Is There Hardening of the Heart During Medical School?
←
→
Page content transcription
If your browser does not render page correctly, please read the page content below
Physician–Patient Relationship
Is There Hardening of the Heart During
Medical School?
Bruce W. Newton, PhD, Laurie Barber, MD, James Clardy, MD, Elton Cleveland, MD,
and Patricia O’Sullivan, EdD
Abstract
Purpose obstetrics– gynecology, pediatrics, but the scores of women choosing
To determine whether vicarious empathy and psychiatry) or noncore (all other noncore careers fell below those of the
(i.e., to have a visceral empathic specialties). norms by their second year.
response, versus role-playing empathy)
decreases, and whether students Results
Vicarious empathy significantly decreased Conclusions
choosing specialties with greater patient
during medical education (P ⬍ .001), The findings suggest that undergraduate
contact maintain vicarious empathy
especially after the first and third years. medical education may be a major
better than do students choosing
specialties with less patient contact. Students choosing core careers had determinant differentially affecting the
higher empathy than did those choosing vicarious empathy of students on the
Method noncore careers. Men choosing core basis of gender and/or specialty choice.
The Balanced Emotional Empathy Scale careers initially had empathy exceeding The greatest impact occurred in men
was administered at the beginning of population norms, but their empathy fell who chose noncore specialties. The
each academic year at the University of to be comparable with that of norms by significant decrease in vicarious empathy
Arkansas for Medical Sciences for four the end of their third year. The empathy is of concern, because empathy is crucial
classes, 2001–2004. Students also of men choosing noncore careers was for a successful physician–patient
reported their gender and specialty comparable with that of norms. Women relationship.
choice. Specialty choice was classified as choosing core careers had empathy
core (internal medicine, family medicine, scores comparable with those of norms, Acad Med. 2008; 83:244–249.
Medical professionalism is essential have shown that medical school can often individual’s ability to imaginatively take
for maintaining the integrity of the have a detrimental effect on certain the role of another so as to understand
profession, and it includes demonstrating aspects of students’ professional growth. and accurately predict that person’s
compassion, caring, and a willingness to Negative characteristics such as cynicism thoughts, feelings and actions.6 The first
put the concerns of patient and society may increase, and ethical and moral definition reflects an innate emotional
above one’s own. Medical education development can be stunted.1–3 response, that is, a “gut reaction,” and is
should promote the development of these equivalent to the “empathic concern”
professional qualities. However, studies Empathy is one of the most highly described by Davis7; the second
desirable professional traits that medical definition refers to “cognitive” empathy
education should promote, because and reflects a learned ability to imagine
Dr. Newton is associate professor of neurobiology empathic communication skills promote and intellectualize.7
and developmental sciences, and associate dean for patient satisfaction and adherence to
undergraduate medical education, University of treatment plans while decreasing the Many scales that measure empathy are
Arkansas for Medical Sciences, Little Rock, Arkansas.
likelihood of malpractice suits.4,5 Patients investigating cognitive empathy of
Dr. Barber is professor of ophthalmology, view physicians who possess the quality individuals to “role-play.”8 Previous data
University of Arkansas for Medical Sciences, Little of emotional empathy as being better concerning medical students’ cognitive
Rock, Arkansas.
caregivers. A physician may possess empathy are conflicting, indicating either
Dr. Clardy is professor of psychiatry, and associate competent diagnostic skills, yet be no changes, decreases, or increases in
dean for graduate medical education, University of
Arkansas for Medical Sciences, Little Rock, Arkansas.
considered by patients as “ineffective” empathy during undergraduate medical
because the physician misses the link training.9 –13 In our previous cross-
Dr. Cleveland is associate professor of family
medicine and pediatrics, University of Arkansas for
between patient satisfaction, adherence to sectional study, we observed a decline in
Medical Sciences, Little Rock, Arkansas. medical instructions, and physician vicarious empathy during medical
empathy. school.14 There are no known longitudinal
Dr. O’Sullivan is professor of medicine, and
associate director of educational research, University studies of vicarious empathy. In the
of California at San Francisco, San Francisco, Sociologists and psychologists have current study, we examined the
California. divided the concept of empathy into two longitudinal effect of medical education
Correspondence should be addressed to Dr. Newton, main definitions or types: vicarious and on vicarious empathy.
College of Medicine, Academic Affairs, #603, imaginative. Vicarious empathy is “an
University of Arkansas for Medical Sciences, 4301 W. individual’s vicarious emotional response Previous studies suggest that certain
Markham St., Little Rock, AR 72205; telephone:
(501) 686-7407; fax: (501) 686-8160; e-mail: to perceived emotional experiences of measures of a medical student’s
(newtonbrucew@uams.edu). others” and imaginative empathy is “an personality may predict whether the
244 Academic Medicine, Vol. 83, No. 3 / March 2008Physician–Patient Relationship
student will enter one of five core Specialty choice. We classified each The percentages of men and women who
specialties that are characterized by student’s specialty choice on the basis of were nonresponders (75.6%, 87 men, and
continuity of patient care (i.e., family his or her residency match at the time of 24.4%, 28 women) did not differ greatly
medicine, pediatrics, internal medicine, graduation. Specialty choice was divided by gender from the same type of
obstetrics– gynecology, and psychiatry) into two categories, five core specialties percentages of the responders (77.8%,
versus noncore specialties, where there is (i.e., internal medicine, family medicine, 326 men, and 22.2%, 93 women; P ⫽
less interpersonal contact and continuity pediatrics, obstetrics– gynecology, and .25). For nonresponders, 53.9% entered
of care (all other specialties, for instance, psychiatry) and noncore specialties (all core specialties, which did not differ from
emergency medicine, surgery, radiology, other choices, for instance, surgery, the percentage of responders that entered
pathology).10,15 With these possible pathology, and radiology). those specialties (P ⫽ 1.0). The female
personality–specialty connections in nonresponders did not differ statistically
mind, we designed the present study to Timing of test administration. Students in their likelihood of entering core or
determine whether vicarious empathy completed the questionnaire during noncore specialties from the female
decreases as students progress through registration for each academic year. responders (P ⫽ .82). The same was
medical school, and whether students Therefore, the M1 classes had no medical true for men: there was no statistical
choosing specialties with greater patient training, providing a baseline empathy difference between responders and
score. nonresponders in the distribution of
contact maintain vicarious empathy
specialty choice between core and
better than do students choosing
Analysis of data. Scores for each student noncore (P ⫽ .63). Therefore, the
specialties with less patient contact.
were calculated according to BEES nonresponders do not represent a bias in
instructions.16 Descriptive statistics were the data.
calculated by class, gender, and choice of
Method specialty. As stated earlier, we conducted There was a significant association
Setting and sample. We gathered this separate analyses for men and women, between gender and specialty choice, with
study’s data from a single South-Central because the BEES is gender specific. For 94 (63.9%) women planning to enter a
U.S. medical school: The University of each year, we conducted a two-factor core specialty compared with 134
Arkansas for Medical Sciences. Starting in repeated-measures ANOVA, using the (48.9%) men (P ⫽ .004). As anticipated
the 1997, 1998, 1999, and 2000 academic general linear model procedure from from the gender-sensitive BEES, the
years, the students in the graduating SPSS, with the significance level set at women always had significantly higher
classes of 2001, 2002, 2003, and 2004 P ⬍ .05. The between-subjects factor was BEES scores than the men (P ⬍ .001).
completed a survey at the beginning of specialty choice, and the within-subjects
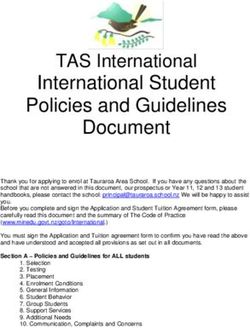
their freshman (M1), sophomore (M2), factor was time. Significant effects were Table 1 displays the mean scores by year
junior (M3), and senior (M4) years. With followed by post hoc tests. We also (M1–M4) and specialty preference for
approval from our local institutional performed single-sample tests of means men and women. Figure 1 shows part of
to compare our respondents with those the data in graphic form. Entering male
review board in 2005, we contacted the
in the normed sample for the BEES. medical students, regardless of specialty
535 graduates and asked whether they
choice, had empathy scores that were
would allow their data to be used in a
significantly higher than those in the
research study. A total of 419 (78.3%)
Results normal population (29 ⫾ 28; P ⬍ .001).16
students agreed, 1 student refused, and
The core male medical students stayed
115 students did not reply. Among the four classes, with 419 significantly more empathic than the
students in the study, 25.7% (108; 80.7% norms (P ⬍ .001) until they finished the
Survey instrument. The survey of the class) graduated in 2001, 26.0% junior year (see the M4 data point in
instrument was the Balanced Emotional (109; 78.4% of the class) graduated in Figure 1), when there was no longer a
Empathy Scale (BEES), a well-established 2002, 23.4% (98; 76.5% of the class) significant difference (P ⫽ .91). In
measure of the vicarious emotional graduated in 2003, and 24.8% (104; contrast, after finishing their freshman
qualities of empathy that examines 77.6% of the class) graduated in 2004. year, noncore male BEES scores (see the
the emotional “primitive” level of Our overall sample had 272 men M2 data point in Figure 1) dropped to
interpersonal interactions.8,16 The BEES (64.9%) and 147 women (35.1%). For where they were no longer significantly
coefficient alpha is 0.87. The BEES comparison, the entire graduating different from norm population scores.
consists of 30 positively or negatively medical school classes had 65.4%
worded items (15 items in each category) men and 34.5% women. Among the Entering female students had empathy
that measure responses to fictional four classes, there were no significant scores that were comparable with those of
situations and particular life events. differences in students’ empathy scores as the normal female population (60 ⫾ 21)16
Because the BEES is gender sensitive, they began medical school. Therefore, we until after completion of the junior year
with men scoring lower than women, the combined the four cohorts for the (see the M4 data point in Figure 1), when
students were asked to report their subsequent analyses. More than half of they dropped below the norm (P ⫽ .003).
gender. Using the students’ responses to the students (227; 54.2%) selected a core When women were classified by core and
the BEES, we analyzed the changes in the specialty (men ⫽ 133; 58.6%; women ⫽ noncore specialties, core women were
students’ vicarious empathy by gender 94; 41.4%), whereas the remainder always comparable with the norm (P ⬎
across their first three years of medical selected noncore specialties (men ⫽ 139; .05). However, noncore women started
school. 72.4%; women ⫽ 53; 27.6%). comparable with the norm (P ⫽ .14) but
Academic Medicine, Vol. 83, No. 3 / March 2008 245Physician–Patient Relationship
either gender, total BEES scores drop
Table 1 significantly from initial enrollment to
Empathy Scores of 419 Medical Students by Year and Specialty Choice, the beginning of the sophomore year.
2001–2004 Graduating Classes, the University of Arkansas for Medical Sciences* Empathy scores stay level from the
beginning of that year to the beginning of
Year of empathy score, by Specialty Mean
students’ gender choice† score‡ SD the junior year. After completing the first
clinical year, BEES scores decline sharply,
Empathy score 1, start of
freshman year
as evidenced by the senior BEES scores.
......................................................................................................................................................................................................... Thus, men’s and women’s scores both
Women Noncore 57.13 23.22
Core 64.35 19.98 have a significant cubic trend (i.e., a line
Total 61.75 21.41 with two inflection points and a central
.........................................................................................................................................................................................................
Men Noncore 35.88 23.99 plateau; P ⬍ .001 for men; P ⫽ .023 for
Core 39.95 20.53 women).
Total 37.87 22.42
.........................................................................................................................................................................................................
Total Noncore 41.74 25.56 For the women, there was no significant
Core 50.05 23.57 interaction of year in medical school with
Total 46.25 24.82 specialty choice (P ⫽ .22), but there were
Empathy score 2, start of significant main effects for type of
sophomore year
.........................................................................................................................................................................................................
specialty choice (P ⫽ .001), with core
Women Noncore 50.19 22.43 women having both a higher score and
Core 60.71 23.06 year of school than did noncore women
Total 56.92 23.32 (P ⫽ .001) where, as described above,
.........................................................................................................................................................................................................
Men Noncore 28.53 25.32 empathy scores followed a cubic trend.
Core 34.71 22.83
Total 31.56 24.29
Similar to the women, the men had no
......................................................................................................................................................................................................... significant interaction of time with
Total Noncore 34.51 26.36
Core 45.48 26.23
specialty choice (P ⫽ .19). BEES scores
Total 40.45 26.82 for the men differed significantly for
Empathy score 3, start of career choice (P ⫽ .006) and year of
junior year medical school (P ⬍ .001), as described
.........................................................................................................................................................................................................
Women Noncore 49.19 27.59 above.
Core 61.49 25.76
Total 57.05 27.00 Women choosing a core specialty had the
.........................................................................................................................................................................................................
Men Noncore 26.32 26.14 smallest M1–M4 decline of all groups at
Core 36.05 22.64 13.0%. Men entering a noncore specialty
Total 31.08 24.93 had the greatest single-year decline (M1–
.........................................................................................................................................................................................................
Total Noncore 32.64 28.39 M2; 20.5%) compared with all other
Core 46.59 27.02 groups. Men choosing a core specialty
Total 40.19 28.49 had a 25.8% drop in M1–M4 BEES
Empathy score 4, start of scores, whereas noncore men had a
senior year
......................................................................................................................................................................................................... 38.7% decline. Women entering a
Women Noncore 40.40 29.72 noncore specialty had a 29.3% M1–M4
Core 55.98 23.75
Total 50.36 27.02 decline in BEES scores, with a single
......................................................................................................................................................................................................... 17.3% drop in empathy after completing
Men Noncore 22.00 25.40
Core 29.66 26.94 the M3 year.
Total 25.75 26.40
......................................................................................................................................................................................................... For students choosing a core specialty,
Total Noncore 27.08 27.83
Core 40.56 28.72 there was a gender difference in the
Total 34.38 29.07 degree of decline in M1–M4 scores; the
men’s decline was essentially twofold
* The table presents mean scores by medical school year, specialty preference, and students’ gender. Scores are
for students’ vicarious empathy (i.e., to have a visceral empathic response); responses were to a well-established
greater than the women’s decline. Among
measure of the various emotional qualities of empathy, administered at the beginning of each medical school women, the drop in M1–M4 BEES scores
year. Vicarious empathy significantly decreased during medical education (P ⬍ .001), especially after the first was 2.25-fold greater for those who
and third years. Students choosing core careers had higher empathy than did those choosing noncore careers.
† choose noncore versus those who chose
Core specialties (i.e., family medicine, internal medicine, obstetrics– gynecology, pediatrics, and psychiatry) have
substantial patient contact and continuity of care, whereas noncore specialties (all others, including core specialties. For men, the drop in
anesthesiology, dermatology, and general surgery) have minimal patient contact and continuity of care. Totals in M1–M4 BEES scores was only 1.5-fold
this column are the combined women and men core or noncore scores for each year of the study. greater for the noncore versus core
‡
Totals in this column are the average women’s, men’s, and combined women’s and men’s scores for all students
at the start of the freshman, sophomore, junior, or senior year. students. In either gender, the greatest
declines in M1–M4 BEES scores are
associated with those students who
then dropped significantly For both men and women, the pattern of selected a noncore specialty.
lower than the norm (P ⬍ .002) after empathy scores (see Figure 1) across the
completing the freshman year (see the four time points (i.e., the first three A secondary analysis was done to
M2 data point in Figure 1). years of medical school) is similar. For determine how similar women’s scores
246 Academic Medicine, Vol. 83, No. 3 / March 2008Physician–Patient Relationship
Mean Score that occurred after completing the
70 freshman year of medical school may
have resulted from a high degree of
student stress and anxiety caused by the
60 students’ competitiveness and desire to
overachieve on examinations. Additional
stressful factors may include the media’s
50 presentation of doctors as heroes, which
helps create a skewed image of the ideal
physician for entering freshmen medical
40 students. As the students progressed
through their freshman year, they
probably realized there is a mismatch
30 between the media representation and
reality.19 Additionally, the freshmen likely
considered themselves to be in a hostile
20 educational environment that treated
M1 M2 M3 M4 them like children.20 All of these stressors
Women Core Women Total Women Non-Core
Men Core Men Total Men Non-Core induce self-preservation and coping
Figure 1 Mean scores, by medical school year, specialty preference, and students’ gender, for behaviors. In our view, some of these
419 men and women in the classes of 2001–2004, the University of Arkansas for Medical behaviors, expressed as increased
Sciences. Scores are for students’ vicarious empathy (i.e., to have a visceral empathic response); cynicism2 and, ostensibly, decreased
responses were to a well-established measure of the various emotional qualities of empathy, vicarious empathy, were used by the
administered at the beginning of each medical school year. The figure shows that vicarious students to adjust to the stresses and
empathy significantly decreased during medical education (P ⬍ .001), especially after the first and internal conflicts associated with medical
third years. Students choosing core careers had higher empathy than did those choosing noncore education.
careers. Core refers to core specialties (i.e., internal medicine, family medicine, obstetrics– gynecology,
pediatrics, and psychiatry, which have greater patient contact), and noncore refers to all other
The larger drop in the noncore empathy
specialties, where patient contact is less.
scores of the M2 women versus the core
empathy scores for the M2 women
were to men’s within specialty type. This significant decline in the component of suggest that the aforementioned stressors
analysis was prompted by the finding that empathy that is essential to patient care, may have a differential effect on some
women choosing noncore specialties had because empathy is one of three core women. We believe women choosing
lower BEES scores than did the other values needed to establish an effective core specialties may better maintain their
women when there was no similar physician–patient relationship.17 vicarious empathy, at least partially,
difference for the males. For students because the continuity of patient care (a
choosing a core specialty, women The results of this study suggest that characteristic of core specialties) lends
reported significantly higher empathy student empathy is affected by medical itself to attracting a more nurturing
scores than men did across all four time education. Our study supports the individual. Conversely, the marked drop
points (P ⬍ .001). The effect size, as findings of Coulehan and Williams,18 in vicarious empathy of women choosing
measured by a partial eta squared, was who described deleterious changes in noncore specialties may reflect more of a
0.33. Women choosing noncore various humanistic qualities as medical “survival” or “coping” mechanism.
specialties also had higher scores than students became “immunized” against Because noncore specialties (e.g.,
men choosing noncore specialties, but these values after their matriculation into orthopedics and surgery) are still
the difference was not as great (P ⫽ .02). medical school. In the freshman year, the predominately chosen by men, the
In this instance, the effect size was only similar M1 BEES scores for all four noncore women we studied were
0.045. classes indicate that the matriculates adjusting in the same way that the less
studied were drawn from a homogenous empathetic noncore males did.
population, and that the undergraduate
Discussion education of the matriculates, The sophomore year, which is an
Our study is unique in at least two predominated by basic science courses, additional year of basic science courses
aspects. It is the first longitudinal study to did not decrease vicarious empathy similar to the freshman experience,
follow four cohorts of undergraduate below the established norm. Indeed, the maintained stable BEES scores. This may
medical students. Second, it is the first entering male medical students had BEES be explained by the students’ acclimating
study to examine vicarious empathy (i.e., scores that were significantly higher than to the academic rigors of basic science
to have a visceral response) instead the norm. For both the men and the courses. The junior clinical year, where
of cognitive empathy (i.e., to, in women, the M1 BEES scores were not all students participate in standard
imagination, take the role of another) in significantly different between core and rotations, produced another dramatic
medical students. We believe that the noncore groups. drop in BEES scores for both the men
decrease in BEES scores revealed in this and the women. This drop substantiates
study represents a loss of vicarious For all the students studied, the findings from the literature that suggest
empathy. If so, this study reveals a significant decrease in vicarious empathy that the first clinical year of medical
Academic Medicine, Vol. 83, No. 3 / March 2008 247Physician–Patient Relationship
school is demanding and challenging.21 The “intended” medical curriculum, four-year curriculum.2,9,33,34 Some
The large drop in M3 students’ which is the formally offered and residency programs, aware of the
vicarious empathy occurred while the endorsed curriculum, often falls short of reduction in humanitarian traits in
students were seeing patients they had, student expectations because of the medical graduates, have developed
presumably, looked forward to helping. It “informal” and the “hidden” curricula.28 intensive workshops devoted to teaching
is interesting to note that a recent study The informal curriculum, as defined and enhancing physician–patient
showed that a similar drop in empathy by Hafferty,28 “is an unscripted, interactions, yet studies show that even
occurred after dental students began predominantly ad hoc, highly with such courses, idealism and empathy
seeing patients.22 In university tertiary interpersonal form of teaching that takes decrease and cynicism increases in as
care centers, empathy is hard to direct place among and between faculty and little as five months after the start
toward the challenging patients when the students” (e.g., in the hallway, lounge, or of the intern year.35–37 We maintain
treatment emphasis is on technology.23 on-call room), whereas the hidden that the attempted maintenance of
Immense cultural differences between curriculum “is a set of influences that professionalism should be part of the
physicians-in-training and patients may function at the level of organizational medical school curriculum that is
also make it more difficult to achieve structure and culture” (e.g., advertising combined with the reinstatement of
adequate empathy. Physicians who are the amount of National Institutes of effective bedside teaching. However, our
role models should work more closely Health dollars the institution garners or study findings suggest that the loss of
with medical students to develop an espousing the need for basic science innate, vicarious empathy could make it
empathic relationship with such rather than humanities courses when difficult to effectively teach medical
patients.24 Our own findings suggest that applying to medical school). These latter students, interns, and residents to
this could be particularly important for two curricula contribute to insidious consistently role-play empathic concern.
women who enter a noncore specialty, declines in desirable professional traits,
because their drop in vicarious empathy because students easily recognize that This study was of a single four-year
scores more closely emulated the campus policies and resource allocations medical school in the mid-South.
naturally lower empathy scores of the and “what’s really important to learn” Therefore, the findings may not be
men than the scores of their female often conflict with the stated institutional directly applicable to other medical
colleagues who selected a core specialty. educational mission.1,28 Instead, the institutions in the United States. During
mandate that should be implicit within the period of this longitudinal study, the
Studies show that clinicians consider an the informal and hidden curricula should curriculum at the institution remained
empathic physician–patient relationship be the societal obligation of medical fairly stable and can be described as
as one of the most important aspects of schools to provide and/or train better “traditional.” Therefore, differences in
professionalism5 and that professionalism physician role models who can aid empathy scores from year to year, or
and physician–patient interactions are students in overcoming losses in empathy between graduating classes, were not
best demonstrated by clinician role and other professional characteristics.26 influenced by large-scale curricular
models at the bedside in hospitals or,25 as changes. The students voluntarily took
suggested by Benbassat and Baumal,24 in The most frequently offered solutions to the BEES four times. As with any
primary and chronic care clinics and/or ameliorate the loss of professionalism at repeated measure, there are concerns that
hospice facilities. Other studies reveal a the undergraduate medical level involve familiarity with the survey may affect
chronic lack of clinical role models,26 and teaching students to be empathic or the students’ responses. For logistical
perhaps a lack of positive role models “humanitarian” via courses that reasons, this study did not examine BEES
could have contributed to the decline in emphasize empathic communication scores after the completion of the senior
empathy scores we observed after the skills.9,12,29 Evidence suggests that in most year. It is unknown whether another
completion of the first clinical year of instances the gains are modest and significant decrease in vicarious empathy
undergraduate medical education. temporary,10,30 and some feel that would have occurred after completion of
empathy and compassion are increasingly the M4 year or even into residency
In addition to complicated treatment difficult to teach as an individual training, but other studies suggest this
regimes and a lack of clinical role models, matures.20 In contrast to traditional four- would have been the case.34,35 A number
literature shows that juniors, as student/ year schools, several recent studies have of students did not respond to our
physicians (i.e., individuals that are shown that six-year medical schools, or request to use their BEES data. Therefore,
learning to assume an authoritative role schools with a problem-based learning the effect that these purged data would
in providing care while simultaneously curriculum, have greater opportunities to have had on our current results cannot
being subservient to their mentors), integrate humanism and empathy into be determined. However, we do know
perceive themselves as being abused their curricula.31,32 Despite some that for either gender, the numbers of
by their mentor/role models.1,21,27 encouraging initial reports from several nonresponders who entered core or
This student abuse has been termed of these nontraditional schools, a large noncore specialties on graduation did not
“traumatic deidealization” by Kay19 and cadre feels that medical students possess a differ significantly from those who did
is another factor possibly contributing to detrimental inertia, fueled by a frank permit their data to be used. Thus,
the declines in empathy. Other potential decline in ethics, morals, empathy, and nonresponder career choice was not a
factors include fatigue and a lack of service-oriented attitudes, that cannot be factor that could have skewed our results.
patient continuity that is exacerbated by overcome by a concurrent limited
starting a new clinical rotation every four exposure to the humanities, especially In conclusion, in our study, the first three
to five weeks. when presented in an already crowded years of medical education significantly
248 Academic Medicine, Vol. 83, No. 3 / March 2008Physician–Patient Relationship
decreased students’ vicarious empathy. 5 Brownell AK, Côté L. Senior residents’ views 21 Silver HK, Glicken AD. Medical student
The decline in empathy occurred in on the meaning of professionalism and how abuse: Incidence, severity and significance.
students who chose core and noncore they learn about it. Acad Med. 2001;76:734 – JAMA. 1990;263:527–532.
737. 22 Sherman JJ, Cramer A. Measurement of
specialties, with significant declines 6 Mehrabian A, Young AL, Sato S. Emotional changes in empathy during dental school.
occurring during the first basic science empathy and associated individual J Dent Educ. 2005;69:338 –345.
year as well as the initial clinical year differences. Curr Psychol Res Rev. 1988;8: 23 Griffith CH III, Wilson JF. The loss of student
when students were exposed to patients. 221–240. idealism in the 3rd-year clinical clerkships.
The decrease may constitute a coping or 7 Davis MH. Empathic concern and the Eval Health Prof. 2001;24:61–71.
muscular dystrophy telethon. Empathy as a 24 Benbassat J, Baumal R. What is empathy, and
survival mechanism where empathic multidimensional construct. Pers Soc Psychol how can it be promoted during clinical
feelings are suppressed. Although a Bull. 1983;9:223–229. clerkships? Acad Med. 2004;79:832– 839.
hardening of the heart may aid physicians 8 Chlopan BE, McCain ML, Carbonell JL, 25 Wright SM, Kern DE, Kolodner K, Howard
coping with patients on a daily basis, this Hagen RL. Empathy: Review of available DM, Brancati FL. Attributes of excellent
runs counter to the patient’s need for an measures. J Pers Soc Psychol. 1985;48:635– attending-physician role models. N Engl
653. J Med. 1998;339:1986 –1993.
empathic caregiver.38 Because of the
9 Diseker RA, Michielutte R. An analysis of 26 Greganti MA. Where are the clinical role
significant drop in vicarious empathy empathy in medical students before and models? Arch Intern Med. 1990;150:259 –261.
during medical school, we propose that following clinical experience. J Med Educ. 27 Brainard AH, Brislen HC. Learning
empathy should be constantly reinforced 1981;56:1004 –1010. professionalism: A view from the trenches.
by the use of role-playing throughout 10 Rezler AG. Attitude changes during medical Acad Med. 2007;82:1010 –1014.
students’ education and be periodically school: A review of the literature. J Med Educ. 28 Hafferty FW. Beyond curriculum reform:
1974;49:1023–1030. Confronting medicine’s hidden curriculum.
reinforced during their residency training 11 Jarski RW, Gjerde CL, Bratton BD, Brown Acad Med. 1998;73:403– 407.
and practice as physicians. DD, Matthes SS. A comparison of four 29 Evans M. Reflections on humanities in
empathy instruments in simulated patient– medical education. Med Educ. 2002;36:508 –
medical student interactions. J Med Educ. 513.
Acknowledgments 1985;60:545–551. 30 Kauss DR, Robbins AS, Abrass I, Bakaitis R,
The authors thank the Academic Affairs Office of 12 Stepien KA, Baernstein A. Educating for Anderson LA. The long-term effectiveness of
the College of Medicine for their assistance in empathy. J Gen Intern Med. 2006;21:524 – interpersonal skills training in medical
distributing the questionnaire, and Tom Hart 530. schools. J Med Educ. 1980;55:595– 601.
and Marilyn Walderns, of the Office of Academic 13 Hojat H, Mangione S, Nasca TJ, et al. An 31 Sirridge M, Welch K. The program in medical
Computing, for collating the data. This study was empirical study of decline in empathy in humanities at the University of Missouri–
supported by the UAMS Teaching Scholars medical school. Med Educ. 2004;38:934 –941. Kansas City School of Medicine. Acad Med.
Program (funded by the Arkansas Department of 14 Newton BW, Savidge MA, Barber L, et al. 2003;78:973–976.
Higher Education) and Research to Prevent Differences in medical students’ empathy. 32 Roche WP III, Scheetz AP, Dane FC, Parish
Blindness. Special thanks to John Németh. Acad Med. 2000;75:1215. DC, O’Shea JT. Medical students’ attitudes
15 Hojat M, Brigham TP, Gottheil E, Xu G, in a PBL curriculum: Trust, altruism, and
Glaser K, Veloski JJ. Medical students’ cynicism. Acad Med. 2003;78:398 – 402.
References personal values and their career choices a 33 Pellegrino ED. The metamorphosis of
quarter-century later. Psychol Rep. 1998;83: medical ethics. A 30-year retrospective.
1 Hafferty FW, Franks R. The hidden
curriculum, ethics teaching, and the structure 243–248. JAMA. 1993;269:1158 –1162.
of medical education. Acad Med. 194;69:861– 16 Mehrabian A. Manual for the Balanced 34 Rogers J. Being skeptical about the medical
871. Emotional Empathy Scale (BEES); 1996 humanities. J Med Humanit. 1995;16:265–
2 Testerman JK, Morton KR, Loo LK, Worthley [unpublished; available from Albert 277.
JS, Lamberton HH. The natural history of Mehrabian, 1130 Alta Mesa Road, Monterey, 35 Griffith CH, Wilson JF. The loss of idealism
cynicism in physicians. Acad Med. 1996;71 CA 93940]. throughout internship. Eval Health Prof.
(10 suppl):S43–S45. 17 Rogers CR. A Way of Being. Boston, Mass: 2003;26:415– 426.
3 Branch WT Jr. Supporting the moral Houghton Mifflin; 1980. 36 Bellini LM, Baime M, Shea JA. Variation of
development of medical students. J Gen 18 Coulehan J, Williams PC. Vanquishing virtue: mood and empathy during internship. JAMA.
Intern Med. 2000;15:503–508. The impact of medical education. Acad Med. 2002;287:3143–3146.
4 Levinson W, Roter DL, Mullooly JP, 2001;76:598 – 605. 37 Klein EJ, Jackson JC, Kratz L, et al. Teaching
Dull VT, Frankel RM. Physician–patient 19 Kay J. Traumatic deidealization and the professionalism to residents. Acad Med. 2003;
communication. The relationship with future of medicine. JAMA. 1990;263:572–573. 78:26 –34.
malpractice claims among primary care 20 Kimball CP. Medical education as a 38 Rosenfield PJ, Jones L. Striking a balance:
physicians and surgeons. JAMA. 1997;277: humanizing process. J Med Educ. 1973;48: Training medical students to provide
553–559. 71–77. empathic care. Med Educ. 2004;38:927–933.
Academic Medicine, Vol. 83, No. 3 / March 2008 249You can also read