Breast Cancer in Pregnancy - "back from St.Gallen 2013" Giovanni Giardina
←
→
Page content transcription
If your browser does not render page correctly, please read the page content below
Epidemiology
* Breast cancer is the most common malignancy occuring
during pregnancy.
* It has been estimated that up to 3.8% of breast cancer
may be diagnosed in women who are pregnant.
(median age 33-34 yrs; median gestational age 17-25 ws)
* Approximately, 1 in 3000 – 3500 pregnancies is
associated with cancer
A. Frederic, EJC,2010* The incidence is expected to increase further with
the rising trend of delaying childbirth to later in
life.
* There is generally limited experience in treating this
clinical setting of breast cancer and the management
presents a considerable challenge, mandating changes
in approach to the diagnosis, staging and planning of
locoregional and systemic therapies.
S, McGrath, Ther.Adv.Med.Oncol.,2011The diagnosis may be difficult due to pregnancy
related physiological changes of the breast.
Average delay from the first symptoms ranges
from 1 to 2 months.
Delay of diagnosis by 1 month may increase the
risk of nodal involvement by 0.9%.Diagnosis
Similar to non-pregnant women, the diagnosis
is based on
* clinical examination
* mammography
* ultrasound
* magnetic resonance imaging
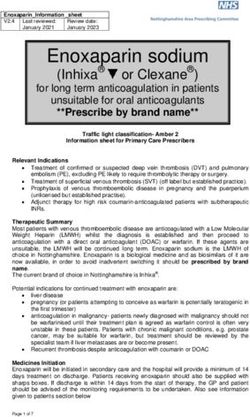
* cito-histologyStaging Procedures Staging procedures, including radiology, should always be executed if they are likely to change therapeutic decisions. Thereshold related deterministic radiation effects, such as mental retardation and organ malformations, only arise above a dose of 0.1-0.2 Gy.
Possibilità terapeutiche
CHIRURGIA
CHEMIOTERAPIA
RADIOTERAPIA
da definire in funzione del periodo di gestazione
>>>> in modo interdisciplinare e con la pazienteCHEMOTHERAPY
adjuvant/neoadjuvant
* MATERNAL PHYSIOLOGY
decreased plasma albumin/increases other proteins
will alter drug-protein binding
amniotic fluid (pharmacological third space)
may be delayed the drug elimination* FETAL DEVELOPEMENT
Organogenesis takes place during the first
10 weeks
p-glycoprotein expressed in the human
placenta may reduce fetal exposure to
sevaral antineoplastic agents
Ring et al. 2005In general, insults during the first trimester can
result in major malformations.
Once organogenesis is complete, such malfomations
are unlikely.
………. BUT
Chemotherapy after the first trimester is not without
risk as the foetus still needs to grow and mature.
(central nervous system and gonads)
H.A. AZIM, The Breast,2011RECOMANDATION of an international
consensus meeting (EJC,46,2010)
Regimens that could be used in the (neo)adjuvant setting:
* FEC / EC / FAC / AC / Taxanes
(non-DNA damaging / very low transfer rate)
* weekly Epirubicin
(fetal safety data / insufficient efficacy data)
F.Peccatori et al. 2009Study n° pts Regimen weeks at weeks at birth congenital
start delivery weight anomalies
Cardonick 130 AC/FAC 20.4+/- 5.4 35.8+/-1.9 2836+/- 4 cases
2010 FEC/ADM 1075 pyloric stenosis
VNR/TAX pul-artery fistula
encephalopathy
hemangioma
Hahn 57 FAC 23(11-34) 37(29-42) 2890 3 cases
2006 (1389-3977) down’s syndrome
ureter. reflux
club foot
Peccatori 20 EpiADM w 19(16-30) 35(28-40) -- 1 case
2009 ADM based polycyst. kidney
Azim 26 ADM based 2° trim. 35(28-40) -- 1 case
2008 polycist. kidney
Ring 28 AC/EC 20(15-33) 37(30-40) 3000 nil
2005
Ther. Advances Med. Oncol. 2011Given the potential fetal toxicity of Methotrexate
CMF should not be used
The Panel concludes that whilst the long term outcome
of children exposed in utero to Chemotherapy is poorly
documented, the evailable evidence is reassuring with
regard to outcome and Chemotherapy should not be
withheld for fetal reasons in the second and third
trimester of pregnancy.OTHER AGENTS
TRASTUZUMAB is not recommended
oligo/anhydramnios
neonatal deaths (4 cases) secondary to
respiratory and renal failure
TAMOXIFEN is not recommended
various birth defects
delaying hormonal treatment, if indicated, after
delivery/chemotherapy will not reduce efficacyLAPATINIB is not a standard tratment for early BC
its use during pregnancy cannot be recommended
(massive transplacental transfer; concerns regar-
ding the use of anti-HER2 agents)
BEVACIZUMAB
its mode of action would strongly caution against
using it during pregnancySUPPORTIVE THERAPY
Metoclopramide, Alizapride, 5-HT antagonists,
NK1 antagonists, G-CSF and Erythropoietin
are SAFE
Methylpredisolone or Hydrocortisone is preferred over
Dexa/Betamethasone
(repeted courses of 12 mg betamethasone for lung
maturation have higher rates of attention problems
and cerebral palsy in more children at the age of 2)IMPORTANT ISSUES
Before starting staging and treatment :
an US of the foetus should be performed
Before every cycle of chemotherapy :
an evaluation of fetal morphology, growth and
wellbeing must be carried out by US and, if
indicated with Doppler including the peak
systolic velocity of the middle cerebral arteryChemotherapy should not be administred :
after 35 weeks (spontaneous labour, risk of
neutropaenia at the time of delivery, limited
capacity to metabolise and eliminate drugs
due to liver and renal immaturity)
Chemotherapy can be restarted when needed after
delivery
1 week only is needed (uncomplicated cesarean)Although placental metastasis in breast cancer are rare :
* the placenta should be analysed
histopathologically
In absence of safety data :
* breastfeeding shortly after chemotherapy
is not recommended.
* primary inhibition of milk production is needed
because especially lipophylic agents as taxanes
can accumulate in the milkTAKE HOME MESSAGES * Efficient treatment of BC during pregnancy is possible * Diagnostic procedures/Staging imaging/Chemotherapy are feseable but should be discussed by a multidisci- plinary team with sufficient expertise (distant disease staging can be postponed after delivery)
*Chemotherapy can be administred during the second and third trimester. Although preliminary data indicate that the serum levels of cytotoxic drugs are lower during pregnancy, standard dosages based on actual heigh and weight should be used
* Trastuzumab and Tamoxifen should be avoided * If possible, delivery should not be induced before the 37° week * In recent studies, no significant reduction in RFS and OS has been seen with termination of pregnancy * Several studies have indicated that the prognosis for pregnant patients may not be worse than for age and stage-matched nonpregnant controls
The Panel recommends a plan of care that integrates the physical and emotional well being of the mother with the health of the foetus Referral to an experienced multidisciplinary team, including neonatal, perinatal, obstetrical, breast surgical and oncological care is recommended
CASO CLINICO
C.A. 35 anni *anamnesi familiare negativa *nessuna patologia di rilievo *1 gravidanza a termine a 32 anni Dicembre 2011, in corso di controllo ginecologico si rileva nodulo QSE Sx
Esegue ECOGRAFIA che conferma nodulo
con aspetti di malignità
FNAC = C 5
ER 45% PgR-voDopo discussione con la paziente e marito
19.01.2012 QUADRANTECTOMIA SE Sx
+ BLNS
Es. Istologico: Carcinoma duttale, G 3
ER 95% PgR 2% Ki67 29%
p53 2% HER2-vo (FDA 1+)
inv. vascolare: assente
Stadio TNM: pT1c (1.2cm) pN0sn (0/3)
M0 (non eseguita Scinti ossea)Si era alla 15° settimana di gravidanza QUALE TERAPIA ADIUVANTE ??? * rischio di recidiva locale (indicazione x RT) * rischio di recidiva a distanza (indicazione x Chemio-Endocrino)
ADJUVANT on line RISCHIO DI MORTE a 10 anni senza terapia 14% con OT beneficio 3.9 con CHT “” 5.3 CHT + OT “” 7.7 RISCHIO DI RICADUTA senza terapia 33% con OT beneficio 11.3 con CHT “” 14.4 CHT + 0T “” 21.0
In paziente non gravida
Si proporrebbe :
* EC x 4 (durata: 12 sett.)
* RADIOTERAPIA (60 Gy; 6 sett.)
* ENDOCRINOTERAPIA completa
(LH-RHa da subito e Tamoxifene)NELLA NOSTRA PAZIENTE
* ENDOCRINOTERAPIA
non proponibile !!!
* CHEMIOTERAPIA
fattibile nel 2°/3° trimestre
* RADIOTERAPIA
non fattibile nel 3° trimestreRADIOTERAPIA subito ??
inizio alla 16°/17° settimana
durata 6 settimane
(fine a 22°/23° settimana = nel 2° trimestre)
ERA POSSIBILE !!!!CHEMIOTERAPIA subito ??
inizio alla 18° settimana
con EpiADM settimanale x 16
(fine alla 34° settimana)
POTEVA andare bene !!!!
e dopo il parto: RT e inizio di OTNULLA
Avrebbe comportato dilazionare la terapia
adiuvante di 5 mesi,
…… scelta non “ottimale”
in termini di riduzione del rischio
per la madreQUALE CHEMIOTERAPIA
Adjuvant on line
senza T Antra Antra
(mono) (based)
OS 10aa 86% 91% 91%
DFS 10aa 67% 80% 81%QUINDI, si poteva proporre
(ragionevolmente)
a 4 settimane da intervento (18° settimana; 2° trimestre)
CHEMIOTERAPIA con EC x 4 oppure
EpiADM settimanale x 16
arrivando così alla 30° o 34° settimana
e poi RT + OT dopo il parto (naturale o indotto
alla 36°/37° settimanaLa paziente ha eseguito 16 settimane di Chemioterapia ben tollerata, eccetto episodio di Neuropenia G4 E’ stata monitorata settimanalmente dai Colleghi Ginecologi
Il 1° agosto 2012 è nato Matteo che sta crescendo “vivo e vegeto” La pz ha eseguito Radioterapia e avviato terapia Endocrina completa con LHRHa e Tamoxifene che continuerà per 5 anni
European Task Forse on Cancer in Pregnancy
German Breast Group
European Society of Gynecological Oncology
(www.cancerinpregnancy.org)Centro Multidisciplinare di Senologia - Varese
GRAZIE per l’attenzione
You can also read