Health care systems in transition: New Zealand Part I: An overview of New Zealand's health care system - Oxford ...
←
→
Page content transcription
If your browser does not render page correctly, please read the page content below
Journal of Public Health Medicine Vol. 18, No. 3, pp. 269-273
Printed in Great Britain
Health care systems in transition:
New Zealand
Part I: An overview of New Zealand's health
Downloaded from https://academic.oup.com/jpubhealth/article-abstract/18/3/269/1528742 by guest on 03 June 2020
care system
Toni Ashton
Keywords: New Zealand, health systems transition, AIDS have a lower life expectancy, lower average incomes,
higher unemployment and generally poorer health
The country and its people compared with non-Maori. Diseases such as obesity,
cardiovascular disease and the complications of
New Zealand is located in the south-west Pacific Ocean, diabetes mellitus all occur more frequently amongst
about 2000 km off the south-east coast of Australia. both Maori and Pacific Islanders compared with the
The country comprises two main islands plus a number rest of the population.2
of smaller islands with a combined land area similar Central to New Zealand's constitutional history is
to that of the United Kingdom. Of the 3-6 million the Treaty of Waitangi, signed in 1840 between some
inhabitants, 80 per cent of the population is of Maori tribes and the British Crown, in which Maori
European descent, predominantly British or Irish; the people ceded sovereignty to the Crown in exchange for
indigenous Maori people and their descendants make the guaranteed protection of their lands, forests,
up about 13 per cent of the population, and Pacific fisheries and cultural treasures, and the rights and
Island Polynesians with 4 per cent of the population privileges reserved for British subjects. It is widely
comprise the third largest ethnic group.' A recent wave accepted that the Treaty has not been honoured and
of immigration from Asian countries is, however, that Maori ownership, rights and privileges have been
rapidly reshaping the ethnic mix in some areas. steadily undermined. Recent efforts by the Government
Although New Zealand is often perceived to be a are slowly beginning to redress past grievances, and the
rural country - possibly owing to the historical Treaty is now central to race relations and to issues
dominance of the agricultural sector in the economy affecting the social and economic position of Maori,
- 80 per cent of the population now lives in urban including the health system.
areas, with 50 per cent concentrated in the four main Since the mid-1980s, the Government has imple-
cities. The rural population is widely dispersed. mented a programme of rapid and significant economic
Although many fanning areas are relatively affluent, and social reform, with a general trend towards a
other rural areas - particularly those with a high greater reliance on market mechanisms. Major initia-
proportion of Maori - are characterized by unemploy- tives have included the removal of industrial and export
ment, poor housing and poverty. subsidies and the deregulation of industry, the restruc-
European settlement from the late eighteenth century turing of government departments, the reduction in
had a devastating effect on the health of the Maori and narrower focusing of welfare benefits and access to
population. Infectious diseases - such as typhoid, government-funded services, and the corporatization
tuberculosis and venereal diseases took their toll, as
did the introduction of alcohol and firearms. In spite of Department of Community Health, School of Medicine, University of
a recent narrowing in socio-economic and health status Auckland, Private Bag 92 019, Auckland, New Zealand
differentials between Maori and non-Maori, Maori still TONI ASHTON, Senior Lecturer in Health Economics
© Oxford University Press 1996270 JOURNAL OF PUBLIC HEALTH MEDICINE
and privatization of state trading departments. The Eligibility for the higher subsidy levels was also
increased emphasis on market-based service provision extended to include more low-income families. In
also encouraged the restructuring of other government- spite of these adjustments, anecdotal evidence suggests
funded services in the early 1990s, including housing, that the new financial regime has failed to overcome
education and the health system. problems of financial barriers governing access to
primary care for low-income groups.
The New Zealand health care system: an Most primary services are delivered by general
practitioners (GPs), who act as gate keepers to the
overview
public hospital system and the use of other subsidized
The New Zealand health care system is predominantly health services such as laboratory tests, Pharmaceuticals,
Downloaded from https://academic.oup.com/jpubhealth/article-abstract/18/3/269/1528742 by guest on 03 June 2020
(77 per cent) publicly funded,3 with around 91 per cent physiotherapy and diagnostic imaging. A range of
of this public funding raised through general taxation. allied health professionals and voluntary organizations
Although there is no special social insurance levy, also provide primary health services, including mid-
funding for accident-related injuries is raised separately wives, independent nurse practitioners, public health
through a compulsory state-run insurance scheme. nurses and the Plunket Society, which provides child
Most private funding is out-of-pocket payments. health care.
Almost half of the population have some private A network of state-owned hospitals provides around
health insurance but this accounts for only 6 per cent 20 000 general, psychiatric and maternity beds (i.e. 5-6
of total health expenditure. Private health insurance beds per 1000 population).4 In addition, there are
does not provide comprehensive cover and is most around 7000 private hospital beds, more than 75 per
commonly used to claim reimbursement for primary cent of which are geriatric or long-stay beds where
care user charges, elective surgery in private hospitals patients are eligible for income- and asset-tested
and specialist out-patient consultations. Total expen- government subsidies. The remaining private hospital
diture has increased only marginally over the last beds are used primarily for privately funded elective
decade although the proportion funded by the state has surgery. Doctors and other health professionals work-
been falling gradually. ing in public hospitals are salaried. Most specialists also
Since the Social Security Act of 1938, separate work part time as private consultants on a fee-for-
funding and development of primary and hospital- service basis.
based services has existed. The original intention of the
1938 Labour Government had been to provide health
Recent changes
services free at point of delivery for all subjects,
regardless of income. However, opposition from the From July 1993, the public health system was
medical profession resulted in the development of restructured in line with the market-oriented reforms
privately owned fee-for-service primary medical services, that had been introduced in the wider economy. The
with varying levels of subsidization, operating alongside central features of this restructuring process were the
a fully subsidized and government-owned public hospi- separation of the purchaser and provider roles - both
tal service. Although this general structure still largely of which had previously been undertaken by 14 area
remains in place, changes are currently taking place. health boards - and the reconfiguration of public
In 1992 a new regime of subsidies and user charges hospitals into more business-like structures. The
for health services was introduced. The primary general tax-based financing arrangements, however,
objective was to improve access for low-income remained unchanged.
groups by moving away from universal subsidies to a Four regional health authorities (RHAs) were set up
more directed regime. User charges were introduced for to purchase all primary, secondary and tertiary health
public hospital services for higher-income groups and services, including disability support services. In effect,
subsidies for general practice services for higher-income this means that all government funding for personal
adults were withdrawn entirely. The main group to health services is now integrated into a single budget
benefit from the changes was low-income working and that this budget is capped, including the previously
adults. Welfare beneficiaries were also marginally open-ended fee-for-service primary care payments. The
better off. A number of adjustments have since been 14 area health boards werereconfiguredinto 23 crown
made to this new user-charge regime. Most signifi- health enterprises (CHEs) which enter into contracts
cantly, the charges for in-patient hospital services were with RHAs to provide services alongside private
removed just 13 months after they had been introduced, hospitals or other private providers. CHEs, like NHS
largely because of strong public opposition, whereas trusts in the United Kingdom, are independent business
charges for out-patient services have been retained. entities, governed by a government-appointed board ofNEW ZEALAND'S HEALTH CARE SYSTEM 271
directors. Under the legislation, CHEs are required to disease prevention. Public health services have had a
act as successful and efficient businesses while exhibiting chequered history in recent years. Before 1983, they
a sense of social responsibility.6 A National Advisory were centrally funded and organized by the Department
Committee on Core Health and Disability Support of Health through a network of regional offices. The
Services (now known as the National Health Com- Area Health Boards Act of 1983 provided for the
mittee) was established to advise the Minister of Health decentralization of these services to the 14 area health
which personal health services should be purchased by boards which were established progressively between
the RHAs. 1983 and 1989. By 1989, the organization and provision
Negotiations are currently under way between RHAs of public health services had been decentralized
Downloaded from https://academic.oup.com/jpubhealth/article-abstract/18/3/269/1528742 by guest on 03 June 2020
and GPs and other primary care providers to develop although the Department of Health retained a regula-
mechanisms for purchasing primary care services. Many tory function.
GPs have joined umbrella groups called Independent In 1993, public health services were effectively
Practitioner Associations (IPAs) to negotiate contracts. recentralized as part of the most recent reforms. The
Some of these groups, which range in size up to 300 original proposal was to apply the purchaser-provider
members, have become budget holders for pharma- model through the establishment of an independent
ceuticals or laboratory tests. As RHA budgets are Public Health Commission (PHC), which would co-
capped, many GPs are anticipating a move away from ordinate and purchase public health services, and a
the current fee-for-service form of government subsidy Public Health Agency, which would be the major
towards capitation payments. However, some IPAs provider of regionally based public health services. In
strongly support the continuation of fee-for-service the event, only the PHC was established. Its role was to
payments for general practice services. Regardless of provide policy advice to the Minister and to purchase
how the public subsidy component is paid to GPs, public health services. The PHC contracted for services
patient user charges are likely to remain in place for directly with independent service providers and indir-
general practice services and Pharmaceuticals. ectly with CHEs via RHAs.
Separate arrangements have been established for the During the first year after the reforms were enacted
provision of public health services - population-based and implemented, a number of problems emerged.
services such as health education, promotion and Confusion existed concerning the conflicting roles of
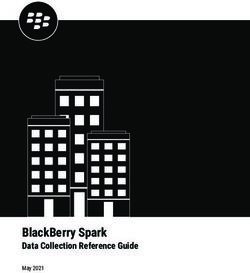
MINISTERS
National Advuoty Committee on
ADVISORS Core Contracts
Health and Disability Support Advice
Services' Monitoring
PURCHASERS
PROVIDERS
FIGURE 1 The structure of the health care system in New Zealand after recent modifications. 1 Now known as the National
Health Committee, includes independent GPs, IPAs, a range of non-GP primary care providers, and diagnostic and
pharmacy services, includes rest homes, home support services, and a range of services provided by voluntary
organizations.272 JOURNAL OF PUBLIC HEALTH MEDICINE
the PHC as an independent policy advisor while being compete for contracts, for most services competitive
part and parcel of central government. There was also purchasing has been minimal to date. Incumbent
confusion about overlapping responsibilities and lines providers have usually been awarded contracts and
of accountability of the PHC and the Ministry of few private hospitals have been successful in their
Health, previously known as the Department of Health. bids.'0 In part, this is because RHAs were required to
Service delivery problems arose as a result of poor purchase the same type and level of services in the first
service specification and of the unclear boundaries of year to smooth the transition to the new system. It may
responsibility between different government agents. It also be because RHAs do not have sufficient informa-
was also apparent that the Government sometimes felt tion to make informed comparisons between the
Downloaded from https://academic.oup.com/jpubhealth/article-abstract/18/3/269/1528742 by guest on 03 June 2020
uncomfortable with some of the issues raised by the quality, cost and efficiency of services offered by
PHC. For example, the PHC was critical of poor alternative providers. Costings remain crude and
housing conditions which could be traced directly to there is no standard method for case-mix adjustment
changes in government housing policy. After some brief for hospitals.
consultation with interested parties, the PHC was On a more positive note, the contracting process
abolished on 30 June 1995. Its roles are now under- itself has improved the accountability of providers and
taken by a public health unit located within the is encouraging the development of better information
Ministry of Health. The structure which has emerged about the volume, quality and cost of services. The
following these and a number of other modifications to reforms have also opened up a number of opportunities
the original reformed structure is depicted in Fig. 1. which have yet to be developed to their full potential. In
particular, the integration of funding for all personal
health and disability support services opens up the
Analysis of the 1993 reforms and future
opportunity to provide a more integrated health service
developments and to improve efficiency and effectiveness by shifting
It is too early to make any overall judgement about the resources across services and service providers. It
effect that the reforms have had either on the is expected that the RHAs will move towards the
effectiveness or efficiency of health service provision development of more co-ordinated care through
or the health status of the population. Before the the expansion of various types of budget-holding
reforms, throughput of surgical services had been arrangements.8
steadily increasing, and waiting lists also continued to Changes are also occurring with respect to services
increase; both of these trends have continued since the for Maori. Maori have consistently sought to gain
changes were introduced. Improved transparency of autonomy in health services based upon constitutional
the CHEs' accounting systems has revealed that many equity arising from the Treaty of Waitangi." Although
of them are infinancialdifficulties and the Government such autonomy remains little more than a dream,
has had to inject additional funds into the CHEs. the new structure has opened up both dialogue and
Nevertheless, a number are closing or reducing services, opportunities for Maori to gain better access to
especially relating to rural hospitals, and some have and control of health resources. For example, one
reduced staff numbers significantly. For the public, RHA has negotiated a joint venture with Maori groups
perceptions of the success of the reforms so far are to jointly purchase services. New community based
probably derived mostly from commentaries in the health groups which provide more acceptable and
media, most of which tend to focus on negative aspects appropriate services for Maori are also slowly devel-
such as hospital closures and waiting lists. From the oping. Nevertheless, some commentators are of the
patient's perspective, most services remain largely opinion that autonomy cannot be achieved unless a
unchanged. separate Maori Health Authority with its own budget
To date, the focus of evaluation has been on the to purchase health services for Maori is established
process itself rather than on the outcome of the reforms alongside the four RHAs."
in terms of health indices. It is clear that the process A major concern of the reformed health care system
itself has been more complicated, has required more in New Zealand is a lack of overall planning for the
modifications and has been more costly to implement future. The focus of both the advisory committee on
than originally envisaged.4 This applies especially to core services and the RHAs is currently on trying to
public health services, where continuous restructuring establish service priorities. Questions revolve around
has undermined staff morale and resulted in confusion what services should be purchased today, rather than
and fragmentation of service provision. what services are likely to be required in future years.
Although the structure for personal health services The structure of New Zealand's population is
was based upon the notion that providers would expected to change rapidly over the next 25 years.NEW ZEALAND'S HEALTH CARE SYSTEM 273
Whereas the European population is ageing as the difficulty is that, as yet, the advisory committee on core
'baby-boomers' of the 1950s are approaching retire- services has been unable to provide RHAs with
ment age, around 60 per cent of the Maori and Pacific guidelines on what services they should purchase.
Island population are less than 25 years old. This Until there is some clarification both of the minimum
clearly has major implications for future service level of services to be provided and the cost of these
needs. services, there is a danger that cost containment will be
There is also a lack of planning with respect to achieved at the expense of reasonable access to health
routine implementation of new technology. RHAs are services by the population.
concerned with securing services which meet the health
Downloaded from https://academic.oup.com/jpubhealth/article-abstract/18/3/269/1528742 by guest on 03 June 2020
needs of their population. This gives CHEs and other
service providers considerable choice as to how their References
services are provided, and evidence of the unnecessary
1
duplication of technology is already beginning to Department of Statistics. 1991 census of population and
emerge. In contrast, there is tight control over the dwellings: national summary. Wellington: Department of
Statistics, 1992.
subsidy on both existing and new drugs. The four Laugeson M, Salmond C. New Zealand health care: a
RHAs have set up a joint venture company which background. Health Policy 1994; 29: 11-23.
3
decides which drugs should be listed on the pharma- Muthumala D, Howard P. Health expenditure in New
ceutical schedule and the price the Government will Zealand 1980-1994. Wellington: Performance Monitoring
and Review Unit, Ministry of Health, 1995.
pay. As a monopoly purchaser, this company has 4
Scott C. Reform of the New Zealand health care system.
strong bargaining power. However, it appears that the Health Policy 1994; 29: 25-40
primary objective is cost containment of the drug Upton S. Your health and the public health, a statement of
budget rather than efficiency in its use.12 Little government policy. Wellington: Ministry of Health, 1991.
6
emphasis seems to be placed on the overall cost- Ministry of Health. Health and Disability Services Act,
Section 11. Wellington: Ministry of Health, 1993.
effectiveness of drugs, or on the possibility that 7
Ministry of Health. Postelection briefing, Vol. 1. Wellington:
increased expenditure on drugs could reduce treatment Ministry of Health, 1993.
costs elsewhere. 8
Ashton T. The purchaser/provider split in New Zealand:
the story so far. Aust Hlth Rev 1995; 18: 43-60.
Containment of health care expenditure has in the 9
Public Health Association. Shackled by the contracting
past not been an overt concern in New Zealand. chain: a review of the purchase and delivery of public
Nevertheless, before the reforms it was clear that cost health services. Unpublished Discussion Paper, December
containment was being achieved only by tight control 10
1994.
of expenditure on public hospitals. Real expenditure on Performance Monitoring and Review. Review of 1994/95
RHA contracting. Wellington: Ministry of Health, 1995.
public hospitals was declining, capital was not being " Laing P, Pomare E. Maori health and the health care
maintained and debts were mounting. In contrast, reforms. Health Policy 1994; 29: 143-156.
expenditure on primary health care was increasing at an 12
Pharmaceutical Management Agency Ltd. PHARMAC -
average rate of 6 per cent per year. The integration of the first 20 months. Wellington: Pharmaceutical Manage-
primary care into RHA budgets means that contain- ment Agency Ltd., 1995.
ment of public expenditure should be achieved if both
RHAs and CHEs can remain within their budgets. The Accepted on 2 April 1996You can also read