GEORGIA: Enhancing healthcare access through a state-wide telehealth network - ASTHO
←
→
Page content transcription
If your browser does not render page correctly, please read the page content below
CASE STUDY: ENHANCING SYSTEMS TO IMPROVE HEALTH OUTCOMES
CASE STUDY:: Enhancing Systems to Improve Health Outcomes
GEORGIA: Enhancing healthcare access
through a state-wide telehealth network
The Association of State and Territorial Health level while understanding the conditions necessary
Officials (ASTHO), in partnership with the to implement change, key actions needed to
United Health Foundation (UHF) engaged in support change, and the components of account-
a nation-wide learning collaborative with five ability to measure change.
states. The learning collaborative focused on
five states working to improve health outcomes This case study highlights the health systems
around diabetes, obesity, infant mortality, and/ transformation currently taking place in Georgia.
or smoking through systems-level changes in an In order for this transformation to take place, the
effort to improve their America’s Health Ranking®. Georgia Department of Health (DPH) has initiated
All states participating in this learning collab- primary care and public health integration
orative utilized the Plan, Do, Study, Act (PDSA) efforts bringing together state, local, community,
quality improvement model to identify areas of and clinical partnerships across the state. The
focus, set goals, identify measures, and analyze approach initiated through this learning collabo-
health outcomes. ASTHO used a comprehensive, rative is representative of the method outlined in
multi-level framework to ascertain how conditions the Institute of Medicine 2012 report on Primary
affecting policy and systems change move from Care and Public Health: Exploring Integration to
the state policy level to the community practice Improve Population Health.1
© ASSOCIATION OF STATE AND TERRITORIAL HEALTH OFFICIALS 2231 CRYSTAL DRIVE, STE 450, ARLINGTON, VACASE STUDY: ENHANCING SYSTEMS TO IMPROVE HEALTH OUTCOMES
Georgia’s Story
Georgia is a large rural state where healthcare
access varies considerably by geography, leading
to inequitable health outcomes across the state.
Georgia ranked 43 in infant
DPH performed surveillance on access to health- mortality in 2011 and 34 in 2013 in
care services in relation to infant mortality rates America’s Health Rankings.
across the state and discovered that the largest
part of the state with the highest infant mor- Georgia successfully
tality rate had no access to obstetricians. Given implemented a telehealth
the lack of access, Georgia has been engaging network in all 159 counties
with telemedicine over the last 20 years and it in Georgia.
has become one of the most widely accepted
solutions to increasing access to care across the
state. Telemedicine seeks to improve patient’s
health by permitting two-way, real time inter- The second goal was to create an external
active communication between the patient, and communications-marketing framework and plan,
the physician at the distant site. It is viewed as a encompassing all stakeholders, to outline and
cost-effective alternative to the more traditional explain the telemedicine and telehealth programs
face-to-face healthcare delivery model.2 Some to increase access and utilization of the system.
counties within Georgia had already integrated
telemedicine within their healthcare delivery Leadership and Vision
systems and were looked upon for sharing best
practices and lessons learned. Leadership and vision is defined as the extent to
which the health department’s senior leadership,
DPH acquired funding from a variety of state, including the State Health Official (SHO), provided
federal, and private sources to purchase telemed- strategic direction, aspirational goals, and
icine carts and partnered with local health depart- leadership of efforts towards the achievement of
ments to identify areas with the greatest needs measureable and sustainable outcomes.
and gaps in services to strategically deploy the
telemedicine carts. The ASTHO/UHF learning • Brenda Fitzgerald’s, MD, Georgia Department
collaborative was utilized as an opportunity to of Public Health State Health Official, support
accelerate the development of the telemedicine for the project assisted in implementing a
network across the state. Medicaid reimbursement policy change for
telemedicine services in the state of Georgia –
Georgia consists of a total of 18 health districts Medicaid grants states the option of including
encompassing a local health department and one telemedicine under their program. Prior to
or more counties within Georgia. The intention this change, a physician’s initial consult with a
of this learning collaborative was to deploy 12 patient had to be face-to-face. An exemption
telemedicine carts in rural public health clinics to by the Georgia Medical Composite Board was
allow patients with a variety of health needs to made for telemedicine consults performed by
reach healthcare providers and help DPH address a public health nurse, a public school nurse,
infant mortality, obesity, and associated diseases. the Department of Family and Children’s
Services, law enforcement, community mental
health center, or through an established childCASE STUDY: ENHANCING SYSTEMS TO IMPROVE HEALTH OUTCOMES
advocacy center, allowing physicians to consult ww The network was grassroots driven by
with patients regardless of having the initial the local health districts and counties,
in-person appointment. supported by the state.
• Dr. Fitzgerald played an integral role in facili- • “Having someone at the grassroots level who
tating agreements that defined how a public uses telemedicine daily, teaching it to other
health district would partner with private counties and sharing their success helps with
specialist providers via telemedicine after the the buy in and making it realistic vs. a state
initial meetings with county health district issue or mandate.” Suleima Salgado, Telehealth
directors and community provider groups. Director with DPH. This approach aided in
the adoption of telemedicine unique to each
• Integrating the visionary approach of including
county and health district.
public health as a provider within telemedicine
was key to aligning efforts. • DPH established a formalized partnership
with the Georgia Partnership for Telehealth,
Engaged Partners and which allowed public health departments with
telemedicine carts to access 200 additional
Meaningful Partnerships medical specialists, as needed.
Public health professionals recognize that they • Communication and planning efforts prior
cannot maximally accomplish their goals without to implementing carts at the identified sites
engaged and invested partners, collaborating were vital in assessing the clinic’s capacity and
meaningfully on work towards a shared vision garnering leadership buy-in and support.
and mission.3 Georgia strategically engaged with
partners at the local level in order to best identify
and understand the needs and capacity within
each health district. Implementer and policy
makers at all levels – from the SHO to those
doing work on the ground-engaged multi-sector “The role of telemedicine is
partnerships in meaningful work. vital to increasing access to
care in Georgia. At our health
• Georgia’s approach to building a statewide
telehealth network among a number of departments, children get
partners was successful due to DPH recog- excited seeing inside their
nizing that: mouth, ears, and throats via
ww Telemedicine was not a new concept in the telemedicine cart. We can
Georgia (especially for some rural health screen them right there in their
departments) but, most health depart-
own community or school and
ments were not aware of the increased
levels of patient engagement within then refer them to local doctors
those rural health departments. and specialist for follow up.”
ww The emerging role of public health within - BRENDA FITZGERALD, MD, STATE
telemedicine was to be viewed as a
HEALTH OFFICIAL, DPH
partner and not a competitor.CASE STUDY: ENHANCING SYSTEMS TO IMPROVE HEALTH OUTCOMES
Spread and Sustainability practices by looking to coordinate with
interpreters in other counties.
Spread and sustainability help illustrate the return
• Improvement plans are being drafted to
on investment in leveraging leadership and vision
continue expanding telemedicine into the
to engage meaningful partnerships within primary
remaining health districts with the vision to
care and public health integration work. Learning
expand to every county health department
collaboratives are intentional to increase capacity
based on needs.
within the health system at all levels. The end goal
is to foster strong partnerships within states to
allow for a more efficient delivery of resources and Results/Outcomes
healthcare services.
The Georgia Department of Public Health’s efforts
• DPH secured approximately $2 million in grant throughout the learning collaborative process led to
funding to continue to support public health a variety of systems-level improvements, including:
telemedicine programs to address infant
• DPH deploying 10 of the 12 previously
mortality, obesity, HIV/AIDS, dental health, and
purchased telemedicine carts in rural public
other issues, especially in medically under-
health clinics across the state for HIV clinics,
served areas.
Asthma-Allergy clinics, Endocrinology, Genetics,
• DPH has made proactive steps through the High-risk OB, and teledentisty.4
development of a comprehensive sustainable
• Healthcare professionals operating the
business model that will help continue
telemedicine carts with the patients utilized the
expanding on its network/infrastructure
time within the appointment to further engage
through data collection/analysis, the devel-
with patients and provide them with more
opment of management protocols, an evalu-
health education and resources—facilitating
ation kit, a marketing-communications plan,
a more patient-centered approach to care
and financial profiling.
delivery. This patient engagement opportunity
• Sustainable funding has been identified through is key to empowering patients.
the Federal Communications Commission’s
• Public health clinics seeing an increase in
(FCC) Healthcare Connect Fund that provides
patient engagement and ability to follow
reimbursements for telehealth and telemedicine
through with their appointments. The
programs serving rural communities.
telemedicine carts have allowed clinics to see
• DPH is consistently leveraging partners and more patients in a timely manner. Given the
expertise to educate state legislators on success, some clinics are beginning to utilize
the telehealth/telemedicine benefits and telemedicine for mental health consults and
on-going efforts. teledentistry.
• DPH continues to monitor telemedicine • Developing the network-enabled public
cart utilization quarterly, assess the quality health practitioners to maximize their overall
of delivery, and maintain the utility for efficiency and reach. The expansion of the
community members. telemedicine network aims to engage the
Georgia Volunteer Health Care Program
• Some clinics are beginning to integrate
(GVHCP), enlisting the help of providers willing
culturally and linguistically appropriate
to provide care via telemedicine.
standards of healthcare into their telemedicineCASE STUDY: ENHANCING SYSTEMS TO IMPROVE HEALTH OUTCOMES
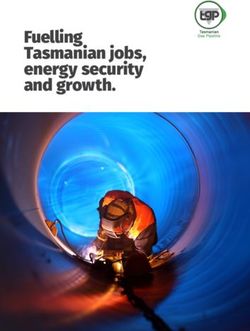
Georgia Department of Public Health Telehealth Network
Dade Fannin Rabun
Catoosa Whitfield Towns
Union
Walker 1-2
Murray Gilmer White Habersham
Telehealth Network
Lumpkin
Chattooga
Gordon Pickens Stephens
Dawson
2 Franklin
Hall Banks
Bartow Cherokee Forsyth Hart
Floyd Madison
Jackson
1-1 Fulton Clarke Elbert Teledentistry
Cobb 10
Polk DeKalb Barrow Oglethorpe
Haralson Gwinnett Telemedicine
Paulding Walton
Wilkes
Oconee
3-1 3-5 Lincoln Network Hub (Waycross)
Douglas Rockdale Newton
3-2 Taliaferro
Carroll
3-4
McDuffie Columbia End Point Locations
Henry Morgan Greene
Fayette 3-3 Warren (Video Conferencing in
Jasper Putnam
Coweta Spalding Hancock Richmond HDs & WIC Centers)
Heard Glascock
4 Butts
6
Troup Lamar Burke
Jones
Pike Baldwin Washington Jefferson
Meriwether Monroe 5-2
Upson Crawford
Talbot Johnson
Bibb Wilkinson Jenkins
Harris Emanuel Screven
Peach Twiggs 1-1 Northwest 5-1 South Central
Muscogee
7 Taylor Bleckley Laurens Treutlen
1-2 North Georgia 5-2 North Central
Houston
Marion
Schley Macon Candler Bulloch Effingham
2 North 6 East Central
Montgomery
Pulaski
5-1 3-1 Cobb/Douglas 7 West Central
Dooly
Stewart Dodge Toombs Evans Bryan Chatham 3-2 Fulton 8-1 South
Wilcox Wheeler
Webster Sumter
Telfair
Tattnall 3-3 Clayton 8-2 Southwest
Quitman Terrell
Crisp
Jeff Long 3-4 Gwinnett, Newton, & Rockdale 9-1 Coastal
Lee Ben Hill
Randolph Davis
Appling 9-1 Liberty 3-5 DeKalb 9-2 Southeast
Turner Irwin
Clay Coffee
Bacon
4 District 4 10 Northeast
Wayne McIntosh
Calhoun Dougherty Worth 9-2
Early Tift 8-1 Pierce
Baker
Berrien Brantley Glynn
Colquitt Atkinson
Cook
Mitchell
Miller 8-2 Lanier Ware Waycross
Seminole Clinch Camden
Thomas Charlton
Brooks
Decatur
Grady
Lowndes
Echols Created: December, 2014
30 0 30 By: Office of Health Indicators for Planning (OHIP)
Source: Department of Public Health
Miles Projection: Georgia Statewide Lambert Conformal Conic
Lessons Learned and • Include the following best practices and
tactics identified at the clinical level: share
Recommendations a systematic strategic plan with all stake-
DPH and its partners shared valuable lessons holders, facilitate communication regarding
learned and recommendations for other state technical needs for setting up telemedicine cart
health departments to consider when imple- placement in the clinic, and provide supportive
menting and refining a similar system. and accessible contracts from state health
departments and other county partners in
• Efficiently maximize the utility of the telemed- implementing telemedicine at new sites.
icine carts, a commitment to continual
• Focus on the community needs and build
workforce capacity building is essential.
telemedicine as an enhancement to the
Providing trainings for administering the
existing services offered within the community.
telemedicine consults are crucial in maintaining
the highest quality delivery.CASE STUDY: ENHANCING SYSTEMS TO IMPROVE HEALTH OUTCOMES
• Include all potential stakeholders (traditional
and non-traditional) in the beginning in order For more information, contact:
to collectively develop a strategic plan. Given
the variability in health needs and patient Lynn Shaull
preference among the health districts, DPH
Senior Analyst, Health Promotion &
worked with the community in devising a
Disease Prevention
tailored plan reflecting current and
emerging needs. Association of State and Territorial Health
Officials
(202) 371-9090
lshaull@astho.org
Endnotes
1 Primary Care and Public Health: Exploring Integration to Improve Population Health. Institute of Medicine.
March 2012. Available at http://www.iom.edu/Reports/2012/Primary-Care-and-Public-Health.aspx
2 Telemedicine. Medicaid.gov. Available at http://www.medicaid.gov/medicaid-chip-program-information/by-top-
ics/delivery-systems/telemedicine.html
3 Frieden. Six components necessary for effective public health program implementation. Am J Pub Health,
Published Online Ahead of Print November 14, 2013: e1-e6
4 Telehealth Map was developed by the Georgia Department of Public HealthYou can also read