Are Serial BNP Measurements Useful in Heart Failure Management?
←
→
Page content transcription
If your browser does not render page correctly, please read the page content below
Controversies in
Cardiovascular Medicine
Are Serial BNP Measurements Useful
in Heart Failure Management?
Serial Natriuretic Peptide Measurements Are Not Useful in
Heart Failure Management: The Art of Medicine
Remains Long
Akshay S. Desai, MD, MPH
N atriuretic peptides, including B-type natriuretic pep-
tide (BNP) and N-terminal-proBNP (NT-proBNP),
have emerged as powerful markers of cardiovascular risk in
strong predictors of the risk for death or hospital readmission
at 6 months.8,10,11
In addition to their association with risk for adverse car-
patients with heart failure.1 Circulating natriuretic peptide diovascular outcomes, circulating levels of NP appear to
(NP) levels add incremental prognostic value to standard vary in relationship to the biology of heart failure progres-
clinical risk stratification algorithms for both ambulatory and sion. NP levels tend to rise during acute heart failure decom-
hospitalized heart failure patients, with a steady increase in pensation and to fall with successful treatment in a pattern
the risk of mortality and recurrent heart failure hospitalization that mirrors reductions in filling pressure, improvements in
as NT-proBNP levels rise above 1000 pg/mL.2–5 A systematic left ventricular structure and function,12 and improvements
review of 19 studies of patients with heart failure demon- in functional capacity.13 Therapies with proven benefit in
strated that for every 100-pg/mL rise in BNP concentration, heart failure patients with reduced ejection fraction, includ-
there was a corresponding 35% increase in the relative risk ing angiotensin-converting enzyme inhibitors,14 angiotensin
of death.6 receptor blockers,15 spironolactone,16 β-blockers,17 and car-
diac resynchronization therapy,18 appear to reduce NP levels
Response by Januzzi and Troughton on p 516
in parallel with improvements in cardiac remodeling and clini-
Beyond the prognostic value of a single NP measurement, cal outcomes.
changes in NP concentrations over time may help to further The prognostic importance of NP levels and their potential
stratify risk.2,7 Reductions in NP levels, whether achieved for modulation with treatment have fueled interest in the use
spontaneously or through application of appropriate medical of serial NP measurements to guide heart failure therapy. The
therapy, appear to be associated with improvement in clinical fundamental premise is an alluring one: that patients with
outcomes.8,9 In the Valsartan Heart Failure Trial, subjects with high biomarker levels (and therefore high risk for adverse
the largest proportional reductions in BNP levels at 4 months outcomes) should receive more intensive disease-modifying
after randomization experienced the best outcomes, whereas therapy and those with low or normal biomarker levels (low
those with the greatest increase in BNP levels experienced risk) should receive less intensive treatment. Advocates of this
the highest event rates.7 Among patients hospitalized with approach highlight the substantial residual risk for heart failure
decompensated heart failure, both predischarge NP levels and hospitalization and death in even well-managed populations,
the relative change in NP levels during hospital treatment are the lack of adherence to guidelines recommending titration
The opinions expressed in this article are not necessarily those of the editors or of the American Heart Association.
From Brigham and Women’s Hospital, Boston, MA.
This article is Part II of a 2-part article. Part I appears on p 500.
Correspondence to Akshay S. Desai, MD, MPH, Cardiovascular Division, Brigham and Women’s Hospital, 75 Francis St, Boston, MA 02115.
E-mail adesai@partners.org
(Circulation. 2013;127:509-516.)
© 2013 American Heart Association, Inc.
Circulation is available at http://circ.ahajournals.org DOI: 10.1161/CIRCULATIONAHA.112.120493
509
Downloaded from http://circ.ahajournals.org/ by guest on May 17, 2015510 Circulation January 29, 2013
of neurohormonal antagonists to maximally tolerated doses, by comparing measured biomarker values with a reference
the inability of many practitioners to reliably estimate filling benchmark. The success of an NP-driven strategy turns heav-
pressures or to recognize the signs/symptoms of clinical ily, therefore, on identification of the appropriate BNP or
decompensation, and the limited sensitivity of weights and NT-proBNP target. Clinical trials of NP-guided therapy have
vital signs for monitoring heart failure progression. The hope generally tested 1 of 2 general approaches: a uniform strategy
is that by providing an objective and responsive measure of in which treatment for all patients is adjusted to target a single
heart failure severity, NP levels will prompt providers to titrate absolute level of BNP or NT-proBNP or an individualized
disease-modifying heart failure therapies more appropriately strategy in which different targets are defined for different
and to improve clinical outcomes. patients based on a measured baseline value.
Identification of a single NP target for all heart failure
Risk Marker or Therapeutic Target? patients is challenging. Levels of BNP and NT-proBNP
Implementation of an effective biomarker-guided strategy vary in relation to heart failure severity but may also be
depends on fulfillment of 4 basic assumptions. First, a clini- influenced by several other factors. Age,35 sex,36 body mass
cally relevant biomarker target must be easily defined for each index,37 and genetic factors38–40 are important confounders,
patient. Second, a therapeutic strategy to adjust biomarker as are concomitant conditions such as atrial fibrillation,
levels to reach the target should be available. Third, the addi- pulmonary hypertension, myocardial ischemia, pulmonary
tional treatments triggered by serial biomarker assessments embolism, and chronic kidney disease.41 Patients with heart
should improve clinical outcomes. Finally, to be truly valu- failure and preserved EF tend to have lower NP levels than
able, a biomarker-driven treatment strategy must provide dif- those with heart failure and reduced EF, even when the
ferent content and superior benefits compared with routine severity of heart failure is similar.42 Furthermore, NP levels
heart failure management guided by the clinical assessment. correlate imperfectly with measured filling pressures43,44 and
Even the most potent markers of cardiovascular risk may remain elevated in those with more advanced or end-
are not necessarily suitable targets for therapy. The serum stage disease even in the absence of significant congestion.11
sodium concentration varies in parallel with heart failure The marked interpatient and intrapatient variability of NP
severity and the degree of neurohormonal activation and is levels has substantially limited the utility of these assays
an accurate predictor of short- and long-term outcomes in for heart failure diagnosis and has similarly challenged the
heart failure patients.19–22 Treatments directed at normal- design of trials of NP-guided treatment. Six trials testing the
ization of serum sodium levels, however, have not been value of an absolute NP target (Table 1) all used a different
associated with improvements in clinical outcomes among threshold NP value, with NT-proBNP targets ranging widely
hospitalized heart failure patients.23 Moreover, even for from 400 to 2200 ng/L. Paradoxically, the trials that have
parameters that show a graded association with risk such demonstrated benefit for NP-guided therapy have not been
as blood pressure, lower may not always be better. For those with the most stringent NP targets, arguing against the
example, in the Action to Control Cardiovascular Risk in notion that more aggressive efforts to reduce NP levels are
Diabetes–Blood Pressure (ACCORD-BP) trial, a strategy necessarily better.
of intensive treatment to aggressive blood pressure targets In the face of these limitations of uniform NP targets,
among diabetic patients was associated with no benefit and some have advocated instead for individualizing NP targets.
a higher rate of adverse events.24 The reference point for this approach is typically set as the
Uncertainty about the incremental value of serial BNP BNP or NT-proBNP nadir at or shortly after hospital dis-
assessment in routine heart failure management has spawned charge, with treatment targeted at maintaining NP levels at
a number of randomized, controlled trials of NP-guided treat- or near this value. Although this approach has the virtue of
ment with a wide range of study designs and treatment tar- acknowledging the inherent between-patient variability in NP
gets25–33 (see Tables 1 and 2). The overall results are mixed, levels, the challenge is the need to define both an appropri-
with the largest studies showing no clear evidence of bene- ate reference baseline and the amount of deviation from this
fit but recent positive trials resurrecting enthusiasm for this baseline that should trigger intervention. Because the long-
approach. Although some have leveraged meta-analytic tech- term within-patient variability in BNP levels exceeds 30%
niques to infer mortality benefit from the biomarker-guided even in stable heart failure patients,45 the amount of change
approach,34 the considerable between-trial heterogeneity in NP levels that is clinically relevant is particularly difficult
makes it difficult to interpret the results of a pooled analy- to discern. In the Can Pro-Brain-Natriuretic Peptide Guided
sis. In the discussion that follows, the evidence supporting the Therapy of Chronic Heart Failure Improve Heart Failure
efficacy of an NP-targeted strategy against the 4 assumptions Morbidity and Mortality? (PRIMA) study,30 the NT-proBNP
outlined above is reviewed. target was based on the lowest plasma level within 2 weeks of
hospital discharge, resulting in a median target value of 2491
Can We Define an Optimal NP Target? pg/mL, well above the absolute threshold used in any of the
The core premise of a biomarker-guided approach is that heart trials using uniform BNP targets. Uptitration of therapy was
failure patients can be efficiently risk stratified for treatment recommended for patients in the biomarker-guided arm when
Downloaded from http://circ.ahajournals.org/ by guest on May 17, 2015Desai NP-Guided Therapy is Not Useful 511
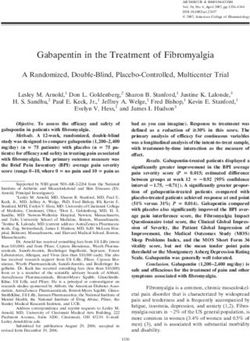
Table 1. Trials of Natriuretic Peptide–Guided Management Using a Fixed Natriuretic Peptide Target
Favors
Mean Target for Comparator Follow-up Primary NP-Guided
n Inclusion Criteria Age, y NP-Guided Arm Group(s) Duration End Point(s) Treatment
Troughton et al 25
69 HF hospitalization, LVEF512 Circulation January 29, 2013
Table 3. Absolute Reductions in Natriuretic Peptide Levels and Percent Achieving Set Targets in Trials of Natriuretic
Peptide–Guided Heart Failure Therapy
Absolute Reduction in NP* Levels, Absolute Reduction in NP* Levels, Achieving Target, NP-Guided Achieving Target,
NP-Guided Group, pg/mL Control Group,† pg/mL Group, % Control Group, %†
Trials with uniform NP Targets
Troughton et al25 668 25 … …
STARS-BNP26 68 (BNP) … 33 …
TIME-CHF 28
… … Minority Minority
BATTLESCARRED29 463 399 49 32
PROTECT31 1219 102 44 36
Berger et al32 … … Majority Majority
Trials with individualized NP targets
STARBRITE27 40 (BNP) −31 (BNP) 68 63
PRIMA30 432 572 80 80
SIGNAL-HF33 301 362 19 22
BATTLESCARRED indicates NT-proBNP-Assisted Treatment to Lessen Serial Cardiac Readmissions and Death; BNP, B-type natriuretic peptide; NP, natriuretic peptides;
PRIMA, Can Pro-Brain-Natriuretic Peptide Guided Therapy of Chronic Heart Failure Improve Heart Failure Morbidity and Mortality?; SIGNAL-HF, Swedish Intervention
Study–Guidelines and NT-ProBNP Analysis in Heart Failure; PROTECT, Use of NT-proBNP Testing to Guide Heart Failure Therapy in the Outpatient Setting; STARBRITE,
Strategies for Tailoring Advanced Heart Failure Regimens in the Outpatient Setting: Brain Natriuretic Peptide Versus the Clinical Congestion Score; STARS-BNP, Systolic
Heart Failure Treatment Supported by BNP; and TIME-CHF, Trial of Intensified vs Standard Medical Therapy in Elderly Patients With Congestive Heart Failure.
*All numbers reflect values of NT-proBNP unless specified otherwise.
†
For trials with 2 control groups, data reflect the intensive clinical management arm.
reach the target. Although many therapies with proven benefit events, 56% of patients in the NP-guided arm and 64% of those
in heart failure patients reduce circulating NP concentrations, in the standard care arm failed to reach the target NT-proBNP
it is not clear that “ideal” NP levels are achievable in every ofDesai NP-Guided Therapy is Not Useful 513
Score (STARBRITE) trial,27 discordance between BNP mea- therapies varies according to heart failure severity or NP lev-
surements and the clinical assessment of congestion was infre- els. In fact, trials of β-blockers,49 renin-angiotensin system
quent, suggesting that NP levels often do not add information antagonists,50 and cardiac resynchronization therapy51 have
to what clinicians already know. shown benefits that are largely independent of baseline NP
In most trials, persistently high NP levels obligated more concentrations. Accordingly, the vast majority of those with
frequent follow-up visits. Superior outcomes with NP-guided chronic heart failure who do not have markedly elevated NP
therapy in selected trials could therefore be attributable in levels43 should still derive benefit from uptitration of proven
large measure to the more intensive clinical support provided therapies. In addition, for the nearly 50% of patients with
to patients with persistently elevated NP levels rather than heart failure and preserved ejection fraction for whom there
success in reducing NP levels to target. In the Systolic Heart is little evidenced-based treatment, it is unclear how elevated
Failure Treatment Supported by BNP (STARS-BNP) trial,26 NP levels should influence clinicians to adapt their approach.
patients in the BNP-guided arm had twice the number of Advocates of the NP-guided approach point out that
physician visits and more frequent medication changes than adherence to published guidelines is suboptimal in clinical
those in the standard care arm, even though only 33% reached practice52 and note that serial NP measurement may be an
the target BNP of 2200 pg/mL were deliberately triaged tion reduces the “guidance” provided by serial NP measure-
to a heart failure specialist for more intensive management, ment to little more than an “intellectual crutch” to practice
and the remainder of patients were managed either by primary evidence-based medicine.53 Moreover, if NP levels truly
care physicians or a nurse-led multidisciplinary team. The facilitate more appropriate medication titration, the greatest
NT-proBNP-Assisted Treatment to Lessen Serial Cardiac opportunity for NP-guided treatment would be expected in
Readmissions and Death (BATTLESCARRED) trial29 the hands of inexperienced clinicians who are less aware of
specifically tested the incremental value of the NP-guided guidelines and for whom the assessment of volume status or
approach relative to both a positive control of intensive, heart failure stability is especially difficult. However, the 1
standardized clinical care that directed medication titration trial examining the benefits of such a strategy in a primary
based on a clinical score and a usual-care arm that received care population (Swedish Intervention Study–Guidelines and
routine primary care follow-up. Relative to usual care, both NT-ProBNP Analysis in Heart Failure [SIGNAL-HF]33) sug-
treatment groups experienced similar reductions in NP gested no significant difference in drug titration or clinical
levels, intensification of medical therapy, and reductions in outcomes between routine care and an NP-guided approach.
the composite of death or heart failure hospitalization. No Ultimately, serial NP measurements are an inadequate sur-
overall difference in survival was seen between the NP-guided rogate for good clinical judgment. Routine titration of neuro-
strategy and intensive clinical follow-up. hormonal antagonists or other heart failure therapies in some
patients with persistently elevated NP levels may be harmful.
Should Patients With Elevated NP Excessive reliance on NP levels to assess volume status might
Levels Be Treated Differently? prompt inappropriate dose escalation of loop diuretics among
Most trials of NP-guided therapy have not defined a specific patients without significant congestion and increase the rate
algorithm to address elevated NP levels but have encouraged of hypotension, renal dysfunction, and other adverse events.
clinicians to respond to elevated NP levels by further titrating Low NP levels may provide false reassurance that treatment
drugs with established benefit in heart failure to recommended is adequate, even as other clinical parameters suggest other-
targets. Acknowledging the association among loop diuretics, wise.43 Aggressive medication titration to manage high NP
neurohormonal activation, and adverse outcomes in heart fail- values may also be poorly tolerated in the elderly or those
ure,47 more recent trials have in addition discouraged titration with significant renal dysfunction (who were systematically
of loop diuretics in patients with high NP levels and have even excluded from most trials). In the TIME-CHF28 trial, which
recommended dose reduction in stable patients. Because high overall showed no incremental benefit to NP-guided therapy,
NP levels frequently direct intensification of therapy even in a strong interaction with age was noted in secondary analyses.
patients who may be clinically asymptomatic, the NP-guided Although patients 75
use of angiotensin-converting enzyme inhibitors, β-blockers, years of age derived no benefit and experienced a higher rate
angiotensin receptor blockers, and spironolactone over stan- of adverse events from NP-guided drug titration. Similar vari-
dard, symptom-guided care. ation in the benefits of NP-guided treatment according to age
Guideline-based recommendations for heart failure man- noted in other trials29 suggests that this is not a spurious result.
agement emphasize titration of neurohormonal antagonists This signal of potential harm among older patients within the
to maximally tolerated doses and minimization of diuretic context of a well-managed clinical trial raises serious con-
dosing in all heart failure patients with reduced ejection frac- cerns for the generalization of the NP-guided approach to
tion.48 There is little evidence that the benefit of heart failure unselected patients in real-life practice, in which an increasing
Downloaded from http://circ.ahajournals.org/ by guest on May 17, 2015514 Circulation January 29, 2013
proportion of heart failure patients are elderly with substantial with normal NP levels and those with advanced age, preserved
comorbid medical illness. Indeed, the most compelling study ejection fraction, and significant medical comorbidities, who
favoring NP-guided treatment to date31 also has the distinction make up the growing majority of the heart failure burden, will
of enrolling a much younger population of patients (median continue to rely on the best clinical judgment of physicians
age, 63 years) than other trials. skilled in the art of medicine.
Conclusion: Serial NP Levels Are Not Disclosures
Useful for Most Heart Failure Patients Dr Desai reports having been a paid consultant to Novartis, Reata,
In an era of increasing concern about both the clinical and Boston Scientific, and Intel.
economic consequences of the growing heart failure burden,
there is an imperative to design new approaches to longitudi- References
nal heart failure management that are both scalable and effec- 1. Tang WH, Francis GS, Morrow DA, Newby LK, Cannon CP, Jesse RL,
tive in improving outcomes. Early recognition of patients with Storrow AB, Christenson RH, Apple FS, Ravkilde J, Wu AH; National
Academy of Clinical Biochemistry Laboratory Medicine. National Acad-
early instability or impending decompensation is a key step to emy of Clinical Biochemistry Laboratory Medicine practice guidelines:
effective intervention but is challenging when based on clini- clinical utilization of cardiac biomarker testing in heart failure. Circula-
cal assessment alone. Given that NPs rise with hemodynamic tion. 2007;116:e99–e109.
stress in a pattern that correlates with risk for short- and long- 2. Masson S, Latini R, Anand IS, Barlera S, Angelici L, Vago T, Tognoni G,
Cohn JN; Val-HeFT Investigators. Prognostic value of changes in N-ter-
term clinical outcomes, it is appealing to look to serial NP minal pro-brain natriuretic peptide in Val-HeFT (Valsartan Heart Failure
measurements to help direct the necessary intensity of heart Trial). J Am Coll Cardiol. 2008;52:997–1003.
failure treatment. 3. Januzzi JL Jr, Sakhuja R, O’donoghue M, Baggish AL, Anwaruddin S,
Chae CU, Cameron R, Krauser DG, Tung R, Camargo CA Jr, Lloyd-Jones
Exactly how clinicians should leverage NP levels to DM. Utility of amino-terminal pro-brain natriuretic peptide testing for
improve heart failure outcomes, however, remains unclear. prediction of 1-year mortality in patients with dyspnea treated in the emer-
Although some trials have suggested benefits for a strategy gency department. Arch Intern Med. 2006;166:315–320.
focused on reducing NP levels below a fixed target level, no 2 4. Cleland JG, McMurray JJ, Kjekshus J, Cornel JH, Dunselman P, Fonseca
C, Hjalmarson A, Korewicki J, Lindberg M, Ranjith N, van Veldhuisen DJ,
trials have tested the same target, and trials with similar targets Waagstein F, Wedel H, Wikstrand J; CORONA Study Group. Plasma con-
have returned discrepant results. The substantial between- centration of amino-terminal pro-brain natriuretic peptide in chronic heart
patient variability in NP levels makes individualized NP failure: prediction of cardiovascular events and interaction with the effects
of rosuvastatin: a report from CORONA (Controlled Rosuvastatin Multi-
targets more appealing than fixed targets, but none of the trials
national Trial in Heart Failure). J Am Coll Cardiol. 2009;54:1850–1859.
of this approach has shown significant impacts on morbidity 5. Masson S, Latini R, Anand IS, Vago T, Angelici L, Barlera S, Missov ED,
or mortality. Even if appropriate targets can be established, Clerico A, Tognoni G, Cohn JN; Val-HeFT Investigators. Direct compari-
values that are set too low are generally unachievable and son of B-type natriuretic peptide (BNP) and amino-terminal proBNP in a
large population of patients with chronic and symptomatic heart failure: the
those that are set too high likely do not materially alter clinical Valsartan Heart Failure (Val-HeFT) data. Clin Chem. 2006;52:1528–1538.
management. Furthermore, the core assumption of NP-guided 6. Doust JA, Pietrzak E, Dobson A, Glasziou P. How well does B-type na-
therapy, the notion that heart failure therapy should vary on triuretic peptide predict death and cardiac events in patients with heart
the basis of measured NP levels (or indeed any other risk failure: systematic review. BMJ. 2005;330:625.
7. Anand IS, Fisher LD, Chiang YT, Latini R, Masson S, Maggioni AP,
marker), is not well supported by clinical evidence. Guidelines Glazer RD, Tognoni G, Cohn JN; Val-HeFT Investigators. Changes in
recommend titration of evidence-based therapies to maximally brain natriuretic peptide and norepinephrine over time and mortality and
tolerated doses in all patients regardless of background risk. If morbidity in the Valsartan Heart Failure Trial (Val-HeFT). Circulation.
2003;107:1278–1283.
the problem is lack of adherence to these guidelines, strategies 8. Bettencourt P, Azevedo A, Pimenta J, Friões F, Ferreira S, Ferreira A. N-
should focus on educating clinicians about the clinical terminal-pro-brain natriuretic peptide predicts outcome after hospital dis-
assessment and optimal management of heart failure patients charge in heart failure patients. Circulation. 2004;110:2168–2174.
rather than on the use of serial laboratory testing that does not 9. Latini R, Masson S, Wong M, Barlera S, Carretta E, Staszewsky L, Vago
T, Maggioni AP, Anand IS, Tan LB, Tognoni G, Cohn JN; Val-HeFT In-
clearly influence the selection of appropriate treatment. Sadly, vestigators. Incremental prognostic value of changes in B-type natriuretic
there are no shortcuts. peptide in heart failure. Am J Med. 2006;119:70.e23–70.e30.
This is not to say that NP levels have no place in heart 10. Logeart D, Thabut G, Jourdain P, Chavelas C, Beyne P, Beauvais F, Bouvi-
er E, Solal AC. Predischarge B-type natriuretic peptide assay for identify-
failure management. Risk stratification by NP levels may be
ing patients at high risk of re-admission after decompensated heart failure.
important to identify a subset of patients who benefit from J Am Coll Cardiol. 2004;43:635–641.
more intensive subspecialty care, as highlighted in the study 11. O’Connor CM, Hasselblad V, Mehta RH, Tasissa G, Califf RM, Fiuzat M,
by Berger et al.32 Additionally, the age interaction suggested Rogers JG, Leier CV, Stevenson LW. Triage after hospitalization with ad-
vanced heart failure: the ESCAPE (Evaluation Study of Congestive Heart
in TIME-HF and BATTLESCARRED and the positive results Failure and Pulmonary Artery Catheterization Effectiveness) risk model
of the PROTECT trial reserve the possibility that there may and discharge score. J Am Coll Cardiol. 2010;55:872–878.
be a role for NP-targeted treatment in younger patients with 12. Fruhwald FM, Fahrleitner-Pammer A, Berger R, Leyva F, Freemantle N,
reduced ejection fraction, particularly those being treated by Erdmann E, Gras D, Kappenberger L, Tavazzi L, Daubert JC, Cleland JG.
Early and sustained effects of cardiac resynchronization therapy on N-
clinicians who require the objective prompt to titrate treat- terminal pro-B-type natriuretic peptide in patients with moderate to severe
ment that a laboratory measure provides. However, patients heart failure and cardiac dyssynchrony. Eur Heart J. 2007;28:1592–1597.
Downloaded from http://circ.ahajournals.org/ by guest on May 17, 2015Desai NP-Guided Therapy is Not Useful 515
13. Lee SC, Stevens TL, Sandberg SM, Heublein DM, Nelson SM, Jougasaki 28. Pfisterer M, Buser P, Rickli H, Gutmann M, Erne P, Rickenbacher P, Vuil-
M, Redfield MM, Burnett JC Jr. The potential of brain natriuretic peptide lomenet A, Jeker U, Dubach P, Beer H, Yoon SI, Suter T, Osterhues HH,
as a biomarker for New York Heart Association class during the outpatient Schieber MM, Hilti P, Schindler R, Brunner-La Rocca HP; TIME-CHF
treatment of heart failure. J Card Fail. 2002;8:149–154. Investigators. BNP-guided vs symptom-guided heart failure therapy:
14. Motwani JG, McAlpine H, Kennedy N, Struthers AD. Plasma brain natri- the Trial of Intensified vs Standard Medical Therapy in Elderly Patients
uretic peptide as an indicator for angiotensin-converting-enzyme inhibi- With Congestive Heart Failure (TIME-CHF) randomized trial. JAMA.
tion after myocardial infarction. Lancet. 1993;341:1109–1113. 2009;301:383–392.
15. Latini R, Masson S, Anand I, Judd D, Maggioni AP, Chiang YT, Bevilac- 29. Lainchbury JG, Troughton RW, Strangman KM, Frampton CM, Pilbrow
qua M, Salio M, Cardano P, Dunselman PH, Holwerda NJ, Tognoni G, A, Yandle TG, Hamid AK, Nicholls MG, Richards AM. N-terminal pro-
Cohn JN; Valsartan Heart Failure Trial Investigators. Effects of valsartan B-type natriuretic peptide-guided treatment for chronic heart failure: re-
on circulating brain natriuretic peptide and norepinephrine in symptomatic sults from the BATTLESCARRED (NT-proBNP-Assisted Treatment to
chronic heart failure: the Valsartan Heart Failure Trial (Val-HeFT). Circu- Lessen Serial Cardiac Readmissions and Death) trial. J Am Coll Cardiol.
lation. 2002;106:2454–2458. 2009;55:53–60.
16. Tsutamoto T, Wada A, Maeda K, Mabuchi N, Hayashi M, Tsutsui T, Oh- 30. Eurlings LW, van Pol PE, Kok WE, van Wijk S, Lodewijks-van der Bolt C,
nishi M, Sawaki M, Fujii M, Matsumoto T, Matsui T, Kinoshita M. Effect Balk AH, Lok DJ, Crijns HJ, van Kraaij DJ, de Jonge N, Meeder JG, Prins
of spironolactone on plasma brain natriuretic peptide and left ventricular M, Pinto YM. Management of chronic heart failure guided by individual
remodeling in patients with congestive heart failure. J Am Coll Cardiol. N-terminal pro-B-type natriuretic peptide targets: results of the PRIMA
2001;37:1228–1233. (Can PRo-brain-natriuretic peptide guided therapy of chronic heart failure
17. Stanek B, Frey B, Hülsmann M, Berger R, Sturm B, Strametz-Juranek IMprove heart fAilure morbidity and mortality?) study. J Am Coll Cardiol.
J, Bergler-Klein J, Moser P, Bojic A, Hartter E, Pacher R. Prognostic 2010;56:2090–2100.
evaluation of neurohumoral plasma levels before and during beta-block- 31. Januzzi JL Jr, Rehman SU, Mohammed AA, Bhardwaj A, Barajas L, Bara-
er therapy in advanced left ventricular dysfunction. J Am Coll Cardiol. jas J, Kim HN, Baggish AL, Weiner RB, Chen-Tournoux A, Marshall JE,
2001;38:436–442. Moore SA, Carlson WD, Lewis GD, Shin J, Sullivan D, Parks K, Wang
18. Cleland JG, Daubert JC, Erdmann E, Freemantle N, Gras D, Kappenberg- TJ, Gregory SA, Uthamalingam S, Semigran MJ. Use of amino-terminal
er L, Tavazzi L; Cardiac Resynchronization-Heart Failure (CARE-HF) pro-B-type natriuretic peptide to guide outpatient therapy of patients
Study Investigators. The effect of cardiac resynchronization on morbidity with chronic left ventricular systolic dysfunction. J Am Coll Cardiol.
and mortality in heart failure. N Engl J Med. 2005;352:1539–1549. 2011;58:1881–1889.
19. Gheorghiade M, Abraham WT, Albert NM, Gattis Stough W, Greenberg 32. Berger R, Moertl D, Peter S, Ahmadi R, Huelsmann M, Yamuti S, Wagner
BH, O’Connor CM, She L, Yancy CW, Young J, Fonarow GC; OPTIMIZE- B, Pacher R. N-terminal pro-B-type natriuretic peptide-guided, intensive
HF Investigators and Coordinators. Relationship between admission se- patient management in addition to multidisciplinary care in chronic heart
rum sodium concentration and clinical outcomes in patients hospitalized failure a 3-arm, prospective, randomized pilot study. J Am Coll Cardiol.
for heart failure: an analysis from the OPTIMIZE-HF registry. Eur Heart 2010;55:645–653.
J. 2007;28:980–988. 33. Persson H, Erntell H, Eriksson B, Johansson G, Swedberg K, Dahlstrom
20. Klein L, O’Connor CM, Leimberger JD, Gattis-Stough W, Piña IL, U. Improved pharmacological therapy of chronic heart failure in pri-
Felker GM, Adams KF Jr, Califf RM, Gheorghiade M; OPTIME-CHF mary care: a randomized Study of NT-proBNP Guided Management
Investigators. Lower serum sodium is associated with increased short- of Heart Failure–SIGNAL-HF (Swedish Intervention study–Guide-
term mortality in hospitalized patients with worsening heart failure: lines and NT-proBNP AnaLysis in Heart Failure). Eur J Heart Fail.
results from the Outcomes of a Prospective Trial of Intravenous Milrinone 2011;12:1300–1308.
for Exacerbations of Chronic Heart Failure (OPTIME-CHF) study. 34. Felker GM, Hasselblad V, Hernandez AF, O’Connor CM. Biomarker-
Circulation. 2005;111:2454–2460. guided therapy in chronic heart failure: a meta-analysis of randomized
21. Leier CV, Dei Cas L, Metra M. Clinical relevance and management of the controlled trials. Am Heart J. 2009;158:422–430.
major electrolyte abnormalities in congestive heart failure: hyponatremia, 35. Redfield MM, Rodeheffer RJ, Jacobsen SJ, Mahoney DW, Bailey KR,
hypokalemia, and hypomagnesemia. Am Heart J. 1994;128:564–574. Burnett JC Jr. Plasma brain natriuretic peptide concentration: impact of
22. Lee WH, Packer M. Prognostic importance of serum sodium concentra- age and gender. J Am Coll Cardiol. 2002;40:976–982.
tion and its modification by converting-enzyme inhibition in patients with 36. Wang TJ, Larson MG, Levy D, Leip EP, Benjamin EJ, Wilson PW, Suther-
severe chronic heart failure. Circulation. 1986;73:257–267. land P, Omland T, Vasan RS. Impact of age and sex on plasma natriuretic
23. Konstam MA, Gheorghiade M, Burnett JC Jr, Grinfeld L, Maggioni AP, peptide levels in healthy adults. Am J Cardiol. 2002;90:254–258.
Swedberg K, Udelson JE, Zannad F, Cook T, Ouyang J, Zimmer C, Or- 37. Wang TJ, Larson MG, Levy D, Benjamin EJ, Leip EP, Wilson PW, Vasan
landi C; Efficacy of Vasopressin Antagonism in Heart Failure Outcome RS. Impact of obesity on plasma natriuretic peptide levels. Circulation.
Study With Tolvaptan (EVEREST) Investigators. Effects of oral tolvaptan 2004;109:594–600.
in patients hospitalized for worsening heart failure: the EVEREST Out- 38. Newton-Cheh C, Larson MG, Vasan RS, Levy D, Bloch KD, Surti A, Gui-
come Trial. JAMA. 2007;297:1319–1331. ducci C, Kathiresan S, Benjamin EJ, Struck J, Morgenthaler NG, Berg-
24. Cushman WC, Evans GW, Byington RP, Goff DC, Jr., Grimm RH, Jr., mann A, Blankenberg S, Kee F, Nilsson P, Yin X, Peltonen L, Vartiainen
Cutler JA, Simons-Morton DG, Basile JN, Corson MA, Probstfield JL, E, Salomaa V, Hirschhorn JN, Melander O, Wang TJ. Association of com-
Katz L, Peterson KA, Friedewald WT, Buse JB, Bigger JT, Gerstein HC, mon variants in NPPA and NPPB with circulating natriuretic peptides and
Ismail-Beigi F. Effects of intensive blood-pressure control in type 2 diabe- blood pressure. Nat Genet. 2009;41:348–353.
tes mellitus. N Engl J Med. 2010;362:1575–1585. 39. Takeishi Y, Toriyama S, Takabatake N, Shibata Y, Konta T, Emi M, Kato T,
25. Troughton RW, Frampton CM, Yandle TG, Espiner EA, Nicholls MG, Kawata S, Kubota I. Linkage disequilibrium analyses of natriuretic pep-
Richards AM. Treatment of heart failure guided by plasma amino- tide precursor B locus reveal risk haplotype conferring high plasma BNP
terminal brain natriuretic peptide (N-BNP) concentrations. Lancet. levels. Biochem Biophys Res Commun. 2007;362:480–484.
2000;355:1126–1130. 40. Ellis KL, Newton-Cheh C, Wang TJ, Frampton CM, Doughty RN,
26. Jourdain P, Jondeau G, Funck F, Gueffet P, Le Helloco A, Donal E, Au- Whalley GA, Ellis CJ, Skelton L, Davis N, Yandle TG, Troughton RW,
petit JF, Aumont MC, Galinier M, Eicher JC, Cohen-Solal A, Juillière Richards AM, Cameron VA. Association of genetic variation in the natri-
Y. Plasma brain natriuretic peptide-guided therapy to improve outcome uretic peptide system with cardiovascular outcomes. J Mol Cell Cardiol.
in heart failure: the STARS-BNP Multicenter Study. J Am Coll Cardiol. 2011;50:695–701.
2007;49:1733–1739. 41. Anwaruddin S, Lloyd-Jones DM, Baggish A, Chen A, Krauser D, Tung R,
27. Shah MR, Califf RM, Nohria A, Bhapkar M, Bowers M, Mancini DM, Chae C, Januzzi JL Jr. Renal function, congestive heart failure, and ami-
Fiuzat M, Stevenson LW, O’Connor CM. The STARBRITE trial: a ran- no-terminal pro-brain natriuretic peptide measurement: results from the
domized, pilot study of B-type natriuretic peptide-guided therapy in pa- ProBNP Investigation of Dyspnea in the Emergency Department (PRIDE)
tients with advanced heart failure. J Card Fail. 2011;17:613–621. Study. J Am Coll Cardiol. 2006;47:91–97.
Downloaded from http://circ.ahajournals.org/ by guest on May 17, 2015516 Circulation January 29, 2013
42. O’Donoghue M, Chen A, Baggish AL, Anwaruddin S, Krauser DG, Tung of heart failure in adults: a report of the American College of Cardiology
R, Januzzi JL. The effects of ejection fraction on N-terminal ProBNP and Foundation/American Heart Association Task Force on Practice Guide-
BNP levels in patients with acute CHF: analysis from the ProBNP Inves- lines: developed in collaboration with the International Society for Heart
tigation of Dyspnea in the Emergency Department (PRIDE) study. J Card and Lung Transplantation. Circulation. 2009;119:e391–e479.
Fail. 2005;11(suppl):S9–S14. 49. Hartmann F, Packer M, Coats AJ, Fowler MB, Krum H, Mohacsi P, Rou-
43. Tang WH, Girod JP, Lee MJ, Starling RC, Young JB, Van Lente F, Fran- leau JL, Tendera M, Castaigne A, Anker SD, Amann-Zalan I, Hoersch S,
cis GS. Plasma B-type natriuretic peptide levels in ambulatory patients Katus HA. Prognostic impact of plasma N-terminal pro-brain natriuret-
with established chronic symptomatic systolic heart failure. Circulation. ic peptide in severe chronic congestive heart failure: a substudy of the
2003;108:2964–2966. Carvedilol Prospective Randomized Cumulative Survival (COPERNI-
44. Dokainish H, Zoghbi WA, Lakkis NM, Al-Bakshy F, Dhir M, Quinones CUS) trial. Circulation. 2004;110:1780–1786.
MA, Nagueh SF. Optimal noninvasive assessment of left ventricular filling 50. Latini R, Masson S, Anand I, Salio M, Hester A, Judd D, Barlera
pressures: a comparison of tissue Doppler echocardiography and B-type S, Maggioni AP, Tognoni G, Cohn JN; Val-HeFT Investigators. The
natriuretic peptide in patients with pulmonary artery catheters. Circula- comparative prognostic value of plasma neurohormones at baseline
tion. 2004;109:2432–2439. in patients with heart failure enrolled in Val-HeFT. Eur Heart J.
45. Schou M, Gustafsson F, Kjaer A, Hildebrandt PR. Long-term clinical 2004;25:292–299.
variation of NT-proBNP in stable chronic heart failure patients. Eur Heart 51. Cleland J, Freemantle N, Ghio S, Fruhwald F, Shankar A, Marijanowski
J. 2007;28:177–182. M, Verboven Y, Tavazzi L. Predicting the long-term effects of cardiac
46. Troughton RW, Frampton CM, Nicholls MG. Biomarker-guided treatment resynchronization therapy on mortality from baseline variables and the
of heart failure: still waiting for a definitive answer. J Am Coll Cardiol. early response a report from the CARE-HF (Cardiac Resynchronization in
2010;56:2101–2104. Heart Failure) Trial. J Am Coll Cardiol. 2008;52:438–445.
47. Felker GM, O’Connor CM, Braunwald E; Heart Failure Clinical Research 52. Fonarow GC, Yancy CW, Albert NM, Curtis AB, Stough WG, Gheorghi-
Network Investigators. Loop diuretics in acute decompensated heart fail- ade M, Heywood JT, McBride ML, Mehra MR, O’Connor CM, Reynolds
ure: necessary? Evil? A necessary evil? Circ Heart Fail. 2009;2:56–62. D, Walsh MN. Heart failure care in the outpatient cardiology practice set-
48. Hunt SA, Abraham WT, Chin MH, Feldman AM, Francis GS, Ganiats ting: findings from IMPROVE HF. Circ Heart Fail. 2008;1:98–106.
TG, Jessup M, Konstam MA, Mancini DM, Michl K, Oates JA, Rahko PS, 53. Packer M. Should B-type natriuretic peptide be measured routinely to
Silver MA, Stevenson LW, Yancy CW. 2009 focused update incorporated guide the diagnosis and management of chronic heart failure? Circulation.
into the ACC/AHA 2005 guidelines for the diagnosis and management 2003;108:2950–2953.
Response to Desai
James L. Januzzi, Jr, MD; Richard Troughton, MD, PhD
We appreciate the elegant comments of Dr Desai; unfortunately, he did not make a strong case against biomarker-guided
therapy (BGT) and was factually incorrect on several important points, only the most important of which we highlight
because of space constraints. Raising concern about potential harm from BGT is a tired and incorrect argument, as is sug-
gesting the risk of undertreatment in those with low natriuretic peptide (NP) values. Not 1 trial has demonstrated safety con-
cerns of BGT, and no trial withheld treatment for those with low NPs: in fact, achieved doses of therapies in BGT studies are
more often equivalent to those in landmark trials. Is this not important? The assertion that benefit from BGT has not come
from stringent NP targets is totally incorrect. In addition, the argument that the inability to always achieve NP targets limits
the value of the approach is flawed: Outcomes are significantly associated with the lowest achieved NP value; some lowering
is better than none; and higher-risk patients may thus be better identified to correctly receive precious resources in this cost-
conscious healthcare environment. The laughable argument of using an immovable/irrelevant parameter such as height to
guide HF therapy ignores the prognostic value of NPs and the value of their lowering. These are only a few of the incorrect
statements made in Dr Desai’s commentary. However, there is a common reassuring theme in both of our arguments: Best
care is needed for our patients with HF. Routinely combining biomarkers with clinical judgment helps achieve this goal.
Downloaded from http://circ.ahajournals.org/ by guest on May 17, 2015Are Serial BNP Measurements Useful in Heart Failure Management?: Serial Natriuretic
Peptide Measurements Are Not Useful in Heart Failure Management: The Art of Medicine
Remains Long
Akshay S. Desai
Circulation. 2013;127:509-516
doi: 10.1161/CIRCULATIONAHA.112.120493
Circulation is published by the American Heart Association, 7272 Greenville Avenue, Dallas, TX 75231
Copyright © 2013 American Heart Association, Inc. All rights reserved.
Print ISSN: 0009-7322. Online ISSN: 1524-4539
The online version of this article, along with updated information and services, is located on the
World Wide Web at:
http://circ.ahajournals.org/content/127/4/509
Permissions: Requests for permissions to reproduce figures, tables, or portions of articles originally published
in Circulation can be obtained via RightsLink, a service of the Copyright Clearance Center, not the Editorial
Office. Once the online version of the published article for which permission is being requested is located,
click Request Permissions in the middle column of the Web page under Services. Further information about
this process is available in the Permissions and Rights Question and Answer document.
Reprints: Information about reprints can be found online at:
http://www.lww.com/reprints
Subscriptions: Information about subscribing to Circulation is online at:
http://circ.ahajournals.org//subscriptions/
Downloaded from http://circ.ahajournals.org/ by guest on May 17, 2015You can also read