IMPACT OF SEVERE ACUTE RESPIRATORY SYNDROME CORONAVIRUS 2 (SARS-COV-2) VARIANT-ASSOCIATED RECEPTOR BINDING DOMAIN (RBD) MUTATIONS ON THE ...
←
→
Page content transcription
If your browser does not render page correctly, please read the page content below
Clinical Infectious Diseases
Major Article
Impact of Severe Acute Respiratory Syndrome
Coronavirus 2 (SARS-CoV-2) Variant-Associated
Receptor Binding Domain (RBD) Mutations on
the Susceptibility to Serum Antibodies Elicited by
Downloaded from https://academic.oup.com/cid/advance-article/doi/10.1093/cid/ciab656/6328361 by guest on 28 August 2021
Coronavirus Disease 2019 (COVID-19) Infection or
Vaccination
Lin-Lei Chen,1,a Lu Lu,1,a Charlotte Yee-Ki Choi,1 Jian-Piao Cai,1 Hoi-Wah Tsoi,1 Allen Wing-Ho Chu,1 Jonathan Daniel Ip,1 Wan-Mui Chan,1
Ricky Ruiqi Zhang,1 Xiaojuan Zhang,1 Anthony Raymond Tam,2 Daphne Pui-Ling Lau,3 Wing-Kin To,4 Tak-Lun Que,5 Cyril Chik-Yan Yip,6 Kwok-Hung Chan,1
Vincent Chi-Chung Cheng,6 Kwok-Yung Yuen,1,6 Ivan Fan-Ngai Hung,2,7 and Kelvin Kai-Wang To1,6
1
State Key Laboratory for Emerging Infectious Diseases, Carol Yu Centre for Infection, Department of Microbiology, Li Ka Shing Faculty of Medicine, The University of Hong Kong, Pokfulam,
Hong Kong Special Administrative Region, People’s Republic of China; 2Department of Medicine, Queen Mary Hospital, Hong Kong Special Administrative Region, People’s Republic of China;
3
Department of Medicine and Geriatrics, Princess Margaret Hospital, Hong Kong Special Administrative Region, People’s Republic of China; 4Department of Pathology, Princess Margaret Hospital,
Hong Kong Special Administrative Region, People’s Republic of China; 5Department of Pathology, Tuen Mun Hospital, Hong Kong Special Administrative Region, People’s Republic of China;
6
Department of Microbiology, Queen Mary Hospital, Hong Kong Special Administrative Region, People’s Republic of China; and 7Division of Infectious Diseases, Department of Medicine, Li Ka
Shing Faculty of Medicine, The University of Hong Kong, Pokfulam,Hong Kong Special Administrative Region, People’s Republic of China
Background. Several severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) lineages with mutations at the spike protein
receptor binding domain (RBD) have reduced susceptibility to antibody neutralization, and have been classified as variants of concern
(VOCs) or variants of interest (VOIs). Here we systematically compared the neutralization susceptibility and RBD binding of different
VOCs/VOIs, including B.1.617.1 (kappa variant) and P.3 (theta variant), which were first detected in India and the Philippines, respectively.
Methods. The neutralization susceptibility of the VOCs/VOIs (B.1.351, B.1.617.1, and P.3) and a non-VOC/VOI without RBD
mutations (B.1.36.27) to convalescent sera from coronavirus disease 2019 (COVID-19) patients or BNT162b2 vaccinees was deter-
mined using a live virus microneutralization (MN) assay. Serum immunoglobulin G (IgG) binding to wild-type and mutant RBDs
were determined using an enzyme immunoassay.
Results. The geometric mean neutralization titers (GMT) of B.1.351, P.3, and B.1.617.1 were significantly lower than that of
B.1.36.27 for COVID-19 patients infected with non-VOCs/VOIs (3.4- to 5.7-fold lower) or individuals who have received 2 doses of
BNT162b2 vaccine (4.4- to 7.3-fold lower). The GMT of B.1.351 or P.3 were lower than that of B.1.617.1. For the 4 patients infected
with B.1.351 or B.1.617.1, the MN titer was highest for their respective lineage. RBD with E484K or E484Q mutation, either alone or
in combination with other mutations, showed greatest reduction in serum IgG binding.
Conclusions. P.3 and B.1.617.1 escape serum neutralization induced by natural infection or vaccine. Infection with 1 variant
does not confer cross-protection for heterologous lineages. Immunogenicity testing for second generation COVID-19 vaccines
should include multiple variant and “nonvariant” strains.
Keywords. variant of concern; neutralization; COVID-19 vaccine; reinfection; receptor binding domain.
Since the beginning of the coronavirus disease 2019 (COVID- carrying spike D614G mutation have spread globally since
19) pandemic, severe acute respiratory syndrome coronavirus March 2020 [3]. A single novel lineage can cause large out-
2 (SARS-CoV-2) has evolved into many lineages [1, 2]. Viruses breaks in places with low incidence. For example, the B.1.1.63
lineage and B.1.36.27 lineage dominated the third and fourth
wave in Hong Kong, respectively [4, 5].
The spike protein receptor binding domain (RBD) is respon-
Received 4 June 2021; editorial decision 20 July 2021; published online 26 July 2021.
a
L.-L. C. and L. L. contribute equally to this work. sible for binding to host cell receptor angiotensin-converting
Correspondence: K. K.-W. To, Carol Yu Centre for Infection, State Key Laboratory of Emerging enzyme 2 (ACE2) and is the major target of neutralizing anti-
Infectious Diseases, Department of Microbiology, Li Ka Shing Faculty of Medicine, The
University of Hong Kong, Queen Mary Hospital, Pokfulam, Hong Kong, China (kelvinto@hku.hk).
bodies [6]. RBD mutations may increase infectivity and trans-
Clinical Infectious Diseases® 2021;XX(XX):1–8 missibility, confer an increased risk of reinfection, and reduce
© The Author(s) 2021. Published by Oxford University Press for the Infectious Diseases Society vaccine efficacy [7]. In late 2020 and early 2021, variants with
of America. All rights reserved. For permissions, e-mail: journals.permissions@oup.com.
https://doi.org/10.1093/cid/ciab656
N501Y mutations at the RBD were reported to spread rapidly
SARS-CoV-2 Variants Neutralization • cid 2021:XX (XX XXXX) • 1in the United Kingdom (B.1.1.7), South Africa (B.1.351), and B.1.36.27 lineage virus was isolated from the nasopharyngeal
Brazil (P.1). The B.1.1.7 variant (alpha variant; VOC 202012/01) swab of a 4-year old male in February 2021, who acquired the
has been associated with increased transmissibility and mor- virus locally (GISAID EPI_ISL_2423555). The B.1.351 lineage
tality in epidemiological studies [8, 9]. B.1.1.7 variant has better virus was isolated from the posterior oropharyngeal saliva
fitness than earlier D614G lineages in vitro and replicates better of a 43-year-old female who traveled from the Philippines to
in the upper respiratory tract in a hamster model [10]. The Hong Kong in March 2021 (GISAID EPI_ISL_2423556). The
B.1.351 (beta variant; VOC 202012/02) and P.1 (gamma variant; P.3 lineage virus was isolated from the combined nasopharyn-
B.1.1.28.1; VOC202101/02) variants have additional mutations geal/throat swab of a 37-year-old female who traveled from
at spike amino acid residues 417 and 484, and have been found the Philippines in January 2021 (GISAID EPI_ISL_2423558).
to be 4.5- to 8.6-fold less susceptible to neutralization by vaccine The B.1.617.1 lineage virus was isolated from a nasopharyngeal
or natural infection induced antibodies [11]. The P.3 (theta- swab specimen from a 2-year-old male patient who returned
Downloaded from https://academic.oup.com/cid/advance-article/doi/10.1093/cid/ciab656/6328361 by guest on 28 August 2021
variant; B.1.1.28.3) variant, which has the same ancestor as P.1 from India in April 2021 (GISAID EPI_ISL_2423557). Written
and carries mutation N501Y and E484K, is prevalent in the informed consent was waived by the IRB committee for the
Philippines [12]. At the time of writing, 80% of the P.3 lineage use of archived clinical specimens for viral culture. This study
viruses were found in the Philippines [13]. The World Health was approved by Institutional Review Board of the University
Organization has classified B.1.1.7, B.1.351, and P.1 as variants of Hong Kong/ Hospital Authority Hong Kong West Cluster
of concern (VOCs), and P.3 as a variant of interest (VOI) [14]. (HKU/HA HKW IRB) (UW 13–265 and UW 21–214) and the
Apart from variants with N501Y mutation, viruses with Kowloon West Cluster REC (KW/EX-20–038[144-26]).
spike L452R mutation have also been found. The variants
B.1.427/B.1.429 (epsilon variant) with L452R spread rapidly in Virus Culture and Live Virus Microneutralization Assay
California and have reduced neutralizing antibody titer [15]. Viral culture and live virus MN assay were conducted in the
Since March 2021, there has been a rapid increase in the inci- Biosafety Level 3 facility at the University of Hong Kong as we
dence of COVID-19 in India [16]. The number of cases exceeded described previously [18]. Viral culture was conducted using
400 000 per day. This massive outbreak was associated with a TMPRSS2-overexpressing VeroE6 cells (VeroE6/TMPRSS2
novel lineage B.1.617 with L452R and/or E484Q mutation at the cells) (JCRB Cell Bank Catalogue no. JCRB1819) to avoid mu-
spike RBD. On 11 May 2021, the World Health Organization tations which may arise during culture in normal VeroE6 cells.
has declared B.1.617 as the fourth VOC [14]. B.1.617.1 (kappa Live virus neutralization assay was performed as we de-
variant) was later reclassified as a VOI on 31 May 2021. This scribed previously with modifications [18, 19]. Briefly, serum
study systematically compared the effect of neutralization and specimens were serially diluted in 2-folds starting from 1:10.
immunoglobulin G (IgG) binding that are conferred by these Duplicates of each serum dilution was mixed with 100 TCID50
variants or RBD mutations. We included serum specimens from of B.1.36.27, B.1.351, P.3 or B.1.617.1 virus isolates for 1 hour,
recovered COVID-19 patients, including a patient with reinfec- and the serum-virus mixture was then added to VeroE6/
tion we reported previously [17], or BNT162b2 messenger RNA TMPRSS2 cells. After incubation for 3 days, cytopathic effect
(mRNA) vaccine recipients, including 2 with prior COVID-19. was visually scored for each well by 2 independent observers.
The results were plotted using 5-parameter dose-response curve
in GraphPad Prism version 9.1.1. A value of 5 was assigned if
METHODS
cytopathic effect was seen at a dilution of 1:10.
Clinical Specimens
Serum specimens were collected from recovered COVID-19 Expression and Purification of RBD
patients of Queen Mary Hospital or Princess Margaret Hospital Recombinant RBD (residues 306–543) of SARS-CoV-2 spike
and from BNT162b2 vaccine recipients. COVID-19 patients protein from the reference sequence Wuhan-Hu-1 (GenBank
were diagnosed by reverse transcription polymerase chain re- ID YP_009724390.1) (wild type) or with the mutations N501Y,
action (RT-PCR) at the Clinical Microbiology Laboratory of N501Y-E484K-K417N, L452R-E484Q, E484K, L452R or
Queen Mary Hospital or at the Public Health Laboratory Centre N439K were expressed and purified in insect cells as we de-
of Hong Kong. BNT162b2 vaccine recipients received the vac- scribed previously with modifications [20] (Supplementary
cine in Hong Kong. For COVID-19 patients, serum specimens Figure 1). Briefly, RBD gene sequences were baculovirus-
were randomly selected for live virus microneutralization assay codon-optimized and cloned into pFast dual baculovirus ex-
(MN) or RBD assay. For vaccine recipients, all recruited pa- pression vector. The constructs were fused with an N-terminal
tients as of 15 May 2021, were included. Written informed con- gp67 signal peptide and C-terminal 6×His tag for secretion
sent was obtained. and purification. A recombinant bacmid DNA was gener-
All SARS-CoV-2 viruses were isolated from respiratory spe- ated using the Bac-to-Bac system (Thermo Fisher Scientific).
cimens collected from patients in Hong Kong (Figure 1). The Baculovirus was produced by transfecting purified bacmid
2 • cid 2021:XX (XX XXXX) • Chen et alDownloaded from https://academic.oup.com/cid/advance-article/doi/10.1093/cid/ciab656/6328361 by guest on 28 August 2021
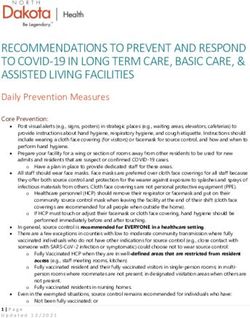
Figure 1. Whole-genome phylogenetic analysis showing the culture isolates used for the microneutralization antibody assay in this study. The phylogenetic tree is
constructed using maximum likelihood method. Culture isolates used in the microneutralization assays are shown in blue. Tree was rooted using the reference genome
Wuhan-Hu-1 (GenBank accession no. MN908947.3).
DNA into Sf9 cells using Cellfectin (Thermo Fisher Scientific) of His-tagged SARS-CoV-2 spike RBD in 0.05 M carbonate bi-
and subsequently used to infect ExpiSf9 cell suspension cul- carbonate buffer (pH 9.6) overnight at 4° C and then followed
ture (Thermo Fisher Scientific) at a multiplicity of infection of by incubation with a blocking reagent. After blocking, 100 μL
1 to 10. Infected ExpiSf9 cells were incubated at 27.5° C with heat-inactivated serum samples at 1:200 dilution were added
shaking at 125 rpm for 96 hours for protein expression. The su- to the wells and incubated at 37° C for 1 hour. The attached
pernatant was collected and then concentrated using a 10 kDa human and mouse antibodies were detected using horseradish-
MW cutoff Labscale TFF System (Millipore). The RBD pro- peroxidase-conjugated goat anti-human IgG and anti-mouse
tein was purified by Ni-NTA purification system, followed by IgG antibody respectively (Invitrogen, Thermo Fisher Scientific,
size exclusion chromatography, and buffer exchanged into 1× Waltham, Massachusetts, USA). The reaction was developed by
phosphate-buffered saline (PBS) pH 7.4. The concentration of adding diluted 3,3′,5,5′-tetramethylbenzidine single solution
purified RBD was determined by using the Bradford Assay Kit and stopped with 0.3 N H2SO4. The optical density (OD) was
(Bio-Rad) according to the manufacturer’s instructions. The read at 450 and 620 nm. For normalization, mouse monoclonal
purity of recombinant RBD mutants were verified by western antibody against His tag (ABclonal, ABclonal, Inc., Woburn,
blotting (Supplementary Figure 2). Massachusetts, USA) was diluted in a series of 2-fold dilution
from 1:3000, and the EC50 for each RBD was determined using
Anti-RBD Assay for Wild Type and Variants the 5-parameter logistic equation.
Enzyme immunoassay for anti-RBD IgG antibody was per-
formed as we described previously with modifications [21, Whole Viral Genome Sequencing and Bioinformatics Analysis
22]. Briefly, 96-well immunoplates (Nunc Immuno modules; Whole viral genome sequencing was performed using nanopore
Nunc, Denmark) were coated with 100 μL/well (0.2 μg/well) sequencing following the Nanopore protocol PCR tiling of
SARS-CoV-2 Variants Neutralization • cid 2021:XX (XX XXXX) • 3COVID-19 (Version: PTC_9096_v109_revH_06Feb2020) ac- B.1.36.27 was higher than VOC/VOI strains for 7 patients
cording to the manufacturer’s instructions with minor modi- (Figure 2A). The geometric mean titer (GMT) of B.1.351 and P.3
fications (Oxford Nanopore Technologies) as we described was 5.7-fold and 5.1-fold lower than that of B.1.36.27. The GMT
previously [4, 5, 23]. For bioinformatics analysis, the recom- of B.1.617.1 was 3.4-fold lower than that of B.1.36.27, almost
mended ARTIC bioinformatics workflow was used with minor reaching statistical significance (P = .066). The GMT against P.3
modifications applied as described previously [4, 5]. Please was significantly lower than that of B.1.617.1 (P = .0339).
refer to Supplementary methods for details. Next, we tested the serum of 12 individuals who have re-
ceived 2 doses of BNT162b2 and without prior infection. At
Statistics 21 or 28 days after the first dose, 6 individuals (50%) had de-
All statistical analysis was performed using PRISM version tectable levels of MN antibody against B.1.36.27 (Figure 2B),
but 3 vaccinees did not have detectable MN antibody against
Downloaded from https://academic.oup.com/cid/advance-article/doi/10.1093/cid/ciab656/6328361 by guest on 28 August 2021
9.1.1. The MN titers or normalized OD values were compared
between different viruses or RBDs using 1-way analysis of var- the VOC/VOIs B.1.351, P.3 or B.1.617.1. The GMT of B.1.351,
iance (ANOVA) with Tukey’s multiple comparisons test. A P P.3 and B.1.617.1 were lower than that of B.1.36.27 after 1 dose
value ofDownloaded from https://academic.oup.com/cid/advance-article/doi/10.1093/cid/ciab656/6328361 by guest on 28 August 2021
Figure 3. Comparison of microneutralization antibody titers for (A) sera from vaccinees with prior COVID-19 and a patient with reinfection with non-VOC/VOI lineages; (B)
sera from patients infected with VOC/VOI lineages. Abbreviations: COVID-19, coronavirus disease 2019; VOC, variant of concern; VOI, variants of interest.
whereas the 2 patients infected with B.1.617.1 had highest titer lineage virus, L452R-E484Q and L452R had similar OD as
against B.1.617.1 (Figure 3B). Notably, for 1 of the patients in- wild type and N501Y, but L452R had significantly higher OD
fected with B.1.617.1, the MN titer against B.1.617.1 virus (MN than N501Y-E484K-K417N (P = .0171) (Figure 4C). For the 3
titer: 269) was at least 7-fold higher than other viruses tested patients with B.1.351, the OD was higher for N501Y-E484K-
(MN titer: 20–38). K417N RBD than for L452R or L452R-E484K RBD (Figure 4D).
RBD Binding
DISCUSSION
Next, we assessed the binding of convalescent-phase or vac-
cine serum for recombinant RBDs using enzyme immuno- SARS-CoV-2 variants with RBD mutations are particularly
assay (Supplementary Table 3). The recombinant RBD tested worrisome as these are more likely to escape humoral immunity
include the wild-type virus, the VOCs (N501Y, N501Y-E484K- induced by natural infection or COVID-19 vaccine. Previous
K417N), a VOI (E484K, representative of VOI B.1.525 [eta var- studies suggested that B.1.351 and P.1 variants have reduced
iant]; L452R; L452R-E484Q), and a mink-associated mutation, susceptibility to neutralization by antibodies induced by vac-
N439K [24]. cine or natural infection due to non-VOC/VOI viruses [25].
For sera from non-VOC/VOI patients, wild-type and N501Y However, the data on B.1.617.1, which emerged in India, and
RBD had similar OD values, and both had significantly higher P.3, which emerged in the Philippines, are scarce. In this study,
OD than all other mutants (P ≤ .0001 for all comparisons) we simultaneously compared neutralization susceptibility of
(Figure 4A). L452R and N439K RBD had similar ODs, and B.1.617.1, P.3, and B.1.351 (all carrying mutations at amino acid
both were significantly higher than the RBDs that contain mu- position 484) with a D614G virus without RBD mutations. We
tation at spike amino acid residue 484 (N501Y-E484K-K417N, also determined the effect of RBD binding due to different mu-
E484K, L452R-E484Q). In particular, the mean OD of L452R tations at amino acid residue 417, 439, 452, 484, and 501, which
(1.411; standard error of the mean [SEM], 0.263) was 1.26-fold are present alone or in combination among VOCs or VOIs. We
higher than that of L452R-E484Q (1.141; SEM, 0.263). There showed that both B.1.617.1 and P.3 confer reduced suscepti-
was no significant differences between the OD values for 3 lin- bility to sera from mRNA vaccinee or from COVID-19 patients
eages that contain mutation at spike amino acid residue 484. infected with non-VOC/VOI strains. Notably, the reduction of
The results for BNT162b2 vaccine recipient was similar to that P.3 is similar to that of B.1.351, while the reduction of B.1.617.1
of non-VOC/VOI patients, in that wild-type and N501Y RBD is slightly less than those of P.3 or B.1.351. Furthermore, we
had the highest OD, followed by L452R and N439K, with the showed that mutation at spike amino acid mutation 484, either
E484K, L452R-E484Q, and N501Y-E484K-K417N RBD having alone or in combination with other RBD mutations, confer the
the lowest OD (Figure 4B). greatest reduction in serum IgG binding.
We also tested the sera from 9 patients with VOCs/VOIs, We showed that B.1.617.1 with L452R-E484Q mutation had
including the sera from the 4 patients tested with neutraliza- 3.4-fold and 4.4-fold lower MN titer than B.1.36.27 for non-
tion assay. For serum from 6 patients infected with B.1.617.1 VOC/VOI patients and vaccine recipients, respectively. Our
SARS-CoV-2 Variants Neutralization • cid 2021:XX (XX XXXX) • 5Downloaded from https://academic.oup.com/cid/advance-article/doi/10.1093/cid/ciab656/6328361 by guest on 28 August 2021 Figure 4. Impact of RBD mutations on antibody binding. OD measured at 450 nm and corrected at 620 nm. Abbreviations: OD, optical density; RBD, receptor binding domain; VOC, variant of concern; VOI, variants of interest. results concur with recent studies, which showed a reduction of Our data showed that the neutralization titer against P.3 is neutralizing antibody titer ranging from 1.94-fold to 7.17-fold similar to that of B.1.351 for both vaccinee and non-VOC/ for vaccine recipients [26–28], and 1.96- to 6.5-fold reduction for VOI COVID-19 patients, although P.3 lacks the K417N mu- convalescent sera [24, 28]. Our RBD binding assay showed that tation in B.1.351. In addition to the spike RBD mutations, both the single L452R or the double L452R-E484Q mutations P.3 lineage virus also contains the spike NTD mutation 141- affect IgG binding, but the magnitude of reduction is greater for 143del, and the furin cleavage site mutation P681H, which L452R-E484Q. Previous study also showed that E484K or L452R is also found in the B.1.1.7 lineage [14]. Whether these mu- alone reduced the binding of some monoclonal antibodies [29]. tations help the virus to escape neutralization remain to be The mutation L452R is also present in the B.1.427/B.1.429 lin- determined. eages from California, which are more resistant to neutraliza- B.1.617.1, B.1.351, and P.3 carry mutation at spike amino tion by serum than nonvariant viruses [15]. Taken together, both residue 484, and our RBD binding assay showed that RBDs L452R and E484Q are important in contributing to the reduced with mutation at residue 484 had the greatest reduction in IgG susceptibility to neutralization. binding from patients or vaccinees. E484K alone reduced the 6 • cid 2021:XX (XX XXXX) • Chen et al
binding of RBD to human ACE2 and affected the binding of [36], has greatest effect on antibody binding. Antibody induced
some monoclonal antibodies [29]. Previous study on B.1.525 by natural infection from a variant virus may not protect vari-
lineage, which carries E484K without other spike RBD muta- ants with other RBD mutations. Hence, immunogenicity testing
tions, had a slightly lower neutralizing antibody titer than the for newer generation COVID-19 vaccines should evaluate vir-
wild-type virus for BNT162b2 vaccinees or convalescent sera uses from lineages carrying different spike mutations.
[30, 31].
For patients infected with B.1.617.1 or B.1.351, their Supplementary Data
Supplementary materials are available at Clinical Infectious Diseases online.
serum MN titers against the virus from their respective lin-
Consisting of data provided by the authors to benefit the reader, the posted
eages were much higher than other lineages, including the materials are not copyedited and are the sole responsibility of the authors,
B.1.36.27 lineage without any RBD mutations. Our result con- so questions or comments should be addressed to the corresponding author.
curs with the study by Cele et al [32], which showed that sera
Downloaded from https://academic.oup.com/cid/advance-article/doi/10.1093/cid/ciab656/6328361 by guest on 28 August 2021
Notes
from patients infected with B.1.351 had reduced neutraliza-
Acknowledgments. The authors gratefully acknowledge the originating
tion against earlier viruses. The reduced cross-neutralization and submitting laboratories who contributed sequences to GISAID
against heterologous viruses, including non-VOC/VOI (Supplementary Table 4).
strains, has implications on reinfection and vaccine design. Financial support. This study was partly supported by Health and Medical
Research Fund (HMRF), the Food and Health Bureau, The Government of
First, patients infected B.1.617.1 or P.3 lineage viruses are the Hong Kong Special Administrative Region (Ref No. COVID190124);
still susceptible to reinfection from viruses without RBD mu- Consultancy Service for Enhancing Laboratory Surveillance of Emerging
tations or other RBD mutations. Second, testing for second Infectious Diseases and Research Capability on Antimicrobial Resistance
for Department of Health of the HKSAR; and donations of Richard Yu and
generation COVID-19 vaccines should include viruses from Carol Yu, Shaw Foundation Hong Kong, Michael Seak-Kan Tong, May Tam
ancestral D614G lineage and variant lineages with different Mak Mei Yin, Lee Wan Keung Charity Foundation Limited, Hong Kong
RBD mutations. Sanatorium & Hospital, Respiratory Viral Research Foundation Limited,
Hui Ming, Hui Hoy and Chow Sin Lan Charity Fund Limited, Chan Yin
For the patient with reinfection due to D614G and a vac-
Chuen Memorial Charitable Foundation, Marina Man-Wai Lee, the Hong
cine recipient with prior COVID-19 infection, their MN titers Kong Hainan Commercial Association South China Microbiology Research
against B.1.617.1 was similar to those of B.1.36.27, although Fund, the Jessie & George Ho Charitable Foundation, Kai Chong Tong, Tse
the MN titers against B.1.351 and P.3 were lower. Because there Kam Ming Laurence, Foo Oi Foundation Limited, Betty Hing-Chu Lee, and
Ping Cham So. The funding sources had no role in study design, data col-
have not been any locally acquired cases with L452R variants in lection, analysis, interpretation, or writing of the report.
Hong Kong, it is unlikely that these individuals have prior expo- Potential conflicts of interest. The authors: No reported conflicts of
sure to B.1.617.1 lineage viruses. interest. All authors have submitted the ICMJE Form for Disclosure of
Potential Conflicts of Interest. Conflicts that the editors consider relevant to
N439K mutation confers reduced serum IgG binding the content of the manuscript have been disclosed.
when compared with wild type. N439K is found in different
SARS-CoV-2 lineages, including mink-associated human References
cases [33]. Our findings corroborate with previous studies 1. To KK, Sridhar S, Chiu KH, et al. Lessons learned one year after SARS-CoV-2
emergence leading to COVID-19 pandemic. Emerg Microbes Infect 2021;
that showed reduced susceptibility to monoclonal anti- 10:507–35.
bodies [33]. 2. Rambaut A, Holmes EC, O’Toole Á, et al. A dynamic nomenclature proposal
for SARS-CoV-2 lineages to assist genomic epidemiology. Nat Microbiol 2020;
There are several limitations in this study. First, we only tested 5:1403–7.
1 virus from each lineage. There may be differences in neutral- 3. Korber B, Fischer WM, Gnanakaran S, et al; Sheffield COVID-19 Genomics
Group. Tracking changes in SARS-CoV-2 Spike: evidence that D614G increases
ization susceptibility among viruses within the same lineage.
infectivity of the COVID-19 virus. Cell 2020; 182:812–27.e19.
Second, there are relatively few patients infected with variants. 4. To KK, Chan WM, Ip JD, et al. Unique SARS-CoV-2 clusters causing a large
Third, we have not examined the binding to spike N-terminal COVID-19 outbreak in Hong Kong. Clin Infect Dis 2021; 73:137–42.
5. Chan WM, Ip JD, Chu AW, et al. Phylogenomic analysis of COVID-19 summer
domain or S2 subunit, which are also targets of monoclonal and winter outbreaks in Hong Kong: an observational study. Lancet Reg Health
neutralizing antibodies [6, 34, 35]. Fourth, we currently do not West Pac 2021; 10:100130.
6. Andreano E, Nicastri E, Paciello I, et al. Extremely potent human mon-
have any clinical data regarding reinfection or vaccine efficacy oclonal antibodies from COVID-19 convalescent patients. Cell 2021;
against B.1.617.1 and P.3. Finally, we did not assess T-cell im- 184:1821–35.e16.
7. Harvey WT, Carabelli AM, Jackson B, et al; COVID-19 Genomics UK (COG-UK)
munity of these patients, which is also important for protection. Consortium. SARS-CoV-2 variants, spike mutations and immune escape. Nat Rev
In conclusion, our results suggest that both B.1.617.1 and Microbiol 2021; 19:409–24.
8. Davies NG, Abbott S, Barnard RC, et al. Estimated transmissibility and impact of
P.3 are less susceptible to neutralization, which may affect vac-
SARS-CoV-2 lineage B.1.1.7 in England. Science 2021; 372:eabg3055.
cine effectiveness and the risk of reinfection. Although many 9. Davies NG, Jarvis CI, Edmunds WJ, Jewell NP, Diaz-Ordaz K, Keogh RH;
recovered COVID-19 patients or vaccinees still have relatively CMMID COVID-19 Working Group. Increased mortality in community-tested
cases of SARS-CoV-2 lineage B.1.1.7. Nature 2021; 593:270–4.
high titers of neutralizing antibody against the variants, the de- 10. Mok BW-Y, Liu H, Lau S-Y, et al. Low dose inocula of SARS-CoV-2 B.1.1.7 variant
cline of antibody level over time may predispose these patients initiate more robust infections in the upper respiratory tract of hamsters than earlier
D614G variants. bioRxiv 2021. doi:https://doi.org/10.1101/2021.04.19.440414.
to be more susceptible to variants. Mutations at the spike amino 11. Abdool Karim SS, de Oliveira T. New SARS-CoV-2 Variants: clinical, public
acid residue 484, located at the key region of antibody binding health, and vaccine implications. N Engl J Med 2021; 384:1866–8.
SARS-CoV-2 Variants Neutralization • cid 2021:XX (XX XXXX) • 712. Tablizo FA, Kim KM, Lapid CM, et al. Genome sequencing and analysis of an 25. Garcia-Beltran WF, Lam EC, St Denis K, et al. Multiple SARS-CoV-2 variants es-
emergent SARS-CoV-2 variant characterized by multiple spike protein muta- cape neutralization by vaccine-induced humoral immunity. Cell 2021; 184:2523.
tions detected from the Central Visayas Region of the Philippines. medRxiv 2021. 26. Yadav PD, Sapkal GN, Abraham P, et al. Neutralization potential of Covishield
Available at: https://doi.org/10.1101/2021.03.03.21252812. vaccinated individuals sera against B.1.617.1. Clin Infect Dis 2021; doi:10.1093/
13. PANGO lineages. Lineage P.3. Available at: https://cov-lineages.org/lineage. cid/ciab483.
html?lineage=P.3. Accessed 29 May 2021. 27. Yadav PD, Sapkal GN, Abraham P, et al. Neutralization of variant under investi-
14. World Health Organization. Weekly epidemiological update on COVID-19: gation B.1.617 with sera of BBV152 vaccinees. Clin Infect Dis 2021; doi:10.1093/
25 May 2021. Available at: https://www.who.int/publications/m/item/weekly- cid/ciab411.
epidemiological-update-on-covid-19---25-may-2021. Accessed 29 May 2021. 28. Edara V-V, Lai L, Sahoo MK, et al. Infection and vaccine-induced neutralizing
15. Deng X, Garcia-Knight MA, Khalid MM, et al. Transmission, infectivity, and neu- antibody responses to the SARS-CoV-2 B.1.617.1 variant. N Engl J Med 2021;
tralization of a spike L452R SARS-CoV-2 variant. Cell 2021; 184:3426–37.e8. NEJMc2107799. doi:10.1056/NEJMc2107799.
16. Mallapaty S. India’s massive COVID surge puzzles scientists. Nature 2021; 29. Yuan M, Huang D, Lee CD, et al. Structural and functional ramifications of an-
592:667–8. tigenic drift in recent SARS-CoV-2 variants. Science 2021; doi:10.1126/science.
17. To KK, Hung IF, Ip JD, et al. COVID-19 re-infection by a phylogenetically distinct abh1139.
SARS-coronavirus-2 strain confirmed by whole genome sequencing. Clin Infect 30. Shi PY, Liu J, Liu Y, et al. Neutralization of SARS-CoV-2 variants B.1.617.1 and
Downloaded from https://academic.oup.com/cid/advance-article/doi/10.1093/cid/ciab656/6328361 by guest on 28 August 2021
Dis 2020; doi:10.1093/cid/ciaa1275. B.1.525 by BNT162b2-elicited sera. Res Sq 2021; doi:1021203/rs3rs-540721/v1.
18. To KK, Tsang OT, Leung WS, et al. Temporal profiles of viral load in posterior 31. Jangra S, Ye C, Rathnasinghe R, et al. The E484K mutation in the SARS-CoV-2
oropharyngeal saliva samples and serum antibody responses during infection by spike protein reduces but does not abolish neutralizing activity of human conva-
SARS-CoV-2: an observational cohort study. Lancet Infect Dis 2020; 20:565–74. lescent and post-vaccination sera. medRxiv 2021. doi:10.1101/2021.01.26.212505
19. To KK, Hung IF, Chan KH, et al. Serum antibody profile of a patient with corona- 43:2021.01.26.21250543.
virus disease 2019 reinfection. Clin Infect Dis 2021; 72:e659–62. 32. Cele S, Gazy I, Jackson L, et al; Network for Genomic Surveillance in South
20. Markovitz D, Chan JF, Oh YJ, et al. A molecularly engineered, broad-spectrum Africa; COMMIT-KZN Team. Escape of SARS-CoV-2 501Y.V2 from neutraliza-
anticoronavirus lectin inhibits SARS-CoV-2 and MERS-CoV infection in vivo. tion by convalescent plasma. Nature 2021; 593:142–6.
Res Sq 2021; doi:1021203/rs3rs-516695/v1. 33. Thomson EC, Rosen LE, Shepherd JG, et al; ISARIC4C Investigators; COVID-19
21. To KK, Cheng VC, Cai JP, et al. Seroprevalence of SARS-CoV-2 in Hong Kong and Genomics UK (COG-UK) Consortium. Circulating SARS-CoV-2 spike N439K
in residents evacuated from Hubei province, China: a multicohort study. Lancet variants maintain fitness while evading antibody-mediated immunity. Cell 2021;
Microbe 2020; 1:e111–e118. 184:1171–87.e20.
22. Fong CH, Cai JP, Dissanayake TK, et al. Improved detection of antibodies against 34. Liu L, Wang P, Nair MS, et al. Potent neutralizing antibodies against multiple
SARS-CoV-2 by microsphere-based antibody assay. Int J Mol Sci 2020; 21:6595. epitopes on SARS-CoV-2 spike. Nature 2020; 584:450–6.
23. Ip JD, Kok KH, Chan WM, et al. Intra-host non-synonymous diversity at a neu- 35. Voss WN, Hou YJ, Johnson NV, et al. Prevalent, protective, and convergent
tralizing antibody epitope of SARS-CoV-2 spike protein N-terminal domain. Clin IgG recognition of SARS-CoV-2 non-RBD spike epitopes. Science 2021;
Microbiol Infect 2020;S1198-743X(20)30661-3. 372:1108–12.
24. Hoffmann M, Zhang L, Krüger N, et al. SARS-CoV-2 mutations acquired in mink 36. Tegally H, Wilkinson E, Giovanetti M, et al. Detection of a SARS-CoV-2 variant
reduce antibody-mediated neutralization. Cell Rep 2021; 35:109017. of concern in South Africa. Nature 2021; 592:438–43.
8 • cid 2021:XX (XX XXXX) • Chen et alYou can also read