Intraoperative Avidination for RadionuclideTherapy: A Prospective New Development to Accelerate Radiotherapy in Breast Cancer
←
→
Page content transcription
If your browser does not render page correctly, please read the page content below
Intraoperative Avidination for RadionuclideTherapy: A Prospective
New Development to Accelerate Radiotherapy in Breast Cancer
Giovanni Paganelli,1 Mahila Ferrari,2 Laura Ravasi,1 Marta Cremonesi,2 Concetta De Cicco,1
Viviana Galimberti,3 Gregory Sivolapenko,5 Alberto Luini,3 Rita De Santis,6
Laura Lavinia Travaini,1 Maurizio Fiorenza,1 Marco Chinol,1 Stefano Papi,1
Claudio Zanna,6 Paolo Carminati,6 and Umberto Veronesi3,4
Abstract Purpose: In a continuous effort to seek for anticancer treatments with minimal side effects, we
aim at proving the feasibility of the Intraoperative Avidination for RadionuclideTherapy, a new pro-
cedure for partial breast irradiation.
Experimental Design: To assess doses of 90Y-DOTA-biotin to target (i.e., breast tumor bed)
and nontarget organs, we did simulation studies with 111In-DOTA-biotin in 10 candidates for con-
servative breast surgery. Immediately after quadrantectomy, patients were injected with 100-mg
avidin in the tumor bed. On the following day, patients were given 111In-DOTA-biotin (f111MBq)
i.v. after appropriate chase of biotinylated albumin (20 mg) to remove circulating avidin. Biokinetic
studies were done by measuring radioactivity in scheduled blood samples, 48-h urine collection,
and through scintigraphic images. The medical internal radiation dose formalism (OLINDA code)
enabled dosimetry assessment in target and nontarget organs.
Results: Images showed early and long-lasting radioactive biotin uptake in the operated breast.
Rapid blood clearance (75% at 24 h) were observed. Absorbed
doses, expressed as mean F SD in Gy/GBq, were as low as 0.15 F 0.05 in lungs, 0.10 F 0.02 in
heart, 0.06 F 0.02 in red marrow, 1.30 F 0.50 in kidneys, 1.50 F 0.30 in urinary bladder, and 0.06
F 0.02 in total body, whereas in the targeted area, they increased to 5.5 F 1.1 Gy/GBq (50%
ISOROI) and 4.8 F 1.0 Gy/GBq (30% ISOROI).
Conclusion: Our preliminary results suggest that Intraoperative Avidination for Radionuclide
Therapy is a simple and feasible procedure that may improve breast cancer patients’ postsurgical
management by shortening radiotherapy duration.
Breast conservative surgery, with sentinel node biopsy and Based on our previous clinical experience in locoregional
postoperative regional radiotherapy, represents the treatment of treatment of peritoneal carcinomatosis and recurrent high-
choice in patients with early breast cancer (1, 2). Unfortunately, grade glioma using the avidin-biotin pretargeting technique
the duration of a standard course of whole-breast external beam (9 – 11), we foresaw a potential application of 90Y-DOTA-biotin
radiation therapy (EBRT), followed by a boost to the tumor bed, radionuclide therapy in breast cancer. We developed the
is usually 6 to 8 weeks. This can represent a logistics problem for Intraoperative Avidination for Radionuclide Therapy (IART)
many patients, particularly those who are far from a radiation that relies on the avidin-biotin binding system. In fact, the
treatment facility (3). Alternative modalities of accelerated partial ‘‘avidination’’ of the anatomic area of the tumor with native
breast irradiation, such as MammoSite, breast brachytherapy, avidin, directly injected by the surgeon into and around the
three-dimensional Conformal External Beam Radiotherapy, tumor bed, provides a target for the radiolabeled biotin i.v.
interstitial brachytherapy, and single fraction intraoperative injected 1 day later.
radiotherapy, are currently under clinical evaluation (4–8). To prove the feasibility of this new procedure, we first did a
pilot study to optimize the chase of biotinylated albumin to
bind circulating avidin, thus restricting the presence of free
Authors’ Affiliations: Divisions of 1Nuclear Medicine, 2Medical Physics, and avidin in the tumor bed. Consequently, 10 patients with early
3
Senology, European Institute of Oncology; 4European Institute of Oncology, breast cancer, candidates for breast conservative surgery, were
Milan, Italy; 5Department of Pharmacy, Pharmacokinetics Laboratory, University of enrolled in a phase I trial specifically designed to study
Patras, Patras, Greece; and 6R&D, Sigma-Tau SpA, Rome, Italy dosimetry and biodistribution of 90Y-DOTA-biotin in target
Received 5/3/07; accepted 5/16/07.
Grant support: Italian Association for Cancer Research (AIRC).
and nontarget organs through simulation studies based on
111
Presented at the Eleventh Conference on Cancer Therapy with Antibodies and In-DOTA-biotin. Tumor resection was followed by avidin
Immunoconjugates, Parsippany, New Jersey, USA, October 12-14, 2006. injection in the tumor bed. On the following day, patients were
Requests for reprints: Giovanni Paganelli, European Institute of Oncology, Via given 111In-DOTA-biotin i.v. after appropriate chase of bio-
Ripamonti 435, 20141 Milan, Italy. Phone: 39-025-748-9043; Fax: 39-025-748-
9040; E-mail: divisione.medicinanucleare@ ieo.it.
tinylated albumin. Biokinetic studies were based on measured
F 2007 American Association for Cancer Research. radioactivity in timed blood samples, 48-h urine collection,
doi:10.1158/1078-0432.CCR-07-1058 and through scintigraphic images. Our preliminary results
Clin Cancer Res 2007;13(18 Suppl) September 15, 2007 5646s www.aacrjournals.orgIARTand Breast Cancer
suggested 20 mg of biotinylated albumin as the optimal chase biopsy), gave signed, written informed consent to participate in our
dose to remove circulating avidin. The 111In-DOTA-biotin study. In particular, 5 patients were randomly selected for a pilot study
simulation studies to predict dosimetry with 90Y-DOTA-biotin for B-HSA chase optimization and 10 were enrolled in a phase I trial.
Inclusion criteria were performance status (Eastern Cooperative
showed that the mean absorbed dose in nontarget organs
Oncology Group), 0-2; age, 18 to 75 years; life expectancy, >1 year;
was 2, previous biopsy or surgically removed tumor,
(30% ISOROI) in the target area. Images showed early and severe psychiatric disorders, pregnancy, and breast-feeding.
long-lasting radioactive biotin uptake in the operated breast. The study was approved by the Local Ethics Committee (IEO
Rapid blood clearance and urine excretion were observed. S208/504). The patient undergoing the pilot therapeutic study
Such findings led to apply IART with 90Y-DOTA-biotin for the had advanced breast cancer with bone and lung metastases and local
first time in a patient with local breast cancer recurrence, cancer recurrence, characterized by little lumps under the skin of
the right thorax and reddish-pink rashes and swelling of the left
showing an objective response to this new targeted locore-
breast area.
gional therapy.
Pilot study to chase circulating avidin
Materials and Methods To correctly set up the phase I trial, we tested the chase while varying
the quantity and volume of administered avidin and the gap time
Reagents between avidin and biotin injection. In particular, avidin doses ranged
Native avidin (10 mg/mL), biotinylated human serum albumin from 50 to 150 mg diluted in 20 to 40 mL. One patient was not given
(HSA-biot; 20 mg/mL), and DOTA-biotin ligand (2 mg/mL, product biotinylated albumin (HSA-biot), whereas the others received a dose
code ST2210) dissolved in saline were supplied by Sigma-Tau S.p.A. ranging from 15 to 25 mg, 3 to 10 min before 111In-DOTA-biotin
i.f.r. Anhydrous sodium acetate (NaAc), acetic acid, and diethylene- administration. Liver and breast uptake, expressed as percentage of
triaminepentaacetic acid were purchased from Sigma-Aldrich Italy at the injected radioactivity, were monitored.
highest available purity. A NaAc buffer at 1 mol/L (pH 5.0) was
prepared using MilliQ water (q = 18 MV/cm) as previously described IART procedure
(12). Indium-111 chloride (111InCl3) in 0.05 N HCl was purchased Intrasurgical phase. In the phase I trial, the surgeon administered
from Mallinckrodt Medical B.V., whereas yttrium-90 chloride (90YCl3) 100 mg native avidin with three 10 mL syringes as 1 cm-apart multiple
in 0.04N HCl was obtained from Perkin-Elmer, Inc. injections into the tumoral-peritumoral bed and periareolar site, where
necessary, to percolate the index quadrant. Avidin injection occurred
Radiolabeling after either sentinel node biopsy or axillary dissection.
The radiolabeling of DOTA-biotin was carried out following a In the pilot therapeutic study, the dose for the subdermal avidination
previously described procedure (12). Briefly, a volume of NaAc buffer, of the skin lesion was 150 mg.
equal to that of the radionuclide MCl3 (M = 111In or 90Y) solution, was Postsurgical phase. Sixteen to 24 h after surgery, patients were given
mixed with a quantity of DOTA-biotin (Mw = 715) to achieve a specific radiolabeled biotin i.v. as a slow bolus injection. 111In-DOTA-biotin
activity of 2.65 MBq/nmol. The buffered DOTA-biotin was added to the activity was 108 F 9 MBq for patients (n = 10) enrolled in the phase I
MCl3 vial and then incubated in a water bath at 95jC for 30 min. After trial.
incubation, radiochemical purity was assessed by Silica Gel Instant Thin To chase the excess of free avidin, which had been drained over-
Layer Chromatography (ITLC-SG, Gelman); an aliquot of the radio- night by the lymphatic system toward the blood stream, patients were
labeled solution was mixed with a molar excess of avidin and given 20 mg/5 mL of HSA-biot via i.v. injection 10 min before
diethylenetriaminepentaacetic acid, then spotted in triplicate. Quanti- radioactive biotin administration. In the pilot therapeutic study,
tation of 111In/90Y – radiolabeled DOTA-biotin (R f = 0) and free the patient received 25 mg of HSA-biot as chase and, 10 min later,
amount of 111In/90Y complexed to diethylenetriaminepentaacetic acid she was co-injected i.v. with 1.2 GBq 90Y-DOTA-biotin for thera-
(R f = 1) was carried out by high-performance storage phosphor screen peutic purposes and 130 MBq 111In-DOTA-biotin for biodistribution
(Cyclone, Packard BioScience). purposes.
Patients Pharmacokinetic studies
Fifteen patients with breast cancer at stage T1-2N0-1, suitable for a To determine 111In-DOTA-biotin blood clearance and excretion rate,
quadrantectomy and axillary dissection (or sentinel lymph node blood samples were withdrawn at t = 5, 10, 30, and 60 min and t = 3, 5,
Table 1. Circulating avidin chase study
Case no. Avidin Avidin HSA-biotin Gap time Liver uptake Breast uptake
mass (mg) volume (mL) chase (mg) (min) (% injected activity) (% injected activity)
1 150 25 — — f9 f4
2 50 20 15 1 f5 f4
3 100 40 25 3 f2 f8
4 50 20 20 10 —30% ISOROI); and the low-uptake area (i.e., area between 30% and
10% ISOROI).
SAAM II software (15) was used to depict the kinetics of the
radioconjugate by an appropriate compartmental model and to obtain
the number of disintegrations [ND(h)] occurring in the source organs
for 90Y, on the assumption that the kinetics of biotin with either 111In
or 90Y would be identical.
Dose calculations were done for each patient according to the
medical internal radiation dose formalism using OLINDA/EXM
software (16), entering the ND(h) for all source organs. The absorbed
doses were calculated according to the patient/phantom mass ratio.
The self-dose in the breast area was calculated assuming uniform
activity distribution in spherical shaped tumors (Spheres Model
available in OLINDA/EXM). The ND(h) for the tumor area was derived
from the breast area time-activity curves.
The ND(h) in the red marrow was calculated from the ND(h) in
blood, assuming that no specific uptake would occur in bone marrow.
Uniform activity distribution as well as equivalent clearance in blood
and red marrow was also assumed. Due to the small size of the
radiolabel, specific activity in red marrow was considered equal to the
specific activity in blood (17).
To calculate the absorbed dose to the bladder wall, the ND(h) for
bladder contents was calculated according to the dynamic urinary bladder
model (18), based on the experimental curve of the cumulative activity
eliminated in the urine. The bladder was assumed to void every 1.5 h in
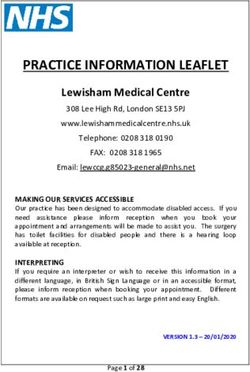
Fig. 1. Scintigraphy scan acquired at 90 to 120 h after f111MBq 111In-DOTA-biotin the first 8 h after injection (forced diuresis) and at every 4.8-h interval
i.v. injection. Patients received 150 mg avidin only (A); 50 mg avidin and 15 mg
HSA-biotin (B); and 100 mg avidin and 20 mg HSA-biotin (C). thereafter.
Biological effective dose: the linear-quadratic model
12, 16, 24, 36, and 48 h, assuming t = 0 at injection time. Urine was The linear-quadratic model enabled a comparison of doses released
collected over 48 h. The urinary tract was assumed to be the only through EBRT to those from IART and analysis of possible effects on
elimination route (13). nontarget organs (19, 20). In fact, we adopted the biological effective
Radioactivity in blood and urine samples was measured with a dose (BED) expression defined by:
gamma counter (Cobra II, Perkin-Elmer) with a 20% reading window
centered on the 173-keV peak of 111In. The efficiency of the X 1 T1=2rep X
BED ¼ Di þ ð Þ D2
gamma counter was determined by counting a calibrated source of i
a
b T1=2rep þ T1=2eff i i
111
In with the same geometry used for biological samples. The radio-
activity measurements were corrected for physical decay at injection where Di is the dose delivered per cycle i; T 1/2 rep is the repair half-time
time and expressed as a percentage of injected activity (IA%) versus of sublethal damage; and T 1/2 eff is the effective half-life of the
time. The time-activity curve in the blood was fitted with three- radiopharmaceutical in the specific tissue. The a/b ratio relates the
exponential function as described (13). The activity in urine samples
was used to obtain the cumulative IA% versus time eliminated through
the kidneys.
Imaging, biodistribution, and dosimetry
Whole-body transmission scans with 57Co-flood source were done
for attenuation correction purposes. At 1, 4, 24, 36, and 48 h after a
slow bolus injection of 111In-DOTA-biotin, standard scintigraphic
whole-body scans were acquired in anterior and posterior views with
a double-head gamma camera (GE Millennium VG) equipped with a
medium energy general purpose collimator.
Whole-body images were analyzed by the conjugated view method
(14). Regions of interest were drawn manually over the whole
body, breast region, and source organs (kidneys, heart, and lungs).
The same set of regions of interest was used for all scans. Counts
from the gamma-camera images were corrected for background,
scatter, and physical decay; biological time-activity curves were
obtained.
To further detect 111In-DOTA-biotin uptake and distribution in the
mammal gland and surrounding tissues, a single-photon emission
computed tomography scan was acquired over the breast region at t =
16 h.
The time-activity curve in the breast gland was created from single-
photon emission computed tomography and whole-body images. The
Fig. 2. Images from scintigraphy scans acquired at t = 1, 5, 16, and 40 h after
breast region was divided into three distinct areas: the high-uptake area 111
In-DOTA-biotin (111MBq) i.v. injection in a patient given 100-mg avidin on the
(i.e., 50% ISOROI, where all pixels/voxels have more than 50% of day of surgery and 20-mg HSA-biot for chase 10 min before radiocompound
maximum counts); the mean-uptake area (i.e., area between 50% and administration. Arrows, early and stable uptake in breast area.
Clin Cancer Res 2007;13(18 Suppl) September 15, 2007 5648s www.aacrjournals.orgIARTand Breast Cancer
Table 2. Dosimetric results
No. disintegrations [ND(h)] Absorbed doses (Gy/GBq)
Mean (SD) Min Max Mean (SD) Min Max
Heart 0.07 (0.05) 0.02 0.14 0.14 (0.11) 0.04 0.39
Kidneys 0.68 (0.28) 0.35 1.20 1.20 (0.42) 0.69 2.05
Lungs 0.11 (0.07) 0.05 0.22 0.07 (0.05) 0.01 0.15
Red marrow 0.12 (0.03) 0.09 0.18 0.05 (0.02) 0.03 0.10
Urinary bladder 0.80 (0.06) 0.72 0.87 1.39 (0.10) 1.24 1.55
Remainder of the body 5.14 (2.43) 2.69 8.91 0.06 (0.10) 0.03 0.11
Other organs — — — 0.05 (0.03) 0.03 0.10
High-uptake region 1.42 (1.01) 0.66 3.39 5.5 (1.1) 4.2 7.3
Mean-uptake region 1.77 (0.46) 1.27 2.41 5.1 (1.4) 3.3 7.7
Low-uptake region 2.09 (1.13) 0.98 4.01 2.1 (1.2) 1.3 3.0
111
NOTE: Number of disintegrations and absorbed doses throughout the body in 10 patients after In-DOTA-biotin injection.
intrinsic radiosensitivity (a) and the potential sparing capacity (b) to a fast, the IA% in the blood at t = 24 h was 0.15 F 0.10%,
specified tissue or effect. whereas the cumulative activity excreted in the urine was 81.4 F
For the breast region, we used T 1/2 rep = 1.5 h, a/b = 10 Gy (21); for 12.2% IA 24 h after injection.
the kidneys, we used T 1/2 rep = 2.8 h, a/b = 2.6 Gy (22). Dosimetry and biological effective dose. Using SAAM II
software, the ND(h) that occurred in the source organs for
90
Results Y was extrapolated (Table 2). The highest absorbed doses
were in the urinary bladder wall (1.4 F 0.1 Gy/GBq) and
Radiopharmaceutical preparation kidneys (1.2 F 0.4 Gy/GBq). The estimated absorbed dose to
DOTA-biotin was successfully labeled with 111In/90Y, rou- the red marrow was 0.05 F 0.02 Gy/GBq.
tinely achieving radiochemical purities z99.0%. In seven patients, the maximum uptake in breast area was at
t = 4 h. The other three had maximum uptake within 24 h after
Patients
injection. The breast area time-activity curve revealed an early
Patients ranged in age from 33 to 64 years. All had good and stable radioactive uptake in the target area (Fig. 3). The
performance status (Eastern Cooperative Oncology Group mean value of the ND(h) for the mean-uptake region of the
score = 0). Postoperative staging according to tumor-node- target tissue was 1.77 h, ranging from 1.27 to 2.41 h; the mean
metastasis classification showed six T1c (1-2 cm), one T1mic value of the absorbed dose to the mean-uptake breast region
(9%) liver uptake (Fig. 1A). Similarly, a short gap injection of 1.2 GBq of 90Y-DOTA-biotin and 130 MBq of
time between HSA-biot and 111In-DOTA-biotin injections led 111
In-DOTA-biotin (Fig. 4A), we extrapolated that the
to liver uptake (Fig. 1B; case no. 2: 5% and case no. 3: 2%). A
low mass of avidin (50 mg) was associated with inadequate
breast uptake (case no. 4: 0.4%) whereas 100-mg avidin seemed
to be the optimal dose to reach satisfactory breast uptake with
a 20-mg HSA-biot injection 10 min before radiolabeled biotin
administration (case no. 5: >4%; Fig. 1C).
An avidin dose ratio of 5:1 was considered appropriate for a
successful chase and led to 20 mg of HSA-biot.
Phase I trial
Patients enrolled in the phase I trial showed no clinical
adverse reactions: the intrasurgical injection of avidin was well
tolerated and no side effects were observed after the i.v.
injection of 111In-DOTA-biotin.
Imaging and biodistribution. The scintigraphic images
showed that the radiolabeled compound remained well
localized within the operated breast area with very negligible Fig. 3. 111In-DOTA-biotin time-activity curve in breast area (points, mean from
background in other tissues (Fig. 2). The blood clearance was 10 patients; bars, SD).
www.aacrjournals.org 5649s Clin Cancer Res 2007;13(18 Suppl) September 15, 2007Fig. 4. A, serial scans of patient with local
breast cancer recurrence, acquired at t = 1,
4, 24, 48, and 96 h after 90Y-DOTA-biotin
(1.2 GBq) and 111In-DOTA-biotin (130 MBq)
co-injection with 150-mg avidin and 25-mg
HSA-biotin as chase, show fast and stable
uptake in target area. B, follow-up images of
patient who underwent IART, documenting
objective response to therapy with
90
Y-biotin.
absorbed dose was 1.8 Gy in kidneys and 2.5 Gy in urinary range in tissue (R max = 11.3 mm). Thus, 90Y-DOTA-biotin is
bladder wall. The target area received a dose ranging from 8 to particularly suitable for radionuclide therapy, with the likeli-
10 Gy. The patient had an objective local response to IART hood of killing the majority of neoplastic cells related to the so-
therapy (Fig. 4B), documented by clinical inspection lasting called cross-fire effect (31), whereas 177Lu may be particularly
more than a year. Moreover, the patient had complete pain suitable for microscopic residual disease or nipple sparing
remission in the chest with consequent withdrawal of pain mastectomy, where it is crucial to avoid a high radiation dose to
relief drugs (morphine). the derma. Avidin-biotin – based pretargeting methods have
been used in clinical imaging and experimental therapy trials
Discussion for more than a decade (11, 30).
This study suggests that the IART procedure succeeds in
In an attempt to provide quality of life improvement through placing interstitial receptors (tissue avidination) able to bind
investigating patient-customized anticancer therapies, we pro- labeled DOTA-biotin 1 day after breast conservative surgery.
pose IART as a new procedure for partial breast irradiation in The scintigraphic images showed a fast and long-lasting
candidates for conservative breast surgery. uptake of labeled DOTA-biotin at the operated breast site. This
The simple two-step method of intraoperative locoregional area is therefore suitable for an efficient, targeted therapy.
avidin injection (first step) and 90Y-DOTA-biotin i.v. adminis- Through simulation studies based on in vivo pharmacokinetics
tration after 16 to 24 h (second step) relies on avidin-biotin and biodistribution of 111In-DOTA-biotin, we estimated the
chemical affinity and Yttrium radioisotope properties. In fact, absorbed doses and biological effective dose to the breast
avidin is a 66-kDa glycosylated and positively charged region and normal organs during treatment with 90Y-DOTA-
(isoelectric point ffi 10) glycoprotein with extremely high biotin.
affinity for the 244-Da vitamin H, biotin (k d = 10-15 mol/L; In the phase I trial, pharmacokinetics of labeled DOTA-biotin
ref. 23). Surgical intervention causes an inflammation reaction showed a rapid renal elimination, which, however, resulted in a
that increases capillary permeability and triggers cation- moderate dose to the kidney. The absorbed dose to the most
exchanging flows (24). Therefore, at the injection site, avidin involved nontarget organs (urinary bladder and kidneys) was
is retained for several days and may act as ‘‘artificial receptor for far from the threshold doses of tissue side effects, according to
radiolabeled biotin’’ (25, 26). Preclinical animal studies and the EBRT experience (32). However, these threshold doses are
prior clinical experience show that avidin injection in surgically not suitable for internal radionuclide therapies because the
created cavities is well tolerated (27 – 30). radiation dose delivered during such therapy differs in many
On the other hand, biotin can be easily labeled with 90Y or aspects from that delivered by external beam irradiation (33).
177
Lu through the chelating agent N,N¶,N 00,N-1,4,7,10-tetraa- Recently, the linear-quadratic model has been used to quantify
zacyclododecan-1,4,7,10-tetraacetic acid (DOTA). 90Y is a high- the dose-rate sparing concepts expressly for radionuclide
energy pure h-emitter (E ave, b = 0.935 MeV), with a relatively therapy, taking into account the different dose rate as compared
short physical half-life (T 1/2 = 64.1 h) and a long penetration with EBRT (34 – 36). In particular, for an injection of 3.7 GBq,
Clin Cancer Res 2007;13(18 Suppl) September 15, 2007 5650s www.aacrjournals.orgIARTand Breast Cancer the absorbed dose to the kidneys was 4.4 F 1.5 Gy, whereas the treatable with conservative surgery; multifocality, tumor loca- biological effective dose was 4.8 F 1.8 Gy, which is clearly tion, and size are not limiting factors. The surgeon injects lower than the threshold dose for the reported kidney toxicity avidin all around the tumor bed, without margin limitations or (22, 37). constraints. IART can be applied in all institutions where breast The pharmacokinetics herein reported is useful to calculate surgery is done and a nuclear medicine unit is available. the optimal injected activity of 90Y-DOTA-biotin. The radiation In our opinion, the combined use of IART followed by dose released to the breast region is f5 Gy/GBq (biological reduced EBRT is a valid approach to an easier, patient-tailored effective dose, 4.8 F 1.1 Gy/GBq) suitable for targeted accelerated irradiation after breast conservative surgery. radionuclide therapy. The estimated biological effective dose, Based on the pilot therapeutic study results and dosimetry according to the linear-quadratic model, would facilitate data herein reported, we consider further clinical development integration with EBRT treatment planning. IART has the great of randomized trials with IART in combination with EBRT fully advantage of potentially being applied to any breast cancer justified. References 1. Luini A, Gatti G, Galimberti V, et al. Conservative 13. Cremonesi M, Ferrari M, Chinol M, et al. Three-step of prosthetic vascular graft infection using avidin/ treatment of breast cancer: its evolution. Breast Can- radioimmunotherapy with yttrium-90 biotin: dosime- indium-111-biotin scintigraphy. J Nucl Med 1996;37: cer ResTreat 2005;94:195 ^ 8. try and pharmacokinetics in cancer patients. Eur J 55 ^ 61. 2.Veronesi U, Cascinelli N, Mariani L, et al. Twenty-year Nucl Med 1999;26:110 ^ 20. 26. Rusckowski M, Paganelli G, Hnatowich DJ, et al. follow-up of a randomized study comparing breast- 14. Siegel JA, Thomas SR, Stubbs JB, et al. Techniques Imaging osteomyelitis with streptavidin and indium- conservative surgery with radical mastectomy for ear- for quantitative radiopharmaceutical biodistribution 111-labeled biotin. J Nucl Med 1996;37:1655 ^ 62. ly breast cancer. N Eng J Med 2002;347:1227 ^ 32. data acquisition and analysis for use in human radia- 27. Axworthy DB, Reno JM, Hylarides MD, et al. Cure of 3. Athas WF, Adams-Cameron M, Hunt WC, Amir-Fazli tion dose estimates. MIRD Pamphlet no.16. J Nucl human carcinoma xenografts by a single dose of pre- A, Key CR. Travel distance to radiation therapy and re- Med 1999;40:S37 ^ 61. targeted yttrium-90 with negligible toxicity. Proc Natl ceipt of radiotherapy following breast-conserving sur- 15. Foster D, Barret P. Developing and testing integrated Acad Sci U S A 2000;97:1802 ^ 7. gery. J Natl Cancer Inst 2000;92:269 ^ 71. multicompartment models to describe a single-input 28. Paganelli G, Bartolomei M, Ferrari M, et al. Pre- 4.Veronesi U, Orecchia R, Luini A, et al. Full-dose intra- multiple-output study using the SAAM II software sys- targeted locoregional radioimmunotherapy with 90Y- operative radiotherapy with electrons during breast- tem. In: Proc. Sixth International Radiopharmaceutical. biotin in glioma patients: phase I study and preliminary conserving surgery: experience with 590 cases. Ann Dosimetry Symposium, Oak Ridge Institute for Science therapeutic results. Cancer Biother Radiopharm 2001; Surg 2005;242:101 ^ 6. and Education, 1998. 16:227 ^ 35. 5.Vicini FA, RemouchampsV,Wallace M, et al. Ongoing 16. Stabin MG, Sparks RB, Crowe E. OLINDA/EXM: the 29. Chinol M, De Cobelli O, Trifiro' G, et al. Localization clinical experience utilizing 3D conformal external second-generation personal computer software for of avidin in superficial bladder cancer: a potentially beam radiotherapy to deliver partial-breast irradiation internal dose assessment in nuclear medicine. J Nucl new approach for radionuclide therapy. Eur Urol in patients with early-stage breast cancer treated with Med 2005;46:1023 ^ 7. 2003;44:556 ^ 9. breast-conserving therapy. Int J Radiat Oncol Biol 17. Sgouros G. Bone marrow dosimetry for radioimmu- 30. Knox SJ, Goris ML,Tempero M, et al. Phase II trial of Phys 2003;57:1247 ^ 53. notherapy: theoretical considerations. J Nucl Med yttrium-90-DOTA-biotin pretargeted by NR-LU-10 an- 6. Polgar C, Sulyok Z, FodorJ, et al. Sole brachytherapy 1993;34:689 ^ 94. tibody/streptavidin in patients with metastatic colon of the tumor bed after conservative surgery for T1 18. Thomas SR, Stabin MG, Chin-Tu C, Samaratunga cancer. Clin Cancer Res 2000;6:406 ^ 14. breast cancer: five year results of a phase 1-2 study RC. MIRD Pamphlet no. 14: a dynamic urinary bladder 31. Schubiger PA, Alberto R, Smith A. Vehicles. Chela- and initial finding of a randomized phase 3 trial. J Surg model for radiation dose calculations. J Nucl Med tors, and radionuclides: choosing the ‘‘building block’’ Oncol 2002;80:121 ^ 8. 1992;33:783 ^ 802. of an effective therapeutic radioimmunoconjugate. 7. Vaidya JS, Tobias JS, Baum M, et al. TARGeted Intra- 19. Dale R. Dose-rate effects in targeted radiotherapy. Bionconjug Chem 1996;7:165 ^ 79. operative radiotherapy (TARGIT): an innovative ap- Phys Med Biol 1996;41:1187 ^ 4. 32. Emami B, Lyman J, Brown A, et al. Tolerance of nor- proach to partial-breast irradiation. Semin Radiat 20. Dale R. Use of the linear-quadratic radiobiological mal tissue to therapeutic irradiation. Int J Radiat Oncol Oncol 2005;15:84 ^ 91. model for quantifying kidney response in targeted radio- Biol Phys 1991;21:109 ^ 22. 8. Vicini FA, Baglan KL, Kestin LL, et al. Accelerated treat- therapy. Cancer Biother Radiopharm 2004;19:363 ^ 70. 33. Kassis AI, Adelstein SJ. Radiobiologic principles in mentof breastcancer. JClin Oncol 2001;19:1993 ^ 2001. 21. Rosenstein BS, Lymberis SC, Formenti SC. Biologic radionuclide therapy. J Nucl Med 2005;46:4 ^ 12S. 9. Paganelli G, Chinol M. Radioimmunotherapy: is avi- comparison of partial breast irradiation protocols. Int J 34. Dale R, Carabe-Fernandez A. The radiobiology of din-biotin pretargeting the preferred choice among Radiat Oncol Biol Phys 2004;60:1393 ^ 404. conventional radiotherapy and its application to radio- pretargeting methods? Eur J Nucl Med Mol Imaging 22. Barone R, Borson-Chazot F,Valkema R, et al. Patient- nuclide therapy. Cancer Biother Radiopharm 2005;20: 2003;30:773 ^ 6. specific dosimetry in predicting renal toxicity with 90Y- 47 ^ 51. 10. Grana C, Chinol M, Robertson C, et al. Pretargeted DOTATOC: relevance of kidney volume and dose rate in 35. Valkema R, Pauwels SA, Kvols LK, et al. Long-term adjuvant radioimmunotherapy with yttrium-90-biotin finding a dose-effect relationship. J Nucl Med 2005;46: follow-up of renal function after peptide receptor radi- in malignant glioma patients: a pilot study. Br J Cancer 99 ^ 106S. ation therapy (PRRT) with 90YDOTA0,Tyr3-octreotide 2002;86:207 ^ 12. 23. Yao Z, Zhang M, Sakahara H, Saga T, Arano Y, and177Lu-DOTA0,Tyr3-octreotate.JNuclMed2005;46:46: 11. Goldenberg DM, Sharkey RM, Paganelli G, Barbet J, Konishi J. Targeting of interperitoneal tumors with 46:83 ^ 91S. Chatal JF. Antibody pretargeting advances cancer avidin. J Natl Cancer Inst 1998;90:25 ^ 9. 36. Konijnenberg MW. Is the renal dosimetry for 90Y- radioimmunodetection and radioimmunotherapy. J 24. Lazzeri E, Pauwels EK, Erba PA, et al. Clinical DOTA 0,Tyr 3 -octretide accurate enough to predict Clin Oncol 2006;24:823 ^ 34. feasibility of two-step streptavidin/111In-biotin scin- thresholds for individual patients ? Cancer Biother 12. Urbano N, Papi S, Ginanneschi M, et al. Evaluation tigraphy in patients with suspected vertebral osteo- Radiopharm 2003;18:619 ^ 25. of a new biotin-dota conjugate for pretargeted anti- myelitis. Eur J Nucl Med Mol Imaging 2004;31: 37. Cremonesi M, Ferrari M, Bodei L, Tosi G, Paganelli body guided radioimmunotherapy (PAGRITR). Eur J 1505 ^ 11. G. Dosimetry in peptide radionuclide receptor therapy: Nucl Med Mol Imaging 2007;34:68 ^ 77. 25. Samuel A, Paganelli G, Chiesa R, et al. Detection a review. J Nucl Med 2006;47:1467 ^ 75. www.aacrjournals.org 5651s Clin Cancer Res 2007;13(18 Suppl) September 15, 2007
You can also read