Sports Medicine FOR THE PRIMARY CARE PROVIDER - Hershey Medical Center
←
→
Page content transcription
If your browser does not render page correctly, please read the page content below
WINTER 2016
Sports Medicine F O R T H E P R I M A R Y C A R E P R O V I D E R
Concussions and Chronic Traumatic
Encephalopathy
BY MATTHEW SILVIS, M.D.
The recent movie “Concussion” has created quite a stir nationally about chronic traumatic
encephalopathy (CTE). This is written to help fellow providers understand what is known, and
just as importantly, unknown about this condition.
In 10 to 15 percent of athletes with concussion, symptoms last longer than 10 days and can
persist for weeks, months, or years after injury. Post-concussion syndrome is ill-defined, poorly
understood and currently explained as persistent symptoms or signs of concussion that persist
for weeks or months after concussion. ‘Time’ is the primary treatment for post-concussion Dear Health Care Provider,
syndrome, which is frequently frustrating for patients and providers, alike. A multidisciplinary My name is Matthew Silvis. I am medical
approach is recommended, including providers with experience in caring director of Penn State Primary Care Sports
for sports-related concussions and may also include pharmacologic Medicine. I have enclosed the winter edition
management, physical, vestibular, speech and occupational of our Primary Care Sports Medicine
therapies, neuropsychological evaluation and treatment, visio-ocular Newsletter, a biannual newsletter of seasonal
evaluation and treatment, and behavioral health, amongst others. sports topics. We hope you find the information
In recent years, there has been increasing media attention to useful and appreciate any feedback you have
sports-related concussion, specifically CTE. CTE is a progressive to enhance our efforts. We have selected a
neurodegenerative tauopathy associated with repetitive brain variety of topics for this issue.
injury. It was originally diagnosed in boxers
If you’d like to receive this newsletter by
more than 85 years ago. Research groups
email, please forward your address to my
have proposed that head injury, including
administrative assistant, Sandy Miland at
both concussive and subconcussive blows,
smiland@hmc.psu.edu. Please send any
leads to neuropathologic changes and
future topic ideas to Sandy or me at
the development of alterations in mood,
cognition and behavioral functioning. msilvis@hmc.psu.edu.
CTE can occur in as few as one blow to the
head and appears to develop from eight to Enjoy,
20 years following retirement from contact
sports. The diagnosis is made at autopsy and
is separate from permanent post-concussion Matthew Silvis, M.D.
syndrome. Initially, mood and behavior ASSOCIATE PROFESSOR
changes predominate with later clinical PENN STATE HERSHEY FAMILY AND COMMUNITY MEDICINE
presentations involving cognitive and PENN STATE HERSHEY ORTHOPAEDICS AND REHABILITATION
PENN STATE MILTON S. HERSHEY MEDICAL CENTER
CONT’D ON PAGE 2Skin Infections in Wrestlers
BY BY JESSICA BUTTS, M.D.
Wrestling season is upon us. Due to the nature of the sport, with brief, here is a listing with a few reminders:
near constant skin-to-skin contact, skin infections are a common
• Tinea corporis requires a minimum of 72 hours of topical antifungal;
issue encountered when caring for competitive wrestlers of all ages.
Fungal infections (e.g., ringworm), viral infections (typically herpes • Tinea capitis requires 10 days of oral antifungals;
gladiatorum caused by HSV-I) and bacterial infections (impetigo • Herpes gladiatorum requires treatment with an oral antiviral: 10 days
and MRSA) are all common offenders. As these infections are highly for initial outbreak and 120 hours for recurrence; all lesions must be
transmissible among these athletes, providers need to be vigilant with crusted over with no new lesions in the preceding 48 hours.
patients who wrestle and present with skin complaints. Many skin
infections, specifically those listed above, would disqualify the athlete • Bacterial skin infections need at least three days of oral antibiotics
until they have been properly treated. As these infections directly affect with all lesions scabbed.
their eligibility to participate, wrestlers may go to extreme measures All of this information, and more, can be found at the bottom of the
to hide the nature of their lesions. Applying bleach, using sandpaper PIAA wrestling skin form.
and excoriating (or picking) are all possible ways to hide or disguise
As we care for these athletes, being aware of how common these
disqualifying skin conditions. Therefore, providers who treat these
skin infections are in this population, as well as being aware of the
athletes need to have a very high level of suspicion for these conditions,
potentially atypical appearance of some of these lesions, is important.
as well as a low threshold to treat empirically if any of these conditions
Being familiar with the PIAA
are suspected.
guidelines for return-to-play
Completion of the PIAA “skin form” is universally required for all and having a low threshold to
wrestlers with any potentially contagious skin lesion to be allowed to treat keeps as many athletes in
participate. This form is infinitely useful to keep in any primary care the game (or in this case on
office setting where a “wrestler with rash” may present for evaluation. the mat) as possible.
This form identifies diagnosis, number and location of lesions, and
type and date of treatment initiated. This form is required at pre-
participation skin checks by any athlete who has had a skin evaluation
and treatment. Completion of this form by the provider at the time of
visit streamlines this process for the athlete, athletic trainer and medical
staff covering these events.
The PIAA form also outlines standard required treatment for common
skin infections to be eligible to return to play. These guidelines are
extraordinarily useful as they outline the minimum required treatment
for some of the most commonly encountered skin conditions. No
athletes with new lesions in the preceding 48 hours, or with lesions
that are oozing, draining or moist, will be permitted to participate. In
CONCUSSION FROM COVER
motor impairment. by other groups of neuropathologists. recent study demonstrated no increased
Interestingly, there is a greater incidence risk of neurodegenerative disease in a
However, CTE is poorly understood
of abnormal tau protein deposition in long-term follow-up study of high school
at this time. Athletes with significant
the brains of opiate abusers compared to football players versus a control group
neurologic symptoms do not always have
controls according to research studies. Of (band members). While providers and the
histopathologic changes of CTE, and
note, more than half of the players in the public are appropriately concerned, much
the presence of histopathologic changes
National Football League (NFL) have been is unknown about CTE and a definitive
of CTE is not always associated with
reported to use opiates during their NFL causal link to American football has yet
neurologic symptoms. Tau protein may be
careers with most reporting abuse, clouding to be determined. Future prospective,
found in individuals undergoing normal
the etiology of CTE. NFL players are less longitudinal, population-based studies
aging, independent of head trauma,
likely to die from suicide than the general are needed to better understand CTE. For
although some leading researchers report
population and there is no definitive link now, following standard-of-care in the
a qualitatively different deposition of
between CTE and suicide at this time. In management of athletes with concussion
abnormal tau protein in CTE versus other
fact, retired NFL players live longer than remains the best approach.
neurodegenerative diseases. However,
their age-matched peers. Additionally, one
this finding has not been cross-validated
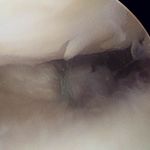
2When is a meniscal tear not a meniscal tear?
When it is a root avulsion!
BY ROBERT A. GALLO, MD
Meniscus tears come in all shapes and sizes. There are vertical tears,
horizontal tears, radial, and even complex tears which can include any
combination of these tear orientations. These conditions are managed
largely by the degree of symptomatology, tear orientation and location.
More recently, meniscal root avulsions (tears), a subset of meniscal
tears, have received increased attention in the orthopaedic community.
A meniscal root avulsion involves any disruption of the tibial
attachment sites of the menisci. While each meniscus has attachments
circumferentially to the knee capsule, the root insertions are located at
1 2
both the anterior and posterior ends of each meniscus. The meniscal
root attachments anchor each meniscus to the tibia and are essential
to the normal function of the meniscus as “shock absorbers.” With
a detachment of its root attachment, the meniscus loses the ability
to resist hoop stresses vital to its normal function. Therefore, the
downward force of the femoral condyles on the tibia causes the
meniscus to eventually extrude beyond the confines of the tibio-
femoral articulation (figure 1). Rapidly progressive osteoarthritis can
follow if the meniscus is unable to efficiently transmit load to the tibia.
While a meniscal root avulsion can occur in younger individuals
in a trauma setting, the majority occur in middle-aged adults. Most 3A 3B
patients recall incidents when they felt a “pop” and immediate
FIGURE 1: Extrusion of the meniscus beyond the border of the femoro-tibial
pain in the posterior medial or lateral aspect of the knee. Similar to articulation (line) occurs with prolonged weight-bearing following disruption of the
other meniscal tears, patients describe worsening pain with deep root attachment.
knee flexion; however, the pain is more posterior than meniscal FIGURE 2: Meniscal root tears are readily visualized as increased signal between the
tears involving the body and posterior horn of the meniscus. On meniscus and tibial (arrow) on T2-coronal MRI sequences.
examination, the hallmark physical examination finding is tenderness FIGURE 3: Meniscus root tears can be surgically repaired by passing sutures into the
to palpation of the joint line at the posterior aspect of the knee. meniscus, sending the sutures down a tunnel through the tibia, and tying the sutures
over a button on the anterior tibial cortex.
Imaging should begin with anteroposterior weightbearing, lateral
and Merchant radiographic views of the affected knee. If moderate
or severe osteoarthritis is identified on radiographs, treatment The post-operative limitations are fairly extensive and involve a period
should manage the symptoms of osteoarthritis. In cases of relatively of non-weight-bearing and immobilization.
preserved joint spaces, MRI should be considered if a posterior root Despite the theoretical advantages of surgical repair, long-term clinical
tear is suspected. While they can usually be visualized on any image data assessing healing, meniscal extrusion and the ability to slow the
orientation, meniscal root avulsions are most readily seen on coronal progression of arthritis are lacking. Therefore, repair should only be
images as an area of signal intensity between the posterior meniscus considered after careful evaluation, which includes assessment of the
and tibia (figure 2). amount of pre-existing osteoarthritis, level of disability and symptoms
The treatment for meniscal root avulsions has evolved over recent and body habitus (i.e., obese patients place increased stress on any
years. Because of recent biomechanical studies confirming the benefits repair and are more likely to fail the repair procedure). Intra-articular
of restoring the meniscal root attachment, repair of these avulsion-type steroid injections and physical therapy are useful alternative treatment
tears has become increasingly popular. Surgical repair involves the modalities.
following process: In conclusion, root avulsions are a unique category of meniscal tears
• passing a high-strength suture through the torn edge of the that must be considered a different entity than other meniscal tears.
meniscus; Presenting with posterior knee pain, meniscal root tears can render
the meniscus nonfunctional, resulting in increased joint reactive forces
• passing those sutures through a small tunnel beginning at the and leading to rapidly progressive osteoarthritis. Consultation to an
normal root insertion site and exiting along the anteromedial tibia orthopaedic surgeon should be considered in those with an MRI-
adjacent to the tibial tubercle; then diagnosed meniscal root tear and relatively well-preserved joint space,
• tying the sutures over a button on the anteromedial cortex of the as seen on anteroposterior weight-bearing radiographs.
tibia (figure 3).
3Helmets – A False Sense of Security?
BY JAYSON LOEFFERT, D.O. , PRIMARY CARE SPORTS MEDICINE FELLOW
However, there are types of head injuries that helmets have been
shown to prevent, including skull fractures and head lacerations.
Helmets can compress during impact, allowing some deceleration
and decreasing the direct force applied to the head. Unfortunately,
this does not translate to prevention of all types of head injuries,
namely traumatic brain injury and concussion.
The question then is why haven’t helmets had more of an impact
on preventing head injury? There are several hypotheses: First, it
has been widely demonstrated that helmet use does not eliminate
the risk of concussion. While helmets can absorb some impact
during a collision, they do not significantly reduce the acceleration
or deceleration and rotational forces resulting in concussion.
Additionally, helmets are not being tested at speeds consistent with
all usage environments. The average skier travels at a speed of 24.6 to
The colder weather brings with it the anticipation of snow, and, of 31.3 miles per hour, yet linear impact tests are conducted in the lab at
course, skiing and snowboarding! Over the last decade, the concern only 14.3 miles per hour. Going above the average speed could result
for injury and prevention has grown, and simultaneously, public in as much as a quadruple increase in subjected impact energy above
helmet use has skyrocketed: 6 to 25 percent in 2003 to 70 to 90 what the helmet is designed to protect. Therefore, helmets may not
percent in 2013. The purpose of this article is to educate fellow be designed to handle the forces they are subjected to in real-world
providers on the limitations of helmet use for preventing head injury, environments. Finally, the idea of increased risk-taking behavior due
as well as to warn against false security and over-assumption that to helmet use has been discussed. While the idea that helmets overtly
helmets prevent head injury. cause recklessness has been refuted, their use could have an indirect
Groups all over the world have recognized the growing trend to wear effect. If athletes believe they are more protected because they are
helmets while skiing or snowboarding, and have studied the effect this wearing a helmet, they may travel at faster speeds or engage in riskier
has had on head injury. Although studies are limited, there does not maneuvers than they otherwise would without the helmet.
appear to be a strong correlation between helmet use and decreased Fortunately head injuries in snow sports are rare, but still a concern
head injury. In fact, one study has shown that in spite of increased for all skiers and snowboarders. When considering helmet use during
helmet use, the frequency of head injuries also increased over the snow sports, it is important to realize that helmets will not prevent all
same time period. head injuries. Practicing safe activities and wiser decision-making on
the mountain may be a better way to prevent head injury!
PRIMARY CARE SPORTS MEDICINE Shawn Phillips, M.D. Robert Gallo, M.D.
sphillips6@hmc.psu.edu rgallo@hmc.psu.edu
Matthew Silvis, M.D.
Assistant Professor, Departments of Family and Community Assistant Professor, Penn State Hershey Orthopaedics
msilvis@hmc.psu.edu
Medicine and Orthopaedics Penn State Hershey Bone and Joint Institute, 717-531-5638
Associate Professor, Departments of Family and Community
Penn State Hershey Medical Group—Mt. Joy, 717-653-2900
Medicine and Orthopaedics Scott Lynch, M.D.
Penn State Hershey Bone and Joint Institute, 717-531-5638
Medical Director, Primary Care Sports Medicine slynch@hmc.psu.edu
Penn State Hershey Medical Group—Palmyra, 717-838-6305 Rory Tucker, M.D. Associate Professor, Director of Sports Medicine Service
Penn State Hershey Bone and Joint Institute, 717-531-5638 jtucker@hmc.psu.edu Practice Site Clinical Director of Adult Bone and Joint Institute
Assistant Professor, Departments of Family and Community Medicine Associate Director of Orthopaedic Residency Education, 717-531-5638
Jessica Butts, M.D.
and Orthopaedics Penn State Hershey Bone and Joint Institute, 717-531-5638
Jbutts@hmc.psu.edu
Penn State Hershey Medical Group—Camp Hill, 717-691-1212
Assistant Professor, Departments of Family and Community Medicine
Penn State Hershey Bone and Joint Institute, 717-531-5638 SPORTS MEDICINE PHYSICAL THERAPY
and Orthopaedics
Penn State Hershey Medical Group—Nyes Road, 717-214-6545 Andrew Wren, D.O. Robert Kelly, PT, ATC
Penn State Hershey Bone and Joint Institute, 717-531-5638 awren@hmc.psu.edu Physical Therapist, Certified Athletic Trainer
Associate Professor, Department of Family and Community Medicine Team Physical Therapist, Hershey Bears Hockey Club
Bret Jacobs, D.O.
Medical Director, Penn State Hershey Medical Group—
bjacobs@hmc.psu.edu Scott Deihl, ATC, PTA
Elizabethtown, 717-361-0666
Assistant Professor, Departments of Family and Community Medicine Physical Therapist Assistant, Certified Athletic Trainer
and Orthopaedics
ORTHOPAEDIC SPORTS MEDICINE Tanya Deihl, ATC, PTA
Penn State Hershey Medical Group—Middletown, 717-948-5180
Physical Therapist Assistant, Certified Athletic Trainer,
Penn State Hershey Bone and Joint Institute, 717-531-5638 Kevin Black, M.D.
Athletic Trainer, Annville Cleona High School
kblack@hmc.psu.edu
Cayce Onks, D.O. Professor and C. McCollister Evarts Chair John Wawrzyniak, MS, ATC, PT, CSCS
conks@hmc.psu.edu Penn State Hershey Orthopaedics Physical Therapist, Certified Athletic Trainer
Assistant Professor, Departments of Family and Community Medicine Penn State Hershey Bone and Joint Institute, 717- 531-5638 Strength & Conditioning Specialist, Hershey Bears Hockey Club
and Orthopaedics
Penn State Hershey Medical Group—Palmyra, 717-838-6305 Aman Dhawan, M.D.
Penn State Hershey Bone and Joint Institute, 717-531-5638 adhawan@hmc.psu.edu
Assistant Professor, Department of Orthopaedics
Penn State Hershey Bone and Joint Institute, 717-531-5638
4
FCM-9228-16 022216You can also read