Tourette syndrome in children - RACGP
←
→
Page content transcription
If your browser does not render page correctly, please read the page content below
Focus | Clinical
Tourette syndrome
in children
Valsamma Eapen, Tim Usherwood UP TO 20% OF CHILDREN exhibit rapid jerky peak severity at the age of approximately
movements (motor tics) that are made 10–12 years, and typically improve by
without conscious intention as part of a adolescence or thereafter.6
Background
Gilles de la Tourette syndrome (GTS),
developmental phase that often lasts a few
characterised by motor and vocal tics, weeks to months.1 Similarly, involuntary
has a prevalence of approximately 1% sounds, vocalisations or noises (vocal or Clinical features
in school-aged children. Commonly phonic tics) such as coughing and even In addition to simple motor and vocal/
encountered comorbidities of GTS brief screams or shouts may be observed in phonic tics, complex tics may be present
include attention deficit hyperactivity some children for brief periods of time. Tics (Table 1). Some complex tics – such as
disorder (ADHD) and obsessive-
lasting for a few weeks to months are known spitting, licking, kissing, etc – may be
compulsive behaviour/disorder (OCB/
OCD). Genetic factors play an important
as ‘transient tic disorder’. When single misunderstood or misinterpreted and
part in the aetiology of GTS, and family or multiple motor or vocal tics – but not a may result in the young person getting
members may exhibit tics or related combination of both – have been present in trouble, especially if these tics include
disorders such as ADHD, OCB or OCD. for more than one year, the term ‘chronic involuntary and inappropriate obscene
tic disorder’ is used. When both (multiple) gesturing (copropraxia) or copying the
Objective
The aim of this article is to present a motor and (one or more) vocal tics have been movements of other people (echopraxia).
summary of the current evidence to assist present for more than a year, with onset Similarly, complex vocal tics may include
the assessment and management of GTS before the age of 18 years, the condition is repeating words or phrases or even
in primary care. known as Gilles de la Tourette syndrome full sentences (echolalia) or repeating
(GTS) or, in short, Tourette syndrome.2 the last word or syllable (palilalia) or,
Discussion
A comprehensive assessment should The aim of this article is to review in approximately 10–15% of cases,
include exploration of not only tics current evidence regarding the involuntary and inappropriate swearing or
but also associated features and assessment and management of GTS. blurting out of obscenities (coprolalia).
comorbidities. The stigmatising and Tics are usually preceded by a
impairing nature of tics can have a premonitory sensation or urge, such as
significant impact on the quality of life Prevalence a feeling of tightness, stretch, tension
of the young person and their parents/
carers, as well as on family functioning.
Once considered rare, GTS is now or itching that is relieved by performing
Management includes education and understood to be relatively common, the tic, thereby leading to an urge-tic-
explanation, behavioural treatments occurring in approximately 1% of relief cycle.7,8 Patients with GTS may
and (sometimes) medication. school-aged children.3 GTS is more also exhibit a number of associated
common in boys, and the male-to-female behaviours such as rage, self-injurious
ratio is estimated to be 4:1.4,5 Tics have behaviours or non-obscene socially
a mean age of onset of 6–7 years, reach inappropriate behaviours that involve
120 Reprinted from AJGP Vol. 50, No. 3, March 2021 © The Royal Australian College of General Practitioners 2021Tourette syndrome in children Focus | Clinical
socially inappropriate comments or observable tics but then show increased members. Tics should be distinguished
actions.9 Attention deficit hyperactivity frequency when they return home. This from involuntary movements due to other
disorder (ADHD) is encountered in may lead to a misunderstanding that conditions (Table 2).5 Careful neurological
approximately 60–75% of children with children can suppress the tics if they examination may provide reassurance for
GTS, while obsessive-compulsive disorder try harder. If anxiety and stress worsen the patient, parent/carer and doctor.
(OCD) is reported in 27%, obsessive- the tics, then they may be mistaken as Once a diagnosis is made, further
compulsive behaviours (OCB) in 32%, ‘psychological’ in origin. Rarely, tics assessments should include those of
and self-injurious behaviours in 25%.10 may be brought on, or made worse, by comorbid conditions, associated features
Although less common, features of autism, a bacterial (eg group A streptococcus) and the impact of their symptoms (Figure 1).
learning difficulties, anxiety, depression, infection such as in paediatric autoimmune
phobia, irritability, impulsivity, rage, neuropsychiatric disorder associated with
aggression, sleep difficulties, oppositional streptococcal infection. Social impact and quality of life
or conduct problems, substance use Tics can affect a child’s life in a number
or personality issues may co-exist.11 of ways; these include the impact on
Some individuals’ overall academic Aetiology school and academic work, social life
and social functioning as well as quality Genetics play a major factor in the and relationships as well as physical and
of life (QoL) may be affected more by development of GTS, but the mechanisms mental wellbeing.12 The visible nature
these associated problems than the tics are complex. While no single susceptibility of the tics may draw attention to the
themselves.12 Regarding the age of onset, gene of large effect has been identified as individual or lead to embarrassment,
it is noteworthy that symptoms of ADHD yet, twin and family studies suggest that teasing/bullying or social exclusion.
may appear between three and six years of it is highly heritable, with a population- Impact on school work may be due to the
age (ie before the tics manifest), while the based heritability estimate of 0.771.13 effect of tics on learning or due to related
OCD symptoms usually manifest in late Environmental factors are also involved, conditions such as ADHD, OCD/OCB or an
childhood or adolescence. such as pre- and perinatal factors associated learning disorder.15 The ability
Tics can come and go, and they take a including difficulties with pregnancy, to focus in class and engage in school
waxing and waning course. While tics are smoking, exposure to infection, immune activities may be reduced as a result of the
involuntary, they are sometimes referred or inflammatory factors and psychosocial child spending time and energy on trying
to as ‘unvoluntary’ because the person may stressors, as well as birth complications.14 to hide or suppress the tics while at school.
be able to suppress the tics for a period of Corticostriatal circuitry is implicated in GTS, Other students or teachers may accuse the
time, and some of the complex tics may with excess dopamine levels thought to be individual with tics of deliberately ‘pulling
be camouflaged to look like purposeful the underlying neurochemical abnormality. faces’, spitting or disturbing the class
movements. Thus children may voluntarily through grunts or vocalisations.
suppress their tics for short periods of QoL has been shown to be lower in
time that may vary from seconds to Assessment people living with GTS when compared
minutes or hours, but this is at the expense Assessment should include a detailed with the general population.16 Among
of mounting inner tension and is often history inquiring about not only tics patients with GTS, individuals without
followed by a rebound or increase in tics. but also other associated conditions comorbidities have been found to
For example, some children may manage including ADHD, OCD and OCB, in have better QoL than those with
the school hours fairly well without many the patient as well as among family comorbidities.17 Parent-reported
Table 1. Common tics of Tourette syndrome*
Simple Complex
(involuntary meaningless movements) (unvoluntary seemingly purposeful movements)
Motor tic Eye blinking, eye rolling, squinting, facial grimaces, Pulling of clothes, touching people/objects, poking/jabbing,
shoulder shrugging, arm extending, mouth opening, smelling fingers/objects, punching self, jumping/skipping,
nose twitching, lip licking, head jerks, brushing or kicking, hopping, walking on toes, kissing self or others, feet
tossing hair out of eyes shuffling, flapping arms, twisting around, twirling hair, self-
injurious behaviour, biting, picking skin or scabs
Vocal/phonic tic Throat clearing, grunting, snorting, yelling/screaming, Making small animal-like sounds, unusual changes of pitch
sniffing, barking, laughing, coughing, spitting, and volume of voice, stuttering, repetition of sounds
squeaking, humming, whistling, honking
*This is not an all-inclusive list
© The Royal Australian College of General Practitioners 2021 Reprinted from AJGP Vol. 50, No. 3, March 2021 121Focus | Clinical Tourette syndrome in children
comorbidity in children and adolescents GTS have ‘Tourette-plus’, where one or Association of Australia, and the health
with GTS has been found to be associated more comorbid conditions are present professional that they have consulted
with decreased QOL, increased emotional (Figure 3).9 Management in these situations may provide information to schools or
symptomatology and impaired emotional, should take into account the symptoms that other environments in which the child
social (including peer relationship) are causing most distress or dysfunction. interacts. The biological nature of tics
and school functioning.18 Warm and should be highlighted, and it should
supportive family relationships are integral Education, explanation and advice be emphasised that they are not due to
to long-term social and emotional stability All affected children and their families stress or ‘bad parenting’.
in children with GTS and their QoL.12 need information about the nature and Following assessment and explanation
course of GTS and any accompanying about the nature of the condition,
conditions, and advice on how to manage moderate cases may benefit from referral
Management tics. For mild cases, advice regarding tic to a psychologist for behavioural methods
Management options for children and management may be all that is needed. of treatment. When the tics are severe with
young people with GTS include education, It is important to emphasise to the associated distress and/or dysfunction, or
explanation and advice; linking with support parents/carers and child that the tics are when significant comorbidities are present,
groups; and behavioural interventions involuntary and outside the child’s control, the general practitioner (GP) may refer
as well as medication. A decision tree on and that they cannot help these sudden the patient to a specialist with expertise
management is outlined in Figure 2.2 movements or voices/noises. A parallel in GTS for a comprehensive assessment
It is noteworthy that only approximately may be drawn with trying to supress a and management plan. GPs can refer
10% of patients with GTS have ‘pure sneeze or avoid blinking. to clinical psychologists under a mental
Tourette’, where they present with only The young person and their family may healthcare plan for the implementation
motor and vocal tics. Most patients with be linked up with the Tourette Syndrome of behavioural treatments.
Table 2. Differential diagnosis of Tourette syndrome5
Diagnosis Characteristic feature
Gilles de la Tourette syndrome Onset at approximately 6–7 years of age, with further emergence of symptoms that peak at
approximately 10–12 years of age, and remission post-adolescence; waxing and waning course;
the type and site of tics changes from one place to another; voluntarily suppressible for short
periods of time
Athetoid type of cerebral palsy Onset between birth and three years of age; static course; associated neurological deficit and
learning disability
Dystonia musculorum deformans Torsion dystonia of legs – progressive; crippling 10–15 years after onset
Spasmodic torticollis Associated with spastic speech; static or progressive
Encephalitis lethargica History of encephalitis, Parkinsonian symptoms
Huntington’s chorea Onset in third to fifth decades (1% in early childhood); usually a positive family history of
Huntington’s chorea; choreoathetoid movements; dementia; progression to death in 10–20 years
Other involuntary movements Myoclonus: shock-like, arrhythmic twitches; not suppressible
Chorea: dance-like, unpatterned movements; often approximate a purpose (eg adjusting clothes,
checking a watch); often rapid, involving proximal or distal muscle groups
Athetosis: writhing movement, mostly arms/hands; often slow
Dystonia: sustained or repetitious muscular contractions; often produces abnormal posture
Hemiballismus: wild, large amplitude, flinging movements on one side of the body, commonly
affecting proximal limb muscles but can also affect the trunk
Tardive tourettism History of long-term use of neuroleptics, levodopa or other medications
Other neurological disorders Signs and symptoms specific to the disorder such as autistic disorder, post-stroke, Sydenham’s
chorea, multiple sclerosis, Wilson’s disease, Hallervorden-Spatz disease, Jakob–Creutzfeldt
disease, choreoathetosis, neurofibromatosis, Arnold–Chiari malformation and status
dysmyelinatus
Acquired tourettism Onset in adulthood; trauma; carbon monoxide poisoning; basal ganglia infarct
122 Reprinted from AJGP Vol. 50, No. 3, March 2021 © The Royal Australian College of General Practitioners 2021Tourette syndrome in children Focus | Clinical
Behavioural methods of treatment urge or tic occurs. The social support Small doses of antipsychotics, such
For children with mild-to-moderate component involves teaching the patient’s as risperidone, aripiprazole, amisulpride
tics, effective treatments include parent (or another person) to praise the or haloperidol, can help control the tics.
specific behavioural techniques such patient for using the competing response It is recommended that patients are
as exposure and response prevention correctly and to remind the patient to use prescribed a low dose, which is then
(ERP), habit reversal therapy (HRT)19 and the competing response. increased slowly if side effects do not
comprehensive behavioural intervention occur. First-generation antipsychotics such
for tics (CBIT).20 In ERP, the patient Medication as haloperidol have been the treatment of
is trained to stay exposed, endure the For moderate-to-severe tics and other choice since the 1960s but are used less
premonitory urge and prevent or resist features of GTS causing either distress or frequently nowadays because of the risk
performing the tic symptoms. In HRT, dysfunction, it is worthwhile considering of extrapyramidal syndromes. Weight
patients are trained to do competing medication. The following medications gain and metabolic effects need to be
responses instead of performing the tics, may be useful. monitored when a patient is prescribed
and the program consists of awareness Centrally acting α-adrenergic agents second-generation antipsychotics such
training with self-monitoring, relaxation such as clonidine or guanfacine are usually as risperidone or aripiprazole. When
training and competing response training. the first line of treatment, especially if tics considering the choice of medication
CBIT combines awareness training and hyperactivity are both present. It is for tics, the effects of the medication
with competing response training and important to monitor blood pressure as on comorbid disorders also deserve
social support. Following awareness these agents can cause hypotension. There consideration. For example, clonidine can
training, patients are taught to engage is also a risk of rebound hypertension if the be useful when the patient also has ADHD
in a ‘competing response’ every time the medication is ceased abruptly. and sleep problems, while risperidone can
have additional benefits when comorbid
aggression and behavioural problems
are present. Aripiprazole has been found
to augment the therapeutic response to
selective serotonin reuptake inhibitors in
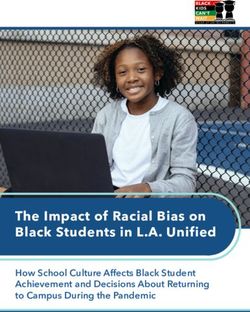
Patient presents with tics. patients who also have OCD, anxiety or
major depressive disorder.21
Less commonly used treatments
that are typically reserved for complex
Distinguish tics from other causes. Tourette syndrome should be cases with comorbid epilepsy and other
suspected if: complexities include anticonvulsants
• multiple motor and at least one vocal or phonic tic are present (eg topiramate, carbamazepine,
• tics have been present for >1 year levetiracetam), benzodiazepines
• tics started before the age of 18 years. (eg clonazepam) and cannabinoids.2
Although not used in children, in adults
with severe refractory and treatment-
resistant GTS, deep-brain stimulation
(DBS) has been used with some success.22
Confirm diagnosis and establish severity.
DBS involves the implantation of
electrodes for chronic stimulation aimed
at modulating neuronal activity in target
regions. There is significant heterogeneity
• Assess for: in outcomes, and there is also a lack of
– comorbid conditions (obsessive compulsive disorder, attention consensus regarding the ideal brain target;
deficit hyperactivity disorder)
therefore, further research is needed.
– associated features (depression, anxiety and learning problems)
– integral features (self-injurious behaviours).
• Assess how the child is functioning in social situations, for example Conclusion
at school, and the impact of symptoms.
Tics are frequently under-recognised
or misdiagnosed; simple tics may be
discounted as habits, and complex tics
as behavioural disorders. Increased
Figure 1. Assessment of patients presenting with tics awareness of the condition and better
supports are sorely needed.
© The Royal Australian College of General Practitioners 2021 Reprinted from AJGP Vol. 50, No. 3, March 2021 123Focus | Clinical Tourette syndrome in children
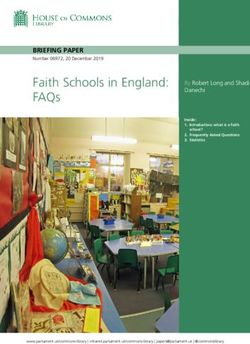
Tic disorder
Symptoms or indicators
Treatment
Psychoeducation
Presence of tics, but no
Yes
indication for treatment Monitoring
No
Presence of tics, but Yes Treatment of comorbid
comorbid disorder(s) disorder(s)
have treatment priority
No
Indication for treatment Yes Behavioural therapy
of tics, with preference (HRT, CBIT and ERP)
for (and availability of)
behavioural treatment
Combination of
pharmacotherapy and
Tics still with indication Yes behavioural therapy
No
for treatment
Combined pharmacotherapy
with different agents
Indication for treatment
of tics, with preference
for pharmacological
Yes Pharmacotherapy
treatment
Yes
Tics still with indication Yes Alternative therapies in specialised centres (DBS,
for treatment cannabinoids, botulinum toxin, among others)
Figure 2. Decision tree for the management of Tourette syndrome
CBIT, comprehensive behavioural intervention for tics; DBS, deep-brain stimulation; ERP, exposure and response prevention; HRT, habit reversal therapy
Reproduced with permission from Robertson MM, Eapen V, Singer HS, et al, Gilles de la Tourette syndrome, Nat Rev Dis Primers 2017;3:16097,
doi: 10.1038/nrdp.2016.97.
Key points • GTS occurs in around 1% of considerably better by young adulthood.
• Motor tics occur in up to 20% of school-aged children. • For mild cases, explanation and advice
children as a developmental phase but • Tics usually appear around the age of about the condition may be sufficient,
usually do not last longer than a year. 6–7 years, increasing in severity until while moderate-to-severe cases will
• GTS is diagnosed when there are several the age of approximately 10–12 years, benefit from referral to a specialist
motor tics and at least one vocal tic that after which they start to reduce and – with expertise in the assessment and
have been present for more than a year. in the majority of cases – become management of GTS.
124 Reprinted from AJGP Vol. 50, No. 3, March 2021 © The Royal Australian College of General Practitioners 2021Tourette syndrome in children Focus | Clinical
9. Eapen V, Robertson MM. Are there distinct
subtypes in Tourette syndrome? Pure-Tourette
syndrome versus Tourette syndrome-plus, and
simple versus complex tics. Neuropsychiatr Dis
Treat 2015;11:1431–36. doi: 10.2147/NDT.S72284
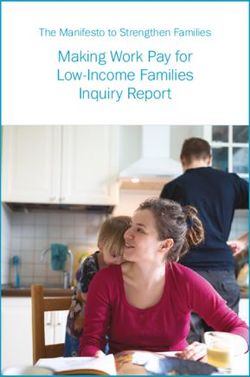
Tourette 10. Freeman RD, Fast DK, Burd L, Kerbeshian J,
Tics
syndrome Robertson MM, Sandor P. An international
perspective on Tourette syndrome: Selected
findings from 3,500 individuals in 22 countries.
Dev Med Child Neurol 2000;42(7):436–47.
doi: 10.1017/s0012162200000839.
11. Eapen V, Črnčec R, McPherson S, Snedden C.
Tic disorders and learning disability: Clinical
characteristics, cognitive performance
Attention deficit Obsessive-
and comorbidity. Australas J Spec Educ
hyperactivity compulsive 2013;37(2):162–72. doi: 10.1017/jse.2013.2.
disorder disorder 12. Eapen V, Cavanna AE, Robertson MM.
Comorbidities, social impact, and quality of life
in Tourette syndrome. Front Psychiatry 2016;7:97.
doi: 10.3389/fpsyt.2016.00097.
13. Mataix-Cols D, Isomura K, Pérez-Vigil A, et al.
Familial risks of Tourette syndrome and chronic
Behavioural problems, tic disorders. A population-based cohort study.
poor impulse control JAMA Psychiatry 2015;72(8):787–93. doi: 10.1001/
jamapsychiatry.2015.0627.
and other behavioural
14. Eapen V, Perkes I, Goff R. Pathways from genes
disorders
to symptoms in Gilles de la Tourette syndrome
(GTS). In: Martino D, Leckman JF, editors. Tourette
syndrome. New York, NY: Oxford University Press,
2021 [in press].
15. Dornbush MP, Pruitt SK. Teaching the tiger:
Figure 3. Conditions associated with Tourette syndrome A handbook for individuals involved in the education
of students with attention deficit disorders, Tourette
syndrome, or obsessive-compulsive disorder. Carol
Stream, IL: Hope Press, 1995.
16. Elstner K, Selai CE, Trimble MR, Robertson MM.
• No single cause has been found for Correspondence to:
v.eapen@unsw.edu.au
Quality of life (QOL) of patients with Gilles
de la Tourette’s syndrome. Acta Psychiatr
GTS, but the major contributing factors Scand 2001;103(1):52–59. doi: 10.1034/j.1600-
include genetics and pre- and perinatal References 0447.2001.00147.x.
difficulties. 17. Eapen V, Snedden C, Črnčec R, Pick A, Sachdev P.
1. Black KJ, Black ER, Greene DJ, Schlaggar BL.
Tourette syndrome, co-morbidities and quality
• Ninety per cent of people living Provisional tic disorder: What to tell parents
when their child first starts ticcing. F1000Res
of life. Aust N Z J Psychiatry 2016;50(1):82–93.
with GTS will experience comorbid 2016;5:696. doi: 10.12688/f1000research.8428.1.
doi: 10.1177/0004867415594429.
conditions such as ADHD or OCD/ 18. O’Hare D, Helmes E, Reece J, Eapen V, McBain K.
2. Robertson MM, Eapen V, Singer HS, et al.
The differential impact of Tourette’s syndrome
OCB or associated features such as Gilles de la Tourette syndrome. Nat Rev Dis
and comorbid diagnosis on the quality of life
Primers 2017;3:16097. doi: 10.1038/nrdp.2016.97.
depression and anxiety. 3. Robertson MM. A personal 35 year
and functioning of diagnosed children and
adolescents. J Child Adolesc Psychiatr Nurs
perspective on Gilles de la Tourette syndrome: 2016;29(1):30–36. doi: 10.1111/jcap.12132.
Prevalence, phenomenology, comorbidities,
Authors 19. Capriotti MR, Himle MB, Woods DW. Behavioral
and coexistent psychopathologies. Lancet
treatments for Tourette syndrome. J Obsessive
Valsamma Eapen MBBS, PhD, FRCPsych, Psychiatry 2015;2(1):68–87. doi: 10.1016/S2215-
Compuls Relat Disord 2014;3(4):415–20.
FRANZCP, Chair, Infant Child and Adolescent 0366(14)00132-1.
doi: 10.1016/j.jocrd.2014.03.007.
Psychiatry, University of New South Wales, NSW; 4. Jankovic J, Kurlan R. Tourette syndrome: Evolving
Head, Academic Unit of Child Psychiatry, South concepts. Mov Disord 2011;26(6):1149–56. 20. Piacentini J, Woods DW, Scahill L, et al.
West Sydney (AUCS), NSW; Stream Director, Early doi: 10.1002/mds.23618. Behavior therapy for children with Tourette
Life Determinants of Health, Sydney Partnership disorder: A randomized controlled trial. JAMA
5. Kurlan R. The differential diagnosis of tic 2010;303(19):1929–37. doi: 10.1001/jama.2010.607.
for Health, Education, Research and Enterprise disorders. In: Martino D, Leckman JF, editors.
(SPHERE), NSW; Director, Program 1, Co-operative Tourette syndrome. New York, NY: Oxford 21. Eddy CM, Rickards HE, Cavanna AE. Treatment
Research Centre for Autism (CRC), Qld; Director, University Press, 2013; p. 395–401. strategies for tics in Tourette syndrome.
BestSTART-SW (Systems Transformation and Ther Adv Neurolo Disord 2011;4(1):25–45.
Research Translation – South West Sydney) 6. Bloch MH, Peterson BS, Scahill L, et al. doi: 10.1177/1756285610390261.
Academic Unit, NSW Adulthood outcome of tic and obsessive-
compulsive symptom severity in children with 22. Martinez-Ramirez D, Jimenez-Shahed J,
Tim Usherwood BSc, MBBS, MD (Res), DMS, FRCP, Tourette syndrome. Arch Pediatr Adolesc Med Leckman JF, et al. Efficacy and safety of deep
FRCGP, FRACGP, FAICD, Head, Westmead Clinical 2006;160(1):65–69. doi: 10.1001/archpedi.160.1.65. brain stimulation in Tourette syndrome: The
School, The University Of Sydney, NSW; Professor of International Tourette Syndrome Deep Brain
General Practice, Faculty of Medicine and Health, The 7. Leckman JF, Walker DE, Cohen DJ. Premonitory Stimulation Public Database and Registry.
University of Sydney, NSW; Honorary Professorial urges in Tourette’s syndrome. Am J Psychiatry JAMA Neurol 2018;75(3):353–59. doi: 10.1001/
Fellow, The George Institute for Global Health, 1993;150(1):98–102. doi: 10.1176/ajp.150.1.98. jamaneurol.2017.4317.
Sydney, NSW 8. Woods DW, Piacentini J, Himle MB, Chang S.
Premonitory urge for tics scale (PUTS): Initial
Competing interests: TU has lived with Tourette
psychometric results and examination of the
syndrome since the age of six years.
premonitory urge phenomenon in youths
Funding: None. with tic disorders. J Dev Behav Pediatr
Provenance and peer review: Commissioned, 2005;26(6):397–403. doi: 10.1097/00004703-
externally peer reviewed. 200512000-00001. correspondence ajgp@racgp.org.au
© The Royal Australian College of General Practitioners 2021 Reprinted from AJGP Vol. 50, No. 3, March 2021 125You can also read