Intramuscular triamcinolone acetonide in chronic
←
→
Page content transcription
If your browser does not render page correctly, please read the page content below
Downloaded from http://thorax.bmj.com/ on January 22, 2015 - Published by group.bmj.com
Thorax 1985;40: 840-845
Intramuscular triamcinolone acetonide in chronic
severe asthma
DT McLEOD, SJ CAPEWELL, JENNIFER LAW, W MAcLAREN, A SEATON
From the Chest Unit, City Hospital, and Institute of Occupational Medicine, Edinburgh
ABSTRACT, Seventeen subjects with chronic severe asthma completed a 48 week prospective,
double blind study with crossover of treatment at 24 weeks, in which triamcinolone acetonide
80 mg intramuscularly every four weeks was compared with oral prednisolone 10 mg daily.
Spirometry, twice daily measurements of peak expiratory flow rate, and self assessment of asthma
symptom scores showed significant improvement during triamcinolone treatment; less extra pred-
nisolone was required and there was significant weight loss. Two patients withdrew, one because
of dissatisfaction with prednisolone and one because of side effects while taking triamcinolone.
Three were withdrawn, one with proximal muscle weakness and two because of intercurrent
illness. Adrenal suppression, bruising, and hirsuitism were worse with triamcinolone, other side
effects being comparable. On completion of the study 16 of the 17 patients opted to continue
taking triamcinolone acetonide. This treatment is an important addition to the therapeutic
options available for chronic severe asthma.
The introduction of corticosteroids revolutionised Methods
the treatment of asthma in the 1950s' and inhaled
corticosteroids subsequently produced further sub- Twenty two patients agreed to take part in the study.
stantial benefits for many asthmatics by reducing or All had longstanding asthma and had previously
abolishing the need for regular oral corticosteroid shown considerable variability in ventilatory func-
treatment.2 Some asthmatic patients continue to tion spontaneously and at least 20% improvement
have symptoms with persistently poor ventilatory in FEV, with corticosteroid treatment. All had
function despite continuous oral corticosteroid required a minimum of 10 mg oral prednisolone
treatment. These patients are frequently much dis- daily for several years as well as inhaled bec-
abled by their disease and improve appreciably lomethasone 400 ,ug daily; with this combination all
only with unacceptably high doses of corticosteroids. had peak flow rates less than 70% of predicted.
They therefore pose both a therapeutic dilemma and None had suffered an exacerbation of symptoms or
an important challenge in asthma research. had needed to increase the dose of prednisolone in
We have treated such patients with intramuscular the four weeks before entering the study.
triamcinolone acetonide for some years and have All patients gave written consent and the study
formed the impression that this often has consider- protocol was approved by the local ethical commit-
able advantages for the patient, a suggestion sup- tee. Patients were instructed in the completion of a
ported by two previous studies.34 To confirm this, diary card, recording twice daily peak flow rate (best
we selected patients with chronic severe asthma who of three blows), day and night symptom scores (from
required at least 10 mg of prednisolone as daily 0 = "no symptoms" to 4 = "symptoms requiring
maintenance treatment in addition to inhaled emergency treatment"'), extra treatment required,
corticosteroids, and compared monthly intramuscu- and any other comments. They were examined
lar triamcinolone acetonide with daily oral pred- every four weeks with measurement of FEV, FVC,
nisolone in a study using objective measurements weight, and blood pressure; urine analysis; and fun-
and diary card assessment. doscopy. Proximal muscle weakness was tested by
Address for reprint requests: Dr A Seaton, Institute of Occupa-
asking the patient to stand upright from the squat-
tional Medicine, Edinburgh EH8 9SU. ting position five times in quick succession. Cushin-
goid appearance, bruising, and peripheral oedema
Accepted 29 April 198S were scored in terms of severity on a five point scale.
840Downloaded from http://thorax.bmj.com/ on January 22, 2015 - Published by group.bmj.com
Intramuscular triamcinolone acetonide in chronic severe asthma 841
In addition, on entry and at 12, 24, 36, and 48 weeks both the " triar' and the " active" bottles were
a full blood count was done and concentrations of counted.
electrolytes, urea, calcium, phoshate, and alkaline The data were entered into a Prime 750 compu-
phosphatase were checked. A short tetracosactrin ter. Statistical methods were primarily descriptive,
test (250 ,g given by intramuscular injection with paired t tests being used to test the significance of
plasma cortisol recorded at 0 and 30 minutes) was any differences observed.
performed on entry and at the end of each 24 week
period of treatment. Results
We used a 48 week double blind, placebo control-
led study design, with crossover of treatment after Twenty two subjects, 15 men and seven women
24 weeks. Active treatment-triamcinolone (mean age 56 years, range 23-71) started the study.
acetonide 80 mg intramuscularly every four weeks Two smoked 10 cigarettes daily and three were
or prednisolone 10 mg orally each day-was given ex-smokers. Three were withdrawn from the study:
to all patients along with the corresponding placebo one suffered a myocardial infarct 20 weeks after
tablets or placebo injections. Patients were ran- starting the study; one died of bronchial carcinoma,
domly allocated in equal numbers to the initial which was diagnosed at 28 weeks; and one noted
active treatment and instructed to take their trial increasing proximal muscle weakness at 40 weeks
tablets early each morning. After the 48 weeks all (16 weeks after starting triamcinolone). Two others
subjects were asked to state whether they preferred withdrew, one because of no improvement after
the first or second 24 week treatment period, after eight weeks of prednisolone and one because of
which the code was broken. weight loss and muscle weakness after 12 weeks of
Subjects were instructed to treat an exacerbation triamcinolone. Thus 17 subjects completed the
during the trial by taking extra prednisolone, 20 study but sufficient data were collected on the
mg/day for at least five days, and then reduce it in patient who completed 40 weeks to permit his inclu-
their usual way. All were supplied with labelled sion in the analysis.
active prednisolone for this purpose. Other treat-
ment, such as inhaled or oral sympathomimetics, PEAK FLOW RATES: DIFFERENCES BETWEEN
was continued unchanged throughout the study. All TREATMENTS
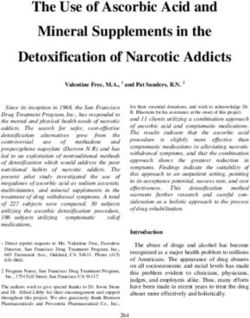
changes in treatment were recorded on the diary The mean results of the peak flow recordings are
cards and at each clinic visit the remaining tablets in shown in the figure. The patients who started with
_.- PM TRIAMCINOLONE FIRST
- - -- -AM TRIAMCINOLONE FIRST
- PREDNISOLONE FIRST
- PM
350 r- -APM PREDNISOLONE FIRST
330 I
/ 0000,
PEAK
310 _-
FLOW
RATE 290
(I.min )
270
250 1-
230 _-
L 1 2 3 4 5 6 7 8 9 10 11 12
MONTHS FROM START OF TRIAL
Mean peak flow rates recorded morning and evening through the trial. Continuous lines
represent subjects who received triamcinolone for the first six months and interrupted lines those
who received prednisolone first.Downloaded from http://thorax.bmj.com/ on January 22, 2015 - Published by group.bmj.com 842 McCleod, Capewell, Law, MacLaren, Seaton triamcinolone had higher average peak flows at the Table 2 Peak flow rates with triamcinolone for months I start of the study (mean values 288 versus 250 1 and 2 compared with months 4 and 5 for 18 patients (mean min-'). This was a chance difference and did not affect values with standard deviations in parentheses) the analysis as each patient was compared with him- Peak flow rate (I min - ') self or herself on the second treatment. Those sub- jects receiving triamcinolone had consistently higher Months I and 2 Months 4 and 5 p value readings than those receiving prednisolone through- Morning 280 (69.7) 297 (75.9)
Downloaded from http://thorax.bmj.com/ on January 22, 2015 - Published by group.bmj.com
Intramuscular triamcinolone acetonide in chronic severe asthma 843
Table 3 Peak flow rate values (1 min-') for 18 patents: second versus fourth week duing each four week cycle (mean
values with standard deviations in parentheses)
Triamcinolone Prednisolone
Week 2 Week 4 p Week 2 Week 4 p
Morning 277 (81.9) 266 (7X.3)Downloaded from http://thorax.bmj.com/ on January 22, 2015 - Published by group.bmj.com
844 McCleod, Capewell, Law, MacLaren, Seaton
Table 6 Numbers ofpatients developing side effects not a new idea. Methyl prednisolone acetate given
every two weeks has been shown to lessen the over-
Side effect Triamcinolone Prednisolone all severity of asthma symptoms.9 This intermittent
Bruising high dose "pulse" corticosteroid treatment has been
Armsandhands 10 10 shown in other diseases to alter alveolar mac-
Shins 4* 1
Muscle weakness 2 0 rophage function in a dose dependent fashion,
Muscle pain 6 4 decrease the level of immune complexes, alter alveo-
Ankle oedema (intermittent) 3 2
Facial hirsuitism 3 1 lar macrophage function, and reduce the number of
Increased Cushingoid neutrophils in the lung,'0 yet even in high dosage is
appearance 3 7 remarkably safe. After the injection of triam-
*There was more pretibial bruising with triamcinolone. cinolone acetonide the peak plasma concentration is
achieved within three to 48 hours, after which there
acetonide every 28 days, equivalent to 2.86 mg/day, is a steady decline until the drug is virtually unde-
is more effective than 10 mg of prednisolone daily.34 tectable in plasma after 21 days." Thus clinical
This suggests that triamcinolone acetonide is more activity, while being reduced somewhat in the fourth
potent in terms of its effect on the airways, though week, lasts much longer than the period during
not necessarily so in respect of systemic side effects which the drug is detectable. Monthly injection of
and adrenal suppression. Such a view is supported triamcinolone acetonide is, in essence, a form of
by a study in which significantly less adrenal sup- such "pulse" treatment with high plasma concentra-
pression was noted with triamcinolone acetonide4 tions, particularly in the first week. This may be one
and by another in which no greater suppression was of its antiasthma mechanisms.
found after two years' treatment with triamcinolone The relative potency of different corticosteroids is
acetonide.3 Our finding of greater adrenal suppres- clearly important in interpretation of our results.
sion with triamcinolone acetonide may be due to our Cautious interpretation is required, as estimation of
studying an older age group with more severely potency depends not only on the animal model but
impaired adrenals before entry, as a result of previ- also on the target organ or tissue tested and the
ous prolonged prednisolone treatment. Others, route of administration. Experiments on rats or
using 60 mg intramuscularly every four to six weeks, mice, species sensitive to corticosteroids, may bear
have found that adrenal recovery occurs before the no relationship to what occurs in man, with his rela-
next injection in half of the patients.56 To judge by tive resistance to corticosteroids. More than 20
experience from the disciplines of dermatology and years ago modified corticosteroids with unusually
rheumatology, where triamcinolone acetonide high topical potency on human skin were developed
40-60 mg every four to six weeks has been used by forming 16,17-acetonides or by esterification at
widely, major side effects have been remarkably the 17 or 21 position (or both). By this means the
few.7 Menstrual irregularities in half of the pre- topical anti-inflammatory activity 'was much
menopausal women have been reported, resulting increased while the systemic glucocorticoid effects
from altered levels of gonadotrophins and ovarian were little changed. A vasoconstriction assay on
hormones.8 Patients tend to lose weight, not always human skin using alcohol solutions of cortico-
a bad thing in chronic asthmatics, perhaps because steroids under occlusive dressings showed that the
of loss of fat or less salt and water retention; the relative topical potency of dexamethasone to triam-
possibility of subclinical myopathy remains specula- cinolone acetonide to beclomethasone dipropionate
tive. Blood glucose and electrolyte concentrations was 0.8:100:500.12 Given intravenously, however,
are unaffected. In our wider experience outside this beclomethasone dipropionate was equivalent to
study, proximal myopathy occurs in about 5% but dexamethasone in lowering cortisol (implying a simi-
this complication should not be exaggerated, being lar systemic glucocorticoid effect). While triam-
easily detected and reversible. Bruising is more not- cinolone acetonide is about 100 times more potent
able, particularly in those over 60 years of age.7 The than dexamethasone on human skin, its relative
risk of osteoporosis has not been assessed and merits potency with respect to reduction of plasma cortisol
further study. Long term side effects may be further does not appear to have been investigated.
reduced by using triamcinolone acetonide judici- One of the actions of corticosteroids leads to the
ously. It may be possible in individual patients to synthesis of a factor that blocks phospholipase A2,
reduce the injection dose as well as to extend the thus preventing the biosynthesis of a whole cascade
interval between injections from four to six or even of lipid mediators.'3 The potency of this inhibition
eight weeks. closely parallels anti-inflammatory activity. If there-
Transferring asthmatic patients from oral to fore a local anti-inflammatory effect within the air-
parenteral long acting corticosteroid treatment is way were a critical factor in the unique efficacy ofDownloaded from http://thorax.bmj.com/ on January 22, 2015 - Published by group.bmj.com
Intramuscular triamcinolone acetonide in chronic severe asthma 845
corticosteroids in asthma, and if this effect within corticosteroid-resistant asthma. Br J Dis Chest 1979;
the bronchial mucosa were relatively greater than 73:39-44.
the systemic glucocorticoid effect, the benefits 4 Willey RF, Fergusson RJ, Godden DJ, Crompton GK,
would outweigh potential side effects. Grant IWB. Comparison of oral prednisolone and
intramuscular deport triamcinolone in patients with
Most patients with asthma respond to pred- severe chronic asthma. Thorax 1984;39:340-4.
nisolone and we see no reason for changing the 5 Mikhail GR, Sweet LC, Mellinger RC. Parenteral
general use of this well tried drug. Growing aware- long-acting corticosteroids: effect on hypothalamic-
ness of the problem of steroid resistant patients,'4 pituitary-adrenal function. Ann Allergy 1973;
however, raises the possibility that individual varia- 6 31: 337-43. Lech
tion in steroid cell membrane receptors may also Droszcz W, B, Malunowicz E, Piotrowska B. Fac-
tors influencing adrenocortical suppression during
alter the clinical response. Triamcinolone acetonide, long-term triamcinolone acetonide therapy in asthma.
for reasons still poorly understood, appears to offer Ann Allergy 1980;44: 174-6.
a valuable alternative to prednisolone in chronic 7 Arnold HL. Safer long-term steroid therapy with
severe asthma. It has the advantage of guaranteed injected triamcinolone acetonide. Int J Dermatol
1978; 17:216-7.
compliance and it appears to be acceptable to most 8 Carson
of our patients. TE, Daane TA, Weinstein RL. Long-term
intramuscular administration of triamcinolone
acetonide. Arch Dermatol 1975; 111: 1585-7.
We are most grateful to Catherine McLennan, 9 Nash J, Jacomb RG. Corticosteroid therapy in chronic
Morag McVittie, and ABH Hunter from the City asthma. Practitioner 1968;201: 358-61.
Hospital, Edinburgh; R Murdoch from the Institute 10 Keogh TA, Bernardo J, Hunninghake GW, Price DL,
of Occupational Medicine; Dr PH Lacey of Pfizer Crystal RG. Effect of intermittent high dose parenteral
corticosteroids on the alveolitis of idiopathic pulmo-
Ltd; and P Woods of ER Squibb and Sons Ltd; and nary fibrosis. Am Rev Respir Dis 1983; 127:18-22.
to Joyce Holywell and Elizabeth Crolla for typing 11 Kusama M, Sakauchi N, Kumaoka S. Studies of plasma
the manuscript. Dr Peter Howard gave us the origi- levels and urinary excretion after intramuscular injec-
nal idea. tion of triamcinolone acetonide. Metabolism 1971;
20:590-6.
12 Harris DM. Some properties of beclomethasone di-
References proprionate and related steroids in man. Postgrad Med J
1975;51,suppl 4:20-5.
1 Walsh SD, Grant IWB. Corticosteroids in treatment of 13 Flower RJ, Blackwell GJ. Anti-inflammatory steroids
chronic asthma. Br Med J 1966;ii: 796-802. induce biosynthesis of a phospholipase A2 inhibitor
2 British Thoracic and Tuberculosis Association. Inhaled which prevents prostaglandin generation. Nature
corticosteroids compared with oral prednisolone in 1979;278:456-9.
patients starting long-term corticosteroid therapy for 14 Carmichael J, Paterson IC, Diaz P, Crompton GK, Kay
asthma. Lancet 1975;ii:469-73. AB, Grant IWB. Corticosteroid resistance in chronic
3 Peake MD, Cayton RM, Howard P. Triamcinolone in asthma. Br Med J 1981;282: 1419-22.Downloaded from http://thorax.bmj.com/ on January 22, 2015 - Published by group.bmj.com
Intramuscular triamcinolone
acetonide in chronic severe
asthma.
D T McLeod, S J Capewell, J Law, W MacLaren and A
Seaton
Thorax 1985 40: 840-845
doi: 10.1136/thx.40.11.840
Updated information and services can be found at:
http://thorax.bmj.com/content/40/11/840
Email alerting Receive free email alerts when new articles cite this
service article. Sign up in the box at the top right corner of the
online article.
Notes
To request permissions go to:
http://group.bmj.com/group/rights-licensing/permissions
To order reprints go to:
http://journals.bmj.com/cgi/reprintform
To subscribe to BMJ go to:
http://group.bmj.com/subscribe/You can also read