Novel therapies with precision mechanisms for type 2 diabetes mellitus - Nature
←
→
Page content transcription
If your browser does not render page correctly, please read the page content below
Reviews
Novel therapies with precision
mechanisms for type 2 diabetes
mellitus
Leigh Perreault 1 ✉, Jay S. Skyler2 and Julio Rosenstock3
Abstract | Type 2 diabetes mellitus (T2DM) is one of the greatest health crises of our time and
its prevalence is projected to increase by >50% globally by 2045. Currently, 10 classes of drugs
are approved by the US Food and Drug Administration for the treatment of T2DM. Drugs in
development for T2DM must show meaningful reductions in glycaemic parameters as well as
cardiovascular safety. Results from an increasing number of cardiovascular outcome trials using
modern T2DM therapeutics have shown a reduced risk of atherosclerotic cardiovascular disease,
congestive heart failure and chronic kidney disease. Hence, guidelines have become increasingly
evidence based and more patient centred, focusing on reaching individualized glycaemic goals
while optimizing safety, non-glycaemic benefits and the prevention of complications. The bar
has been raised for novel therapies under development for T2DM as they are now expected to
achieve these aims and possibly even treat concurrent comorbidities. Indeed, the pharmaceutical
pipeline for T2DM is fertile. Drugs that augment insulin sensitivity, stimulate insulin secretion or
the incretin axis, or suppress hepatic glucose production are active in more than 7,000 global
trials using new mechanisms of action. Our collective goal of being able to truly personalize
medicine for T2DM has never been closer at hand.
Formal diagnostic criteria for diabetes mellitus were speculation that some agents, such as thiazolidinedi-
first introduced by the National Diabetes Data Group ones, might actually increase cardiovascular risk10. On
in 1979 (ref.1) and by the World Health Organization in account of these concerns, in 2008, the FDA mandated
1980 (ref.2). Expanded and refined over time, plasma glu- cardiovascular safety studies be conducted for all new
cose thresholds for diagnosis remain in diagnostic criteria medications approved for lowering plasma levels of glu-
today based on their predictive value for microvascular cose in patients with T2DM. Knowledge gained from the
disease, specifically retinopathy1. Furthermore, land- cardiovascular outcome trials of these newer agents has
mark trials have convincingly demonstrated a reduction considerably expanded our understanding of T2DM and
in incidence of microvascular disease with decreasing what can be done for patients. Specifically, glucagon-like
levels of plasma glucose in both type 1 diabetes melli- peptide 1 (GLP1) receptor agonists and sodium–
tus and type 2 diabetes mellitus (T2DM)3–7. Altogether, glucose cotransporter 2 (SGLT2) inhibitors exert desir-
diabetes mellitus is largely conceived as a disease of ele- able ‘off-target’ non-glycaemic effects (for example,
vated blood concentrations of glucose. The reduction reductions in body weight and blood pressure), have
1
University of Colorado
in HbA1c remains a central focus of care8 as well as the improved safety profiles (for example, no incidences of
Anschutz Medical Campus, benchmark used by the FDA to approve pharmaceuticals hypoglycaemia, as compared with insulin and sulfony-
Aurora, CO, USA. that lower plasma concentrations of glucose. lureas), reduce the risk of atherosclerotic cardiovascular
2
Diabetes Research Institute, Nevertheless, much ado has been made about how disease and hospitalization for heart failure, and slow
University of Miami, Miami, to safely decrease plasma concentrations of glucose in the progression of diabetic kidney disease11–17. These
FL, USA.
people with T2DM, with health-care providers citing beneficial effects are all in addition to their ability to
3
Dallas Diabetes Research concerns over the potential for hypoglycaemia and decrease plasma concentrations of glucose. Interestingly,
Center at Medical City,
Dallas, TX, USA.
weight gain and, most notably, cardiovascular safety8,9. SGLT2 inhibitors can also reduce the number of hospi-
✉e-mail: leigh.perreault@ The latter point arose from interventional randomized talizations for heart failure in people without T2DM18,19.
cuanschutz.edu controlled trials in patients with T2DM, which repeat- This finding suggests that the cardiovascular benefits are
https://doi.org/10.1038/ edly showed a failure to reduce cardiovascular risk by provided by a mechanism that is independent from the
s41574-021-00489-y decreasing plasma levels of glucose4–7, together with glucose-lowering effects.
364 | June 2021 | volume 17 www.nature.com/nrendo
0123456789();:Reviews
that indirectly affect glycaemia (for example, anti-obesity
Key points
therapies) or used for complications related to T2DM.
• Type 2 diabetes mellitus (T2DM) is one of the greatest health crises of our time, and Third, we excluded preclinical, non-human phase
the number of people with T2DM is projected to increase by >50% globally by 2045. evaluations or therapies that failed to meet their
• Despite our extensive armamentarium of current drug treatments for T2DM, >7,000 safety and/or efficacy end points (that is, terminated
trials are registered around the world, many looking at ‘novel’ drug targets. development programmes). Outcomes provided to
• Mechanisms of action for novel drugs in the pipeline for T2DM include directly ClinicalTrials.gov and publications available on PubMed
targeting β-cells, targeting the incretin axis, directly or indirectly affecting glucose were used to corroborate the phase and status of trials,
metabolism in the liver, and increasing insulin sensitivity. whenever possible.
• In our judgement, compounds with the most promise include dual-acting and Thus, this Review focuses on the identification of
triple-acting incretin mimetics owing to their glucose-lowering capacity, potentially novel pharmaceuticals for T2DM that are
non-glycaemic benefits and safety.
in active or completed clinical trials and conducted in
• The bar has been raised for novel therapies under development for T2DM; new people with T2DM, with decreasing HbA1c levels as the
therapies are now expected to prevent cardiovascular and renal complications primary outcome, specifically for the purpose of meeting
independent of and in addition to their ability to decrease the plasma concentrations
regulatory approval.
of glucose.
Identified novel mechanisms of action
In pursuit of precision medicine, guidelines for peo- Once the aforementioned criteria were applied, we iden-
ple with T2DM are now principally focused on reaching tified 43 compounds with highly novel mechanisms of
individualized glycaemic targets, while optimizing safety, action in development for T2DM. Collectively, their
non-glycaemic benefits, and the prevention of micro- glucose-lowering mechanisms could be grouped into
vascular and macrovascular complications for individual four over-arching physiological effectors of diabetes
patients who are at risk of specific complications20. Novel mellitus. First are drugs that stimulate insulin secre-
therapies in development will not only need to show tion directly from β-cells (Fig. 1). These include both
meaningful reductions in glycaemic parameters but pancreas-selective and pancreas–liver dual-activating
will need added value to meet these increased standards. glucokinase activators (GKAs) and G-protein-coupled
Furthermore, to be competitive against the current ther- receptor 40 (GPCR40) agonists (Table 1). Second are
apies in use, new drugs must distinguish themselves with drugs that utilize the incretin axis (Figs 1,2). These include
additional attributes such as contributing to increased agonists of the GLP1 receptor and glucose-dependent
weight loss, having no increased risk for hypoglycaemia, insulinotropic polypeptide (GIP) receptor, GLP1–gluca-
or utilizing improved drug delivery systems and routes gon receptor agonists, triple GLP1–GIP–glucagon
of administration that might decrease the frequency of receptor agonists, oxyntomodulin, and agonists of
use. This Review generates a comprehensive list of the G-protein-coupled receptor 119 (GPCR119) (Table 2).
novel therapies for T2DM currently in development and Third are drugs that directly or indirectly decrease
discusses their potential for improving care for patients. hepatic glucose production or increase hepatic glucose
uptake (Fig. 2). These drugs include glucagon receptor
Review criteria antagonists, antisense oligonucleotide inhibitors specific
To compile the most comprehensive list of promising, for glucagon receptor mRNA, dual amylin–calcitonin
novel therapies for T2DM, the US National Institute receptor agonists (DACRAs) and liver-selective GKAs
of Health Clinical Trials database was searched from (Table 3). Fourth and finally are drugs that improve
November 26, 2019, to March 31, 2020, using the condi- insulin sensitivity (Fig. 3). These include an antisense
tion or disease term ‘type 2 diabetes’. This query yielded oligonucleotide inhibitor for protein tyrosine phos-
7,484 registered trials worldwide, which were examined phatase 1B (PTP1B) mRNA, fibroblast growth factor 21
individually. The following three exclusion criteria were (FGF21) analogues, a diacylglycerol acetyl transferase 1
applied. First, we excluded drugs in existing classes. (DGAT1) inhibitor and an enterocytic microsomal tri-
Therapies considered ‘novel’ were any medical phar- glyceride transfer protein (MTP) inhibitor. Additional
maceutical therapy not currently approved for T2DM. drugs in this category include novel selective peroxi-
Hence, we excluded new drugs in development within some proliferator-activated receptor (PPAR) agonists,
existing classes (for example, new dipeptidyl peptidase a GLUT4 facilitative transporter stimulator, a nuclear
4 inhibitors) as well as advances in devices or technol- factor-κB (NF-κB) inhibitor, a selective allosteric acti-
ogies related to currently approved medications (for vator of LYN kinase, a nicotinic α7 receptor ligand,
example, oral insulin and inhaled GLP1 receptor ago- a ghrelin analogue, a ghrelin–growth hormone (GH)
nists). Importantly, advances in delivery devices and receptor agonist and an activin II-B receptor modulator
technologies for people with T2DM are expected to lead as well as a drug with an unknown mechanism of action
to improved medication adherence and persistence for (imeglimin) (Table 4).
both existing and emerging therapies. An example of
such devices is ITCA650, a mini-osmotic pump capable Novel agents in development
of continuous subcutaneous delivery of exenatide for up The year 2021 marks the 100th anniversary of the
to 6 months21. discovery of insulin — the very first pharmacological
Second, we excluded therapies tested for their other treatment for diabetes mellitus. Over those 100 years,
physiological properties (for example, insulin sensitiza- 10 distinct classes of drugs have been approved by the
tion but not glucose lowering), tested in disease states FDA for the treatment of T2DM, most of which were
naTure RevIews | EnDoCRinology volume 17 | June 2021 | 365
0123456789();:Reviews
Oxyntomodulin
Glucagon
GLP1 receptor
receptor agonists
agonists Meglitinides
Glucose
GLP1 Glucagon Sulphonylureas
receptor GLUT1/2
receptor
KATP channel
GIPR GIPR (SUR1-Kir6.2)4
Glucokinase Glucokinase
agonists activators
Glucose
cAMP PKA ATP
metabolism K+
GPCR119 Pro-insulin
biosynthesis Mitochondrion
GPCR119
agonists Piccolo Membrane
RIM2 RAB3A depolarization
EPAC2 Insulin
Ca2+
Insulin
granule IP3 PLC
L-type Ca2+
RAP1A Ca2+- dependent channel
and calmodulin-
dependent proteins
GPCR40
PKC DAG agonists
Translocation
GPCR40
Priming
Docking
Fig. 1 | Drugs that stimulate insulin secretion. Drug classes with new drugs in development are shown (blue ovals) as
well as the pathways that they act on in β-cells to stimulate insulin secretion. New drugs include glucokinase activators
(GKAs), which augment glucose-stimulated insulin secretion. Glucokinase (green oval) converts glucose into glucose-6-
phophate. By contrast, G-protein-coupled receptor 40 (GPCR40) agonists act to increase free fatty acid-stimulated insulin
secretion. New drugs that target the incretin axis are also under development, for example, dual and triple incretin mimetics,
such as glucagon-like peptide 1 (GLP1) receptor agonists with a glucose-dependent insulinotropic polypeptide receptor
(GIPR) agonist and/or a glucagon receptor agonist, oxyntomodulin analogues, and G-protein-coupled receptor 119
(GPCR119) agonists. Drugs that act on the incretin axis stimulate glucose-dependent insulin secretion through cAMP
signalling. Also shown are the established type 2 diabetes mellitus therapeutics sulfonylurea and meglitinide (orange
ovals), which bind to SUR1 (part of the ATP-sensitive Kir6.2 potassium channel), increase calcium influx and increase
insulin secretion. Adapted from ref.106, Springer Nature Limited.
approved in the past 20 years22. Despite the explosion deficiency occurs when the pancreas makes insuffi-
in therapeutic options for people with T2DM, the pipe- cient insulin, often in the context of insulin resistance.
line for novel therapies in T2DM remains robust and Interestingly, of the >400 genetic associations with
quite prolific. Companies developing each new therapy T2DM, the majority govern β-cell function23. Genetic
strive for theirs to be novel, first in class and better than, discovery has delivered novel mechanistic insights into
or complimentary to, existing treatments. The goals of disease pathophysiology, including new ways to stim-
novel therapies are to help patients reach their indi- ulate insulin secretion directly from β-cells (Table 1;
vidualized glycaemic targets while optimizing safety, Fig. 1).
non-glycaemic benefits and the prevention of compli-
cations for individual patients who are at risk of specific Glucokinase activators. GKAs are a novel therapy that
complications. directly targets β-cells, with at least 11 drugs under
development (one in phase III, four in phase II and six
Drugs that directly target β-cells in phase I clinical trials) (Table 1). Glucokinase, which
Insulin deficiency is a defining feature of T2DM. facilitates the phosphorylation of glucose to glucose-6-
Absolute insulin deficiency occurs when the pancreas phosphate, functions as the ‘glucose sensor’ of the body,
no longer makes insulin, whereas a relative insulin maintaining plasma concentrations of glucose within a
366 | June 2021 | volume 17 www.nature.com/nrendo
0123456789();:Reviews
narrow range (4–6 nM)24. The action of glucokinase is concentration of triglycerides27–30. Nevertheless, safety
restricted to glucose-sensitive and glucose-responsive issues could be avoidable through careful patient
tissues such as the liver and pancreas. As such, the GKAs selection31 and perhaps liver-s elective GKAs might
in development have been designed to target both liver avoid the increased risk of hypoglycaemia; however, liver
and pancreas (dual) or to be more specific, targeting safety will need to be clearly demonstrated32.
only one tissue (selective)25. Glucokinase activation in
the liver stimulates hepatic glucose uptake and inhib- G-protein-coupled receptor 40. GPCR40 (also known
its hepatic glycogenolysis (Fig. 2), whereas glucokinase as free fatty acid receptor 1; FFAR1) agonists have gen-
activation in the pancreatic β-cell stimulates insulin erated considerable interest as a novel mechanism for
secretion26. Dual GKAs can be further subdivided by direct β-cell stimulation. Agonists of GPCR40 act in the
their enzyme kinetics, which can render them more or β-cell to induce free fatty acid (FFA)-stimulated insulin
less potent to stimulate insulin secretion, thereby under- secretion33 and two agents have advanced into phase II
scoring the customizability of the molecules. Historically, trials. These compounds act as cooperative, allosteric
GKAs have not thrived in development, limited by their modulators of GPCR40 that rely on the ample circulat-
lack of durability, risk of inducing hypoglycaemia, liver ing levels of FFAs to potentiate glucose-dependent insu-
toxicity and ability to cause an increase in the plasma lin secretion34. A previous GPCR40 agonist compound
Table 1 | Drugs that directly stimulate β-cells
Compound Mechanism of action Trial Results Ref. or clinical
phase trial number
GKAs
HMS5552 Dual GKA (pancreas and liver); III 24 people with T2DM randomized 31,103
(dorzagliatin) GKA in pancreatic β-cells to dorzagliatin 75 mg QD or BID for
augments glucose-stimulated 28 days; HbA1c –1.22% with QD and
insulin secretion; GKA in liver –0.79% with BID
increases hepatic glucose
AZD1656 uptake; together, they maintain II 458 people with T2DM randomized 30,104
plasma levels of glucose at to AZD1656 20 mg QD, 40 mg QD,
4–6 nM titrated from 10 mg to 140 mg
QD, titrated from 20 mg to 200 mg QD,
glipizide titrated from 5 mg to 20 mg
QD or placebo for 4 months; HbA1c
–0.80% in the AZD1656 titrated
groups but waned over time
RO4389620 Ib 15 people with T2DM randomized 27,105
(piragliatin) to triple crossover of piragliatin
25 mg, 100 mg or placebo; glucose
AUC during an OGTT at the 100 mg
dose was less than that observed at
the 25 mg dose, which was less than
observed with placebo
PSN-821 I No published data NCT01386099
DS-7309 I No published data NCT01862939,
NCT01956305
PB-201 I No published data NCT03973515
BMS-820132 I No published data NCT01290575,
NCT01105429
LY2608204 I Safety established in phase I trial NCT01247363
Globalagliatin I No published data NCT03414892,
NCT03171623
PF04937319 Systemic partial GKA (weak II 639 people with T2DM randomized 32
pancreatic effects only) to PF04937319 50 mg QD or 100 mg
QD for 12 weeks; HbA1c –0.45%
at 100 mg QD; PK/PD, safety and
add-on studies appear promising
GPCR40 agonists
MK 8666 GPR40 is highly expressed in II 63 people with T2DM randomized 33
pancreatic β-cells; its activation to MK 8666 50 mg QD, 150 mg
by fatty acids amplifies QD, 500 mg QD for 14 days; dose
glucose-dependent insulin dependent 31–54 mg/dl decrease
secretion in fasting plasma glucose
JTT-851 II No published data NCT01699737
AUC, area under the curve; BID, twice daily; GKA, glucokinase activator; GPCR40, G-protein-coupled receptor 40; OGTT, oral
glucose tolerance test; PD, pharmacodynamics; PK, pharmacokinetics; QD, daily; T2DM, type 2 diabetes mellitus.
naTure RevIews | EnDoCRinology volume 17 | June 2021 | 367
0123456789();:Reviews
Liver Islet
Oxyntomodulin Glucagon
receptor
GPCR119 agonists
Glucagon GIPR Glucagon
receptor Glucagon agonists receptor
antagonists
DACRAs
Glucose GLP1
Glucagon receptor antisense receptor
oligonucleotide inhibitors Glucokinase GIPR
Glucagon activators
receptor
Augmented
insulin
secretion Amylin
GLUT1/2 receptor
Increased
Glucagon Adenylate amylin
receptor mRNA cyclase secretion
Glucokinase
β-Cell
cAMP
G-6-P Amylin
Insulin
PKA
Glycogen
• Glycogenolysis
• Gluconeogenesis Hepatocyte
Glucagon
Hepatic glucose secretion
production
α-Cell
Fig. 2 | Drugs that decrease hepatic glucose production or increase hepatic glucose uptake. Glucagon receptor
antagonists and antisense oligonucleotide inhibitors for the glucagon receptor both act directly on hepatocytes to
decrease the hepatic glucose production stimulated by glucagon. By contrast, liver-selective glucokinase activators
increase hepatic glucose uptake. Indirect effects on hepatic glucose metabolism are induced by drugs that act on β-cells.
For example, dual amylin–calcitonin receptor agonists (DACRAs) and drugs targeting the incretin axis (dual or triple
incretin mimetics, oxyntomodulin analogues or G-protein-coupled receptor 199 (GPCR119) receptor agonists) induce
insulin and/or amylin secretion, which inhibits glucagon secretion from α-cells. Decreased circulating levels of glucagon
result in less induction of hepatic glucose production. G-6-P, glucose 6-phosphate; GIPR, glucose-dependent insulinotropic
polypeptide receptor; GLP1, glucagon-like peptide 1.
in development (fasiglifam, also called TAK 875) showed been associated with increased de novo lipogenesis
glucose-lowering properties in phase IIa clinical trials; and subsequent hepatic steatosis36. Furthermore, nat-
however, considerable liver toxicity in phase III trials urally occurring polymorphisms in the glucokinase
led to the termination of its development programme35. regulatory protein have been associated with elevated
Hence, continued vigilance towards safety will dominate plasma levels of triglyceride, FFAs and VLDL cho-
the development of its successors as it is unclear how lesterol in humans37–39. By contrast, studies in animal
these new molecules differ from fasiglifam. models show that the liver toxicity seen with GPCR40
agonists seems to be mediated through disrupted bile
Potential for liver toxicity. The liver toxicity associated acid homeostasis40,41. Taking the liver toxicity data
with drugs that stimulate insulin secretion directly from with GKAs and GPCR40 agonists together, it is clear
β-cells is worth contemplating. Of note, both glucoki- that directly stimulating insulin secretion from the
nase and GPCR40 are expressed in the liver as well as β-cell using drugs that also have actions in the liver
in β-cells. In humans, naturally occurring mutations could lead to untoward alterations in pathways of lipid
leading to hepatic glucokinase overexpression have metabolism.
368 | June 2021 | volume 17 www.nature.com/nrendo
0123456789();:Reviews
Table 2 | Drugs that utilize the incretin axis
Compound Mechanism of action Trial Results Ref. or clinical
phase trial number
Multi-site receptor agonists for GLP1, GIP and/or glucagona
AVE2268 GLP1–GIP–glucagon I No published data NCT00361738
triple receptor agonist
HM12460A GLP1–GIP–glucagon I No published data NCT01724814,
triple receptor agonist NCT03332836
LY3298176 GLP1–GIP dual receptor III 318 people with T2DM randomized to 44
(tirzepatide) agonist tirzepatide 1 mg Q week, 5 mg Q week, 10 mg
Q week, 15 mg Q week, dulaglutide 1.5 mg Q
week or placebo for 26 weeks; HbA1c –1.06%,
–1.73%, –1.89%, –1.94%, –1.21%, –0.06%,
respectively
SAR425899 GLP1–glucagon dual II PK/PD established in 36 people with T2DM 46
receptor agonist
MEDI0382 GLP1–glucagon dual IIa MEDI0382 lowered glucose AUC during a NCT03596177,
receptor agonist MTT versus placebo; PK/PD, safety, add-on NCT03555994,
established in phase I trial NCT03550378,
NCT03745937,
NCT03385369,
NCT02548585,
NCT03341013,
NCT03444584,
NCT03645421,
NCT03244800,
NCT03235050,
NCT04515849,
NCT04208620
Oxyntomodulin analogueb
OPK88003 This oxyntomodulin II No published data NCT03406377
analogue has the
potential actions of a
GLP1–glucagon dual
receptor agonist
GPCR119 agonist
MBX-2982 GPCR119 is highly I No published data NCT01035879
expressed in the human
DS-8500a gastrointestinal tract II 99 people with T2DM randomized to 47,48
(small intestinal L cells) DS-8500a 10 mg QD, 75 mg QD or placebo
and pancreas (β-cells); for 28 days; 24 h mean weighted glucose
the stimulation of measurements decreased by 0.74 mmol/l
GPCR119 has the and 1.05 mmol/l for 10 mg and 75 mg doses,
potential to promote respectively, relative to placebo
glucose-dependent
insulin secretion
AUC, area under the curve; GIP, glucose-dependent insulinotropic polypeptide; GLP1, glucagon-like peptide 1; GPCR119,
G-protein-coupled receptor 119; MTT, meal tolerance test; PD, pharmacodynamics; PK, pharmacokinetics; QD, daily; Q week,
dosed once per week; T2DM, type 2 diabetes mellitus. aGLP1 is secreted by the L cells in the small bowel in response to nutrient
ingestion. Modulated through a complex neural plexus, it augments glucose-dependent insulin secretion, suppresses glucagon
and induces satiety, resulting in weight loss. GIP is secreted by intestinal K cells with food ingestion, has the potential to augment
insulin secretion and has been found to be deficient in people with T2DM. Glucagon has lipolytic and thermogenic capabilities.
The glucose-raising effects of glucagon are constrained when used in combination with GLP1. bOxyntomodulin, like GLP1
and glucagon, is a peptide product derived from the post-translational modification of preproglucagon. It is secreted by the
enteroendocrine cells of the small intestine in response to nutrient ingestion and has been shown in vitro to be a natural chimera,
binding and activating both the GLP1 receptor and the glucagon receptor.
Drugs that utilize the incretin axis of drugs that act on the incretin axis is further amplified
The indirect stimulation of β-cells is achievable through by the ability of incretins to induce weight loss42.
drugs that affect the incretin axis (Table 2; Fig. 2). By defi-
nition, incretin hormones (for example, GLP1 and GIP) Dual-a cting or triple-a cting incretin mimetics.
are hormones secreted by enteroendocrine cells in the Importantly and unlike GKAs and GPCR40 agonists,
gastrointestinal tract in response to the oral ingestion of insulin secretion invoked by incretin mimetics is glu-
nutrients. These hormones act to decrease the plasma cose dependent; that is, the plasma concentrations of
concentrations of glucose by mediating delayed gastric glucose must be elevated or rising for insulin secretion
emptying, augmenting insulin secretion and suppressing to be stimulated. GLP1 receptor agonists have been
glucagon secretion. Of note, the glucose-lowering ability used in T2DM care for the past 15 years to decrease
naTure RevIews | EnDoCRinology volume 17 | June 2021 | 369
0123456789();:Reviews
plasma concentrations of glucose and body weight43 and, rather than the supplementation of GLP1 and GIP is
from 2016, to provide protection from cardiovascular being tested using analogues of GPCR119; one drug
disease13,14. Expanded use of the incretin axis includes is in phase I trials and another is in phase II47,48.
the development of molecules that act as both GLP1 The well-established ability of glucagon to stimulate
receptor agonists and GIP receptor agonists and/or as hepatic glucose production makes it a counterintuitive
glucagon receptor agonists. Such dual or triple agonist choice as a treatment for T2DM. The rationale for inte-
drugs aim to achieve even greater efficacy for glucose grating the pharmacology of GLP1 and glucagon relies
lowering, greater body weight loss and perhaps greater upon the action of GLP1 to restrain the hyperglycae-
cardiovascular protection in patients with T2DM than mic effect of glucagon while adding a centrally medi-
provided by single agonists. ated anorectic action to synergize with the lipolytic and
In addition to their role in treating T2DM, dual- thermogenic capabilities of glucagon with the aim to
acting or triple-a cting agonists have the potential substantially decrease body weight49.
to attain independent indications for obesity, sleep
apnoea, renal insufficiency, non-alcoholic fatty liver Oxyntomodulin analogues. Oxyntomodulin, like GLP1
disease (NAFLD) and non-alcoholic steatohepatitis in and glucagon, is a peptide product derived from the
people with or without T2DM. Currently, drugs in clin- post-t ranslational modification of preproglucagon.
ical trials include one dual-acting GLP1–GIP receptor Oxyntomodulin is secreted by the enteroendocrine
agonist in phase III44, two dual-acting GLP1–glucagon cells of the small intestine in response to nutrient inges-
receptor agonists in phase II45,46, and two triple-acting tion and has been shown in vitro to be a natural chi-
GLP1–GIP–glucagon receptor agonists in phase I trials mera, binding and activating both GLP1 and glucagon
(Table 2). The clinical rationale for combining these receptors50. The dual stimulation of GLP1 and gluca
dual-acting or triple-acting peptides is mainly to poten- gon receptors is currently being tested for T2DM using
tiate the weight loss effects as it is unlikely that the HbA1c an analogue of oxyntomodulin (one drug in phase II
reductions observed will be much greater than the trials)50. Similar to dual-acting GLP1–glucagon recep-
1.5% or even 2% that have already been achieved with tor agonists, oxyntomodulin exerts its glucoregulatory
compounds like semaglutide (approved) or tirzepatide actions independent of but in addition to considerable
(phase III), respectively. In addition, the stimulation weight loss50.
Table 3 | Drugs that modulate hepatic glucose metabolism
Compound Mechanism of action Trial Results Ref. or clinical
phase trial number
Glucagon receptor antagonist
LGD-6972 Inhibits glucagon action II PK/PD established 54
REMD-477 I–II No published data NCT02455011
Antisense oligonucleotide inhibitor for the glucagon receptor
ISIS-449884 (GCGRRx) Inhibits hepatic glucagon II Three phase II randomized, 55
receptor expression and double-blind studies exposed
hepatic glycogenolysis people with T2DM to
ISIS-449884 50–200 mg SC
weekly for 13–26 weeks; HbA1c
–0.9% to 2.0% with the various
doses and a dose-dependent
increase in transaminases was
observed
DACRAs
KBP-042 Calcitonin stimulates II No published data NCT03230786
amylin secretion; amylin
KBP089 lowers glucose levels I No published data NCT03907202
through delayed gastric
emptying and suppressing
glucagon secretion
GKAs
PF-04991532 Liver-selective GKA; GKA II PK/PD, safety established in NCT01129258,
in liver increases hepatic T2DM NCT01469065,
glucose uptake NCT01336738,
NCT01338870,
NCT01369602
GK1-399 (formerly Liver-selective GKA II No published data NCT01474083,
TTP399) NCT02405260,
NCT01474083
DACRA, dual amylin–calcitonin receptor agonist; GKA, glucokinase activator; PD, pharmacodynamics; PK, pharmacokinetics;
SC, subcutaneous; T2DM, type 2 diabetes mellitus.
370 | June 2021 | volume 17 www.nature.com/nrendo
0123456789();:Reviews
The therapeutic potential of the incretin axis. Whether incretin axis is not only being pursued for the treatment
by a new dual or triple agonist therapy or by established of T2DM but also for the treatment of NAFLD and non-
GLP1 receptor agonists, the utilization of the incre- alcoholic steatohepatitis51,52. Without question, the sub-
tin axis holds particular promise for the treatment of stantial weight loss observed with these novel therapies
T2DM and its common comorbidities. As mentioned is responsible for much of their metabolic benefits and
previously, the indirect, glucose-dependent stimulation probably extends to non-metabolic benefits as well (for
of insulin secretion avoids the hypoglycaemia and dis- example, improvements in sleep apnoea and mobility).
rupted lipid metabolism that are seen with GKAs and Furthermore, expanded use of the incretin axis for ther-
GPCR40 agonists. By contrast, expanded use of the apeutic purposes has provided unique insights into the
Insulin Liver Muscle
GH–ghrelin Ghrelin
PTP1B antisense co-agonist analogue
oligonucleotide Glucagon LYN kinase
inhibitors Insulin Glucagon Glucose activator
receptor receptor
GLUT2 GLUT4
GH receptor
PTP1B mRNA ATP cAMP LYN kinase
γ β
PIP2
PTP1B IRS1/2 PI3K ↓ G6Pase αq
Mitochondrion Translocation
PIP3 ↓ FBPase
PKB PDK1/2 Pyruvate
ATP:AMP PLC
GLUT4
LKB facilitative
transporter Synaptic
AMPK vesicle
stimulator
ACC
Glucose
uptake
mTORC1 MAPK cascade
• Gluconeogenesis Transcription of genes ↑ Glucose uptake, Ca2+ influx
• Lipid synthesis involved in energy metabolism and
• Lactate production storage and expenditure glycolysis
Endoplasmic
reticulum
PPAR agonists
PPARs RXR
Hepatocyte or muscle cell
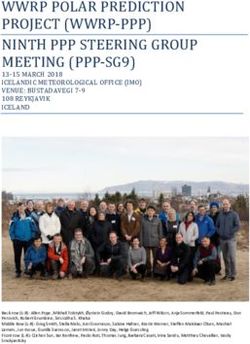
Fig. 3 | Drugs that improve insulin sensitivity. Several new drugs are in action of these drugs is not fully understood but they are thought to
development that improve insulin sensitivity through various mechanisms increase endoplasmic reticulum calcium influx, thereby stimulating
of action. For example, the antisense oligonucleotide inhibitor specific for physiological IGF1 production in the liver, which in turn increases insulin
protein tyrosine phosphatase 1B (PTP1B) mRNA disinhibits insulin signalling action. Not shown on the figure are agents that target fibroblast growth
by reducing the translation of the negative regulator PTP1B. Furthermore, factor 21 (FGF21) or inhibit diacylglycerol acetyl transferase 1 (DGAT1) and
novel peroxisome proliferator-activated receptor (PPAR) agonists are being microsomal triglyceride transfer protein (MTP). These drugs all act as
developed that stimulate the transcription of genes involved in energy presumed insulin sensitizers through altering lipid metabolism. In addition,
storage and expenditure. In skeletal muscle, a selective allosteric activator an agent targeting the type II B activin receptor is also thought to be an
of LYN kinase and a glucose transporter type 4 (GLUT4) facilitative insulin sensitizer through an unknown mechanism. Anti-inflammatory
transporter stimulator both act to increase the translocation of GLUT4 to agents, including a nuclear factor-κB (NF-κB) inhibitor and agent that
the plasma membrane. Finally, a ghrelin analogue and ghrelin–growth upregulates the nicotinic α7 receptor, are also in development. Adapted
hormone (GH) receptor agonist have been developed; the mechanism of from ref.106, Springer Nature Limited.
naTure RevIews | EnDoCRinology volume 17 | June 2021 | 371
0123456789();:Reviews
Table 4 | Drugs that improve insulin sensitivity
Compound Mechanism of action Trial Results Ref. or clinical
phase trial number
Antisense oligonucleotide inhibitor for PTP1B mRNA
ISIS 113715 PTP1B has been shown to be a negative III 92 people with T2DM randomized to ISIS 83
(IONIS-PTP-1BRx) regulator of insulin and leptin signalling; 113715 200 mg SC Q week or placebo for
the inhibition of PTP1B enhances insulin 26 weeks; HbA1c –0.44% with ISIS 113715
and leptin action
FGF21 analogue
LY2405319 FGF21 has been shown to improve whole I 47 people with T2DM randomized to 66
body insulin sensitivity, enhance insulin LY2405319 at 3 mg, 10 mg or 20 mg QD for
secretion while suppressing glucagon 28 days; LY2405319 lowered LDL-cholesterol,
secretion, inhibit hepatic lipogenesis, triglycerides, fasting insulin and body weight
and increase energy expenditure via the while increasing adiponectin but little effect
activation of brown adipose tissue on plasma concentrations of glucose was
observed
SRT2379 I No published data NCT01018628
SAR425899 I No published data NCT03414736,
NCT02973321,
NCT02411825
DGAT1 inhibitor
PF-04620110 Inhibits the acetylation of diacylglycerol I PK/PD established in T2DM NCT01298518
to triacylglycerol; the ectopic deposition
of triacylglycerol has been linked to
insulin resistance
Enterocytic MTP inhibitor
KD026 (SLx-4090) Inhibits the production of apo B II No published data NCT02434744,
containing lipoproteins in the gut; NCT00871936,
by-products stimulate insulin signalling NCT02434744
independent of the insulin receptor
Novel PPAR agonists
CS038 (chiglitazar) Dual PPARα/γ agonist; intranuclear III No published data NCT02173457,
transcription factors that lower plasma NCT02121717
levels of triglycerides and differentiate
preadipocytes into mature adipocytes,
respectively
T0903131 (formerly Partial PPARγ agonist; weak intranuclear I 367 people with T2DM randomized to NCT00952445,
INT-131; besylate) transcription factor that differentiates T0903131 0.5 mg, 1 mg, 2 mg or 3 mg QD NCT00631007
pre-adipocytes into mature adipocytes versus placebo for 24 weeks; dose-dependent
HbA1c –0.3% to –1.0% in T0903131
Other mechanisms
DS-1150b GLUT4 facilitative transporter stimulator; I No published data NCT02004678
improves insulin signalling
CAT-1004 (edasalonexent) Anti-inflammatory I No published data NCT01511900
MLR-1023 (tolimidone) Selective allosteric activator of LYN I No published data NCT03279263,
kinase; improves insulin signalling NCT02317796
TC-6987 Nicotinic α7 receptor ligand; II No published data NCT01293669
anti-inflammatory
AZP-531 (livoletide) Ghrelin analogue; inhibits food intake 1 No published data NCT02040012
and induces weight loss
TH-9507 (tesamorelin Ghrelin–GH receptor agonist; 2 53 people with T2DM randomized to TH-9507 NCT01264497
or Egrifta) GH-releasing hormone analogue; 1 mg or 2 mg SC QD or placebo for 12 weeks;
decreases visceral adipose tissue no difference in HbA1c was observed74
accumulation
S707106 Unknown mechanism of action 2 No published data NCT01154348,
NCT01240759
Bimagrumab Type II-B activin receptor modulator; 2 No published data NCT03005288
activates muscle growth (ref.80)
DGAT1, diacylglycerol acetyl transferase 1; FGF21, fibroblast growth factor 21; GH, growth hormone; MTP, microsomal triglyceride transfer protein; PD,
pharmacodynamics; PK, pharmacokinetics; PPAR, peroxisome proliferator-activated receptor; PTP1B, protein tyrosine phosphatase 1B; QD, daily; Q week, dosed
once per week; SC, subcutaneous; T2DM, type 2 diabetes mellitus.
372 | June 2021 | volume 17 www.nature.com/nrendo
0123456789();:Reviews
complex interplay between diet, enteroendocrine cells tissue-selective but could be designed to be so. Proven
and the microbiome in human health and disease53. safety with DACRAs would strengthen this hypothesis,
Collectively, the knowledge to be gained from and the particularly if neither hypoglycaemia nor liver toxicity
therapeutic potential of the incretin axis is vast. are observed. The development of partial and/or tissue-
selective glucagon receptor antagonists might prove a
Drugs targeting metabolism in the liver worthy pursuit.
Plasma levels of glucose can be decreased using thera-
peutics that target glucose metabolism in the liver. These Drugs that improve insulin sensitivity
agents can target the liver directly, either by modulating Perhaps the greatest need for new therapies in T2DM
the action of glucagon in hepatocytes to reduce hepatic falls in the area of insulin sensitization and the
glucose production or by activating glucokinase to approaches of the pharmaceutical industry to meeting
increase glucose uptake by hepatocytes. Alternatively, this need could not be more diverse. Unfortunately, most
these drugs can reduce glucagon secretion from islets, of these approaches to date do not seem particularly
thereby indirectly reducing hepatic glucose production promising for decreasing levels of glucose in patients
(Table 3; Fig. 2). with T2DM (Table 4; Fig. 3).
Antagonizing glucagon action. Whether endogenous Targeting FGF21. Considerable interest has been
or exogenous, glucagon induces hepatic glycogenolysis shown in FGF21, a hepatokine that activates the NAD-
leading to a rapid increase in plasma concentrations of dependent protein deacetylase sirtuin 1 (three drugs are
glucose. Thus, it is conceivable that blocking the actions currently in phase I trials) (Table 4). FGF21 is thought
of glucagon might lead to improved glucose control. to be an insulin sensitizer through its ability to mitigate
As a single agent, glucagon action in patients with T2DM FFA-induced insulin resistance60. Collectively, investiga-
must be antagonized so as to not exacerbate hypergly- tions have revealed FGF21 as a stimulator of fatty acid
caemia. Indeed, this strategy is being approached in a oxidation, particularly in the liver, that increases the
number of ways; for example, two drugs that are direct production of ketone bodies and inhibits lipogenesis61,62.
glucagon receptor antagonists are currently in phase II Despite reports of circulating levels of FGF21 being
trials54. Furthermore, RNA interference gene therapy has higher in people with any combination of T2DM63,
been utilized for this purpose through the creation of NAFLD64 or obesity than in individuals without these
an antisense oligonucleotide inhibitor for the glucagon conditions, people treated with FGF21 analogues show
receptor (one drug is in a phase II trial)55. The use of weight loss65. Nevertheless, a proof-of-concept study
antisense RNA antagonizes the action of glucagon by in people with T2DM treated with FGF21 analogues
blocking the transcription of the gene that encodes the observed a decrease in the plasma levels of lipids but
glucagon receptor. not in plasma concentrations of glucose66.
Another strategy to indirectly target the hepatic
actions of glucagon involves the use of a DACRA (one Inhibitors of DGAT1 and MTP. One inhibitor of DGAT1
drug is in a phase I trial and another is in a phase II trial) is currently in phase I trials and one inhibitor of MTP
(Table 3). The rationale for DACRAs stems from using is in phase II trials. The rationale for developing these
the action of calcitonin to stimulate the amylin recep- agents lies in the assumption that altering lipid metabo-
tor on β-cells leading to the co-secretion of amylin and lism will favourably affect glucose metabolism. However,
insulin. Amylin itself decreases blood concentrations preclinical studies have yet to show that this scenario
of glucose by delaying gastric emptying56 as well as by is the case67,68 and there might be reason to suspect
inhibiting post-prandial glucagon secretion57. Although that a glucose-lowering ability by these drugs will not
each agent in this group has demonstrated promise in be demonstrated after all. For example, the inhibition
decreasing levels of glucose in humans, their specific of DGAT1 might indeed decrease the tissue accumu-
effect on suppressing hepatic glucose production, per se, lation of triacylglycerol (aka triglyceride); however,
is presumptive and is yet to be clearly proven. it does so at the expense of an increased tissue accumu-
lation of diacylglycerol, which is a far more inflamma-
Safety issues. Unfortunately, an increase in hepatic tory, insulin de-sensitizing lipid than triacylglycerol69,70.
steatosis and blood biomarkers of liver injury (transam- Moreover, MTP acts in the liver and intestine to pre-
inases) have been reported in clinical trials with the vent the transfer of triglycerides to other apo-B con-
antisense oligonucleotide inhibitor as well as after direct taining lipoproteins, thereby reducing post-prandial
antagonism of the glucagon receptor58,59. These safety hypertriglyceridaemia71,72. Nevertheless, a link is lack-
concerns have led to the abandonment of a number of ing between decreasing plasma levels of triglycerides and
compounds in development (for example, Bay 27-9955, insulin sensitization and/or decreases in plasma levels of
MK-0893, MK-3577 and LY-24090215). Most note- glucose in humans73.
worthy is that the inhibition of hepatic glycogenolysis,
whether by glucagon antagonism, GKAs or GPCR40 Targeting the GH receptor. Speculation exists as to
agonists, increases hepatic de novo lipogenesis. The whether the adverse effects of GH on glucose metabo-
physiological nature of this response is predictable but lism might be offset by its anabolic action as well as by its
could be avoidable, for example, by developing tissue- ability to stimulate the production of insulin-like growth
selective drugs that avoid the liver. To date, gluca- factor 1 in the liver. The gastric-derived peptide, ghre-
gon receptor antagonists in development are not lin, is an endogenous ligand for GH-releasing hormone
naTure RevIews | EnDoCRinology volume 17 | June 2021 | 373
0123456789();:Reviews
receptor. GH receptor agonism can be achieved either insulin receptor substrate 1 in insulin-responsive tissues,
directly using a GH–ghrelin receptor co-agonist74 (one which in return phosphorylates LYN kinase, suggesting
drug in phase II trials) or indirectly using a pure ghre- a regulatory feedback loop between LYN kinase and
lin analogue75 (one drug in phase I trials) (Table 4). The insulin receptor activation84. Interestingly, the insulin
potentiation of GH via ghrelin is unlikely to thrive in secretagogue, glimepiride, harbours extra pancreatic
development as a treatment for T2DM owing to the ina- action as an insulin sensitizer through the activation
bility of this mechanism to induce weight loss76,77 and of LYN kinase; however, glimepiride is associated with
blunting of glucose-stimulated insulin secretion78. hypoglycaemia85. By contrast, hypoglycaemia has not
The anabolic action of GH might be better achieved been reported with the upregulation of insulin sig-
with a more direct approach such as type II-B activin nalling in peripheral tissues by other compounds that
receptor modulation (one drug in phase II trials). specifically target LYN kinase currently in development.
Blockade of the type II-B activin receptor inhibits the
actions of natural ligands that negatively regulate skeletal PPAR agonists. The pipeline also revisits PPAR ago-
muscle growth, thereby leading to a preservation and nists, striving to improve their efficacy and safety, either
even expansion of lean mass79. Bimagrumab, a monoclo- through dual PPARα–PPARγ agonism86 (one drug in
nal antibody that inhibits the activin type II receptor, was phase III trials) or through partial dual PPARα–PPARγ
shown in 2021 to increase lean mass, decrease fat mass agonism (one drug in phase I trials) (Table 4). PPARα
and improve HbA1c in adults with T2DM80. Although the agonists inhibit hepatic lipoprotein C-III expression and
precise mechanism of action remains largely unknown, subsequent VLDL production, making them useful as
it is clear that the anabolic action of bimagrumab is single agents for decreasing plasma levels of triglyceride
distinct from GH and harbours favourable effects on (for example, gemfibrozil and fenofibrate are approved
glucose metabolism. for this indication). PPARγ agonists act as intranuclear
transcription factors that improve insulin sensitivity
Strategies that target inflammation. Insulin resistance is by expanding subcutaneous adipose tissue depots and
widely regarded as a pro-inflammatory state, although inducing the differentiation of pre-adipocytes into
it is unclear whether a unidirectional causative pathway mature adipocytes (for example, rosiglitazone and pio-
exists or whether insulin resistance and inflammation glitazone)87. Contemporary clinical trials have eased
are simply associated. Approaches targeting inflam- historic concerns over the cardiovascular safety of
mation are attractive for their widespread benefits some PPARγ single agonists88. However, thus far, none
on diabetes-related complications but are too early in of the dual PPARα–PPARγ agonists has followed suit
development to understand their efficacy and safety with numerous development programmes halted owing
in T2DM. For example, the TINSAL trials (Targeting to renal and cardiovascular concerns (for example,
Inflammation Using Salsalate in Type 2 Diabetes) exten- aleglitazar89, muraglitazar90 and tesaglitazar91).
sively explored the role of the anti-inflammatory agent Altogether, pharmaceuticals in development for
salsalate as a treatment for T2DM. Results from these tri- T2DM mainly directly or indirectly exploit one of the
als demonstrated HbA1c reduction but also raised safety original ‘triumvirate’ of defects, that is, impaired insu-
concerns that precluded the introduction of salsalate lin secretion, reduced insulin sensitivity and increased
to the market as an anti-diabetic agent81,82. New com- hepatic glucose production, described in T2DM many
pounds in the pipeline include a drug in phase I trials years ago92. One agent in phase III clinical trials is
that inhibits NF-κ B as well as a drug in phase II imeglimin, a tetrahydrotriazine-containing oxidative
trials that upregulates the nicotinic α7 receptor (Table 4). phosphorylation blocker that might attend to the entire
The anti-inflammatory mechanisms of action of these triumvirate: stimulating insulin secretion, improving
compounds in development clearly differ from that of insulin sensitivity and reducing hepatic glucose pro-
salsalate (inhibiting NF-κB or activating the nicotinic α7 duction through the enhancement of mitochondrial
receptor ligand versus inhibiting cyclooxygenase) but are bioenergetics93–96. However, the data remain highly
also likely to exert systemic effects. controversial.
Revisiting existing strategies. Remaining novel com- Future directions
pounds in development for insulin sensitization for the In reviewing the 7,484 trials registered in ClinicalTrials.gov
purpose of decreasing blood concentrations of glucose that were generated using the key word ‘type 2 diabe-
in T2DM reminisce on existing themes. One approach tes’, 43 novel therapies were identified. Through unique
seeks to upregulate insulin signalling in peripheral tis- mechanisms of action that directly stimulate insulin
sues by inhibiting dephosphorylation of the insulin secretion in the β-cell, utilize the incretin axis, suppress
receptor using an antisense oligonucleotide inhibitor for hepatic glucose production and/or improve insulin sen-
PTP1B mRNA (one drug in phase III trials)83. A second sitivity, several recurring themes dominate the potential
approach seeks to completely bypass glucose dependency of these novel therapies to move into clinical care. First,
by stimulating the translocation of the insulin-dependent clinical trials continue to reveal important safety signals,
glucose facilitative transporter (GLUT4) directly (one most notably liver toxicity. Given the exquisite ability of
drug in phase I trials) (Table 4). A third strategy aims at the human body to shift substrate utilization and storage,
the indirect potentiation of insulin action through the it is clearly important to recognize that the mechanism
allosteric activation of LYN kinase (one drug in phase I by which one decreases plasma concentrations of glu-
trials) (Fig. 3). Activated LYN kinase can phosphorylate cose in T2DM is probably as important as the absolute
374 | June 2021 | volume 17 www.nature.com/nrendo
0123456789();:Reviews
decrease achieved. For example, drugs in development patient characteristics, risk of complications and expo-
that block hepatic glucose output decrease plasma lev- sure to glucose-lowering medications97. Several genetic
els of glucose at the expense of hepatic steatosis. Future variants and genetic risk scores were differentially
compounds could avoid these issues if designed to be associated with the clusters; however, they were not
tissue selective. Second, dual and triple agonist thera- examined for their independent association with com-
pies harbour the potential to minimize adverse effects plications or drug exposure. Of note, genetic variabil-
as smaller doses can be used and the different agonists ity has been shown to alter the responses of patients to
can also exert synergistic effects with each other. This sulfonylureas99, metformin100 and thiazolidinediones101,
advantage is best exemplified by compounds in develop- suggesting that the same might be true for the newer and
ment that utilize the incretin axis. Incretin-induced insu- emerging medical therapies. Most importantly, future
lin secretion is indirect and glucose dependent, thereby studies could unveil genetic predictors of patients with
avoiding unnecessary hypoglycaemia while invoking the an improved response to a glucose-lowering medication
gut microbiome and its metabolites to diversify the drug as well as of patients who are likely to have complications
response53. Most certainly, therapies that facilitate weight prevented by such medications. Fortunately, comprehen-
loss will treat much more than T2DM. sive modelling approaches are under way102 to bring this
collective science from the bench to the bedside.
Precision mechanisms
As the treatments for T2DM continue to diversify, our Conclusions
ability to deliver precision health care is becoming real- Novel therapies currently in development for the treat-
ized; drugs with different mechanisms of action can be ment of T2DM directly stimulate insulin secretion in
combined to produce the best possible treatment out- the β-cell, utilize the incretin axis, suppress hepatic glu-
comes in individual patients. Undoubtedly, guidelines cose production and/or improve insulin sensitivity via
will continue to integrate emerging data that focus on unique mechanisms of action. In our judgement, com-
reaching individualized glycaemic targets while optimiz- pounds with the most promise — by virtue of validated
ing safety, non-glycaemic benefits, and the prevention mechanisms of action and advancement in clinical trials
of microvascular and macrovascular complications for by meeting preliminary efficacy and safety end points
individual patients at risk of specific complications20. — include dual-acting GLP1–GIP receptor agonists,
To achieve these aims, considerable work is under way to dual-acting GLP1–glucagon receptor agonists, and
predict which patients are most likely to benefit from the perhaps triple-acting GLP1–GIP–glucagon receptor ago-
various non-glycaemic effects and prevention of specific nists and oxyntomodulin. Each is fully expected to attain
complications. individualized glycaemic targets while optimizing safety,
Revelations have come from both clinical biomarkers off-target benefits and the prevention of complications,
and phenotyping97, as well as from pharmacogenomics98. thereby fuelling hope that they might also treat a host of
For example, one data-driven cluster analysis of nearly obesity-related complications beyond T2DM.
9,000 people with new-onset T2DM identified five rep-
licable phenotypic clusters with substantially different Published online 4 May 2021
1. National Diabetes Data Group. Classification and 10. Nissen, S. E. & Wolski, K. Effect of rosiglitazone the American Diabetes Association (ADA) and the
diagnosis of diabetes mellitus and other categories of on the risk of myocardial infarction and death European Association for the Study of Diabetes
glucose intolerance. Diabetes 28, 1039–1057 (1979). from cardiovascular causes. N. Engl. J. Med. 356, (EASD). Diabetes Care 41, 2669–2701 (2018).
2. World Health Organization. Report of the Expert 2457–2471 (2007). 21. Rosenstock, J. et al. Efficacy and safety of ITCA 650,
Committee on Diabetes. WHO https://apps.who.int/ 11. Gerstein, H. C. et al. Dulaglutide and cardiovascular a novel drug-device GLP-1 receptor agonist, in type 2
iris/handle/10665/41399 (1980). outcomes in type 2 diabetes (REWIND): a double- diabetes uncontrolled with oral antidiabetes drugs:
3. The Diabetes Control and Complications Trial blind, randomised placebo-controlled trial. Lancet the FREEDOM-1 trial. Diabetes Care 41, 333–340
Research Group et al. The effect of intensive treatment 394, 121–130 (2019). (2018).
of diabetes on the development and progression of 12. Hernandez, A. F. et al. Albiglutide and cardiovascular 22. American Diabetes Association. Pharmacologic
long-term complications in insulin-dependent diabetes outcomes in patients with type 2 diabetes and approaches to glycemic treatment: standards of
mellitus. N. Engl. J. Med. 329, 977–986 (1993). cardiovascular disease (Harmony Outcomes): medical care in diabetes-2019. Diabetes Care 42,
4. UK Prospective Diabetes Study (UKPDS) Group. a double-blind, randomised placebo-controlled trial. S90–S102 (2019).
Intensive blood-glucose control with sulphonylureas Lancet 392, 1519–1529 (2018). 23. Mahajan, A. et al. Fine-mapping type 2 diabetes
or insulin compared with conventional treatment 13. Marso, S. P. et al. Semaglutide and cardiovascular loci to single-variant resolution using high-density
and risk of complications in patients with type 2 outcomes in patients with type 2 diabetes. N. Engl. imputation and islet-specific epigenome maps.
diabetes (UKPDS 33). Lancet 352, 837–853 (1998). J. Med. 375, 1834–1844 (2016). Nat. Genet. 50, 1505–1513 (2018).
5. Action to Control Cardiovascular Risk in Diabetes 14. Marso, S. P. et al. Liraglutide and cardiovascular 24. Zelent, D. et al. Glucokinase and glucose homeostasis:
Study Group et al. Effects of intensive glucose lowering outcomes in type 2 diabetes. N. Engl. J. Med. 375, proven concepts and new ideas. Biochem. Soc. Trans.
in type 2 diabetes. N. Engl. J. Med. 358, 2545–2559 311–322 (2016). 33, 306–310 (2005).
(2008). 15. Neal, B. et al. Canagliflozin and cardiovascular and 25. Matschinsky, F. M. Assessing the potential of
6. Duckworth, W. et al. Glucose control and vascular renal events in type 2 diabetes. N. Engl. J. Med. 377, glucokinase activators in diabetes therapy. Nat. Rev.
complications in veterans with type 2 diabetes. 644–657 (2017). Drug Discov. 8, 399–416 (2009).
N. Engl. J. Med. 360, 129–139 (2009). 16. Wiviott, S. D. et al. Dapagliflozin and cardiovascular 26. Matschinsky, F. M. & Wilson, D. F. The central role of
7. The ADVANCE Collaborative Group et al. Intensive outcomes in type 2 diabetes. N. Engl. J. Med. 380, glucokinase in glucose homeostasis: a perspective
blood glucose control and vascular outcomes in 347–357 (2019). 50 years after demonstrating the presence of the enzyme
patients with type 2 diabetes. N. Engl. J. Med. 358, 17. Zinman, B. et al. Empagliflozin, cardiovascular in islets of Langerhans. Front. Physiol. 10, 148 (2019).
2560–2572 (2008). outcomes, and mortality in type 2 diabetes. N. Engl. 27. Bonadonna, R. C. et al. Piragliatin (RO4389620),
8. American Diabetes Association. Glycemic targets: J. Med. 373, 2117–2128 (2015). a novel glucokinase activator, lowers plasma glucose
standards of medical care in diabetes-2020. 18. McMurray, J. J. V. et al. Dapagliflozin in patients with both in the postabsorptive state and after a
Diabetes Care 43 (Suppl. 1), S66–S76 (2020). heart failure and reduced ejection fraction. N. Engl. glucose challenge in patients with type 2 diabetes
9. Garber, A. J. et al. Consensus statement by the J. Med. 381, 1995–2008 (2019). mellitus: a mechanistic study. J. Clin. Endocrinol.
American Association of Clinical Endocrinologists 19. Packer, M. et al. Cardiovascular and renal outcomes Metab. 95, 5028–5036 (2010).
and American College of Endocrinology on the with empagliflozin in heart failure. N. Engl. J. Med. 28. Katz, L. et al. AMG 151 (ARRY-403), a novel
comprehensive type 2 diabetes management 383, 1413–1424 (2020). glucokinase activator, decreases fasting and
algorithm - 2019 executive summary. Endocr. Pract. 20. Davies, M. J. et al. Management of hyperglycemia postprandial glycaemia in patients with type 2
25, 69–100 (2019). in type 2 diabetes, 2018. A consensus report by diabetes. Diabetes Obes. Metab. 18, 191–195 (2016).
naTure RevIews | EnDoCRinology volume 17 | June 2021 | 375
0123456789();:You can also read