitals. Oakbrook Terrace, IL: The
Accreditation Council for Graduate Joint Commission; 2010. Available at:
83. Burns KH, Casey PH, Lyle RE, Bird TM,
Medical Education; 2007. Available at: www.jointcommission.org/Advancing_
Fussell JJ, Robbins JM. Increasing
https://www.acgme.org/Portals/0/ Effective_Communication/. Accessed
prevalence of medically complex
PFAssets/ProgramRequirements/320_ May 1, 2018
children in US hospitals. Pediatrics.
Pediatrics_2020.pdf?ver=2020-06-29-
2010;126(4):638–646
162726-647. Accessed November 5, 2020 93. Medical Home Initiatives for Children
84. Simon TD, Berry J, Feudtner C, et al. With Special Needs Project Advisory
74. Olmstead MG, Powell R, Murphy J, et al.
Children with complex chronic Committee, American Academy of
Methodology: US News & World Report
conditions in inpatient hospital settings Pediatrics. The medical home.
Best Children’s Hospitals 2019–2020.
in the United States. Pediatrics. 2010; Pediatrics. 2002;110(1, pt 1):
Research Triangle Park, NC: RTI
126(4):647–655 184–186
International; 2019. Available at: https://
www.usnews.com/static/documents/ 85. Kuo DZ, Houtrow AJ; Council on Children 94. Association of Child Life Professionals.
health/best-hospitals/BCH_ With Disabilities. Recognition and Program review and development
Methodology_2019-20.pdf. Accessed management of medical complexity. services. Available at: https://www.
November 5, 2020 Pediatrics. 2016;138(6):e20163021
childlife.org/resources/for-child-life-
75. Association of Child Life Professionals. 86. Scal P. Transition for youth with chronic specialists/program-review. Accessed
Directory of child life programs. conditions: primary care physicians’ November 5, 2020
Downloaded from www.aappublications.org/news by guest on September 22, 2021
10 FROM THE AMERICAN ACADEMY OF PEDIATRICSChild Life Services
Barbara Romito, Jennifer Jewell, Meredith Jackson and AAP COMMITTEE ON
HOSPITAL CARE; ASSOCIATION OF CHILD LIFE PROFESSIONALS
Pediatrics 2021;147;
DOI: 10.1542/peds.2020-040261 originally published online December 28, 2020;
Updated Information & including high resolution figures, can be found at:
Services http://pediatrics.aappublications.org/content/147/1/e2020040261
References This article cites 69 articles, 13 of which you can access for free at:
http://pediatrics.aappublications.org/content/147/1/e2020040261#BI
BL
Subspecialty Collections This article, along with others on similar topics, appears in the
following collection(s):
Committee on Hospital Care
http://www.aappublications.org/cgi/collection/committee_on_hospita
l_care
Permissions & Licensing Information about reproducing this article in parts (figures, tables) or
in its entirety can be found online at:
http://www.aappublications.org/site/misc/Permissions.xhtml
Reprints Information about ordering reprints can be found online:
http://www.aappublications.org/site/misc/reprints.xhtml
Downloaded from www.aappublications.org/news by guest on September 22, 2021Child Life Services
Barbara Romito, Jennifer Jewell, Meredith Jackson and AAP COMMITTEE ON
HOSPITAL CARE; ASSOCIATION OF CHILD LIFE PROFESSIONALS
Pediatrics 2021;147;
DOI: 10.1542/peds.2020-040261 originally published online December 28, 2020;
The online version of this article, along with updated information and services, is
located on the World Wide Web at:
http://pediatrics.aappublications.org/content/147/1/e2020040261
Pediatrics is the official journal of the American Academy of Pediatrics. A monthly publication, it
has been published continuously since 1948. Pediatrics is owned, published, and trademarked by
the American Academy of Pediatrics, 345 Park Avenue, Itasca, Illinois, 60143. Copyright © 2021
by the American Academy of Pediatrics. All rights reserved. Print ISSN: 1073-0397.
Downloaded from www.aappublications.org/news by guest on September 22, 2021You can also read