Perspective: Genetic Defects in the Etiology of Congenital Hypothyroidism
←
→
Page content transcription
If your browser does not render page correctly, please read the page content below
0013-7227/02/$15.00/0 Endocrinology 143(6):2019 –2024
Printed in U.S.A. Copyright © 2002 by The Endocrine Society
Perspective: Genetic Defects in the Etiology of
Congenital Hypothyroidism
Abstract clude thyroid (hemi)agenesis, ectopic thyroid tissue, cysts of
Congenital hypothyroidism affects about 1:3000 to 1:4000 the thyroglossal duct, and thyroid hypoplasia (2, 3). In the
infants and may be caused by defects in thyroidal ontogeny vast majority of all cases, thyroid dysgenesis is sporadic, but
in about 2% it is familial (4), an observation supporting the
Downloaded from https://academic.oup.com/endo/article-abstract/143/6/2019/2989288 by guest on 06 February 2020
or hormone synthesis. The impressive advances in molecular
genetics led to the characterization of numerous genes that possibility of a genetic etiology. The higher prevalence of
are essential for normal development and hormone produc- thyroid dysgenesis in Hispanics and Caucasians in compar-
tion of the hypothalamic-pituitary-thyroid axis. Mutations in ison to Blacks, the predominance of thyroid dysgenesis in
many of these genes now provide a molecular explanation girls, and the higher prevalence of associated malformations
for a subset of the sporadic and familial forms of congenital also suggest the presence of genetic factors in the pathogen-
hypothyroidism. esis of congenital hypothyroidism (5). More recently,
Defects in one of the multiple steps required for normal detailed analyses of familial and sporadic patients with con-
hormone synthesis account for about 10% of cases with con- genital hypothyroidism, with or without associated pheno-
genital hypothyroidism. They are typically recessive and typic features, have unraveled the molecular basis in a small
therefore more common in inbred families. In the vast ma- fraction of these patients (2, 3). In the remaining 5% of cases,
jority of patients, congenital hypothyroidism is sporadic and the hypothyroidism is thought to result from the transpla-
associated with thyroid dysgenesis, a spectrum of develop- cental transfer of maternal antibodies to the child.
mental defects, which includes the absence of detectable
Hypothalamic and pituitary defects resulting
thyroid tissue, ectopic tissue, and thyroid hypoplasia. The
in hypothyroidism
molecular defects known to date only explain a minority of
these cases and include mutations in the paired box tran- Several clinical reports have suggested isolated TRH de-
scription factor PAX8, and the thyroid transcription factors ficiency as a cause of central hypothyroidism (6, 7), but there
TTF1 and TTF2. It is likely that a further subset of patients are currently no reports on patients with documented defects
with thyroid dysgenesis have defects in other transacting in the TRH gene. Mice with targeted disruption of the Trh
proteins or elements of the signaling pathways controlling gene are hypothyroid and, rather surprisingly, their TSH is
growth and function of thyrocytes. In other instances, thy- elevated, but its biological activity is reduced (8). Similar
roid dysgenesis may be a polygenic disease or have a mul- biochemical constellations with elevated TSH of reduced
tifactorial basis. Aside from providing fundamental insights bioactivity have been reported in some individuals with cen-
into the ontogeny and the pathophysiology of the thyroid, tral hypothyroidism (9) (see Table 1).
the characterization of the molecular basis of congenital hy- Resistance to TRH in pituitary thyrotrophs was discovered
pothyroidism may have growing importance for genetic test- in a boy with isolated central hypothyroidism, and absent
ing and counseling in the future. rise of TSH and PRL in response to TRH (10). Mutational
analysis of gene encoding the TRH receptor, a member of the
Introduction G protein-coupled seven transmembrane receptors, revealed
Normal thyroid function is essential for development, compound heterozygous inactivating mutations (10).
growth and metabolic homeostasis. The prerequisites for an Isolated hereditary TSH deficiency is a rare cause of central
euthyroid metabolic state include a normally developed thy- hypothyroidism and can be caused by recessive mutations in
roid gland, a properly functioning system for thyroid hor- the TSH chain (11, 12). In these patients, TSH is unmea-
mone synthesis, and adequate iodine intake. In iodine suf- surable or very low, and the administration of TRH does not
ficient regions, permanent congenital hypothyroidism result in a rise in serum TSH. The levels and the function of
affects about 1:3000 to 1:4000 newborns, and it is one of the the other pituitary hormones are normal, including an ad-
most common preventable causes of mental retardation (1). equate rise of PRL in response to TRH. Among the five
In about 10% of all cases, congenital hypothyroidism is the currently known mutations, some are recurrent in certain
consequence of defects in one of the steps of thyroid hormone populations suggesting a founder effect, whereas others
synthesis, inborn errors of metabolism referred to as dyshor- have been found independently in sporadic and familial
mogenesis. A heterogeneous group of developmental abnor- patients from different ethnic origins. A subset of these mu-
malities, thyroid dysgenesis, accounts for about 85% of all tations is predicted to disrupt heterodimerization with the
cases with congenital hypothyroidism. These anomalies in- glycoprotein hormone ␣-chain, whereas others lead to pre-
mature truncations (12, 13).
Genetic defects in the development and function of the
Abbreviations: CPHD, Combined pituitary hormone deficiency;
PAX8, paired box transcription factor; PROP1, Prophet of Pit1; RTH, pituitary gland can result in various forms of combined pi-
resistance to thyroid hormone; TG, thyroglobulin; TPO, thyroperoxi- tuitary hormone deficiency (CPHD). Patients with CPHD
dase; TTF, thyroid transcription factor. present with impaired production and secretion of one or
20192020 Endocrinology, June 2002, 143(6):2019 –2024 Kopp • Perspective
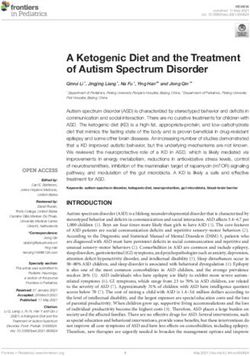
TABLE 1. Genetic defects associated with abnormal thyroid development and hormone synthesis
Phenotype Gene(s) Inheritance Chromosome
Agenesis with cleft palate, choanal atresia, spiky hair TTF2 (FKLHL15) AR 9q22
Hypoplasia or ectopy PAX8 AD 2q12-q14
Other, unidentified
Combined pituitary hormone deficiency PROP1 AR 5q
POU1F1 (P1T1) AR, AD 3p11
LHX3 AR 9q34.3
HESX1 AR, AD 3p21.2-21.1
Other, unidentified
Isolated TRH deficiency TRH? AR 3p
Mutation not
Downloaded from https://academic.oup.com/endo/article-abstract/143/6/2019/2989288 by guest on 06 February 2020
identified
Central hypothyroidism TRH receptor AR 8p23
Absent rise of TSH, PRL in response to TRH
Central hypothyroidism TSH subunit AR 1p13
Absent rise of TSH in response to TRH
Euthyroid hyperthyrotropinemia (partial inactivation) TSH receptor AR 14q13
Overt hypothyroidism with hypoplasia (complete) Other, unidentified
Pseudohypoparathyroidism Ia GNAS1 Heterozygous mutation 20q13.2
⫹ tissue-specific
imprinting
Goiter, impaired iodide uptake NIS AR 19p12-13.2
Pendred’s syndrome PDS/SCL26A4 AR 7q31
Partial organification defect
Goiter, organification defect TPO AR 2p25
Goiter, organification defect THOX2? AD? 15q15
Other, unidentified
Goiter, qualitative or quantitative TG defect TG AR, (AD?) 8q24
Goiter, loss of MIT and DIT Dehalogenase
Gene not identified
Thyroid dysfunction, ataxia, respiratory distress TTF1 (NKX2A) Haploinsufficiency 14q13
Resistance to thyroid hormone with variable features TR AD, (AR) 3p24.3
of hypo- and hyperthyroidism
Other, unidentified AD, AR
OMIM, Online Mendelian Inheritance in Men; AR, autosomal recessive; AD, autosomal dominant. For other abbreviations, see text.
several anterior pituitary hormones that may include TSH. screening of patients presenting with a wide spectrum of
CPHD has been documented in patients with mutations in congenital pituitary dysfunctions. A subset of these patients
four transcription factors involved in pituitary development was indeed found to be heterozygous for HESX1 mutations
and hormone expression (POU1F1, PROP1, LHX3, HESX1) (18). Heterozygous HESX1 mutations result in various con-
(14 –18). Many of these discoveries were preceded by the stellations of pituitary hormone deficiencies, and the phe-
molecular analysis of inbred mouse strains or mice with notype is variable among family members with the same
targeted disruption of these genes. Mutations in the pitu- mutation.
itary-specific transcription POU1F1 (PIT1) result in deficien-
cies of GH, PRL, and TSH. Depending on the location of the
Genetic defects in thyroid development
mutation, the mode of transmission is recessive or dominant.
PROP1 (Prophet of PIT1) is a paired-like homeodomain fac- The mature mammalian thyroid gland evolves from two
tor acting upstream of POU1F1 and its recessive inactivation distinct embryologic structures, the thyroid diverticulum, an
disrupts the ontogenesis, differentiation, and function of so- endodermal component that gives rise to thyroid follicular
matotropes, lactotropes, thyrotropes, and gonadotropes. cells, and the neuroectodermal ultimobranchial bodies that
There is, however, variability in the phenotypic expression differentiate into the parafollicular calcitonin-producing C
among CPHD patients with the same or distinct PROP-1 cells. Following migration and fusion of the two cell popu-
mutations (19). Recessive mutations in LHX3, a LIM home- lations, thyroid follicular cells undergo further differentia-
odomain transcription factor, also cause CPHD of all anterior tion that is characterized by the expression of genes that are
pituitary hormones with the exception of ACTH (16). In essential for thyroid hormone synthesis such as the TSH
addition, these patients have a rigid cervical spine and a receptor, the sodium-iodide symporter, thyroperoxidase
limited ability to rotate the head (16). Familial septo-optic (TPO), and thyroglobulin (TG). Thyroid hormone is detect-
dysplasia, a syndromic form of CPHD associated with optic able in the fetus at about gestational wk 11.
nerve hypoplasia and agenesis of midline structures in the During the last few years, it has become apparent that
brain, can be caused by homozygous mutations in HESX1 (or mutations in transcription factors that govern thyroid de-
RPX/Rathke pouch homeobox), a paired-like class of ho- velopment and gene expression may result in syndromic and
meobox transcription factors (17). The observation that a nonsyndromic forms of thyroid dysgenesis, and these ob-
small proportion of mice heterozygous for a Hesx1 null allele servations are corroborated by similar observation in murine
has a milder form of septo-optic dysplasia prompted further knockout models (20 –23).Kopp • Perspective Endocrinology, June 2002, 143(6):2019 –2024 2021
Heterozygous mutations in PAX8, a paired domain tran- cal apraxia, mental retardation, and neonatal respiratory dis-
scription factor involved in thyroid development and ex- tress (32, 33).
pression of the TPO and TG genes (24), have been docu-
mented and characterized in sporadic and familial patients
Resistance to TSH
with thyroid hypoplasia or ectopy (20, 25, 26). It is currently
unclear why mutation of a single PAX8 allele is sufficient to The response to bioactive TSH may be impaired at the level
result in congenital hypothyroidism in humans, a finding of the thyroid follicular cells. Total insensitivity to TSH re-
that contrasts with the observation that mice heterozygous sults in a small hypoplastic thyroid gland and reduced syn-
for a disrupted Pax8 locus do not display a pathological thesis and secretion of thyroid hormones. Of note, a similar
phenotype (21). In humans, the biochemical and morpho- morphologic and biochemical phenotype may occur in pa-
logical phenotype may vary among patients with the same tients with mutations in PAX8 and emphasizes the limita-
Downloaded from https://academic.oup.com/endo/article-abstract/143/6/2019/2989288 by guest on 06 February 2020
PAX8 mutation (20, 26). Underlying mechanisms may in- tions of morphologic criteria. Resistance to TSH may be
clude incomplete penetrance, a phenomenon associated with caused by various molecular mechanisms.
mutations in other PAX genes. Alternatively, the phenotypic In a subset of these patients, the molecular cause consists
expression may be modulated by modifier genes. of mutations in the TSH receptor that are partially or com-
Homozygosity for recessive mutations in the forkhead/ pletely inactivating (34 –37). In partial resistance, TSH is el-
winged-helix domain transcription factor FKLH15, com- evated, but the peripheral hormone levels are normal, a
monly referred to TTF2, results in a syndromic form of constellation referred to as euthyroid hyperthyrotropinemia
thyroid dysgenesis with the eponym Bamforth-Lazarus (34). In these patients, the size of the thyroid is normal or
syndrome (22, 27). This phenotype, described in two enlarged. Homozygous or compound heterozygous inacti-
brothers from a consanguineous family, includes thyroid vating mutations in the TSH receptor have been found in
agenesis, cleft palate, choanal atresia, bifid epiglottis, and several patients with overt hypothyroidism and thyroid hy-
spiky hair (22, 27). Mice homozygous for a disrupted Ttf2 poplasia (35–37), as well as in the thoroughly characterized
gene die shortly after birth and are profoundly hypothy- hyt/hyt mouse that is severely hypothyroid and has a nor-
roid (23). They exhibit either small lingual thyroid rem- mally located, hypoplastic gland (38). Because of absent
nants or have complete thyroid agenesis, and they also tracer uptake in scintigraphic studies, several of these pa-
have cleft palates. These findings support the important tients were initially diagnosed with thyroid agenesis, but
role of TTF2, which is also involved in transcriptional careful ultrasonographic evaluation revealed the presence of
control of the TG and the TPO gene promoters (28), in hypoplastic thyroid tissue. TG levels are thought to be a
thyroid development. useful marker for demonstrating the presence of thyroid
Thyroid transcription factor 1 (NKX2A, TITF-1, TTF1, or tissue in neonates. However, the TG levels in patients with
thyroid specific enhancer-binding protein T/ebp) is a ho- thyroid hypoplasia associated with TSH receptor mutations
meobox domain transcription factor of the NKX2 family in- were undetectable, normal, or elevated.
volved in the development of the gland and in transcriptional The hallmark of pseudohypoparathyroidism Ia consists of
control of the TG, TPO, and TSH receptor genes (24). It is also resistance to PTH. However, patients with this disorder may
expressed in the lung, the forebrain and the pituitary gland. also exhibit resistance to the glycoprotein hormones TSH,
Mice with targeted disruption of both TTF1 alleles survive LH, and FSH (39). In addition to the clinical and biochemical
throughout gestation, but die at birth from respiratory failure features related to hormone resistance, these patients have
(29). The lung is severely hypoplastic and consists of a sac- characteristic skeletal and developmental abnormalities such
like structure without bronchioli, alveoli or lung parenchyma as short stature, brachydactyly and ectopic calcifications (Al-
(29). Both the thyroid gland and pituitary gland are com- bright’s hereditary osteodystrophy) (39). The unresponsive-
pletely absent, and the hypothalamus is severely malformed. ness to these hormones in pseudohypoparathyroidism Ia is
Several screenings of patients with thyroid dysgenesis for the consequence of mutations in the maternal copy of the
mutations in the TTF1 gene were negative. The observation GNAS1 (Gs␣ subunit) gene, in combination with tissues-
of a newborn with severe respiratory distress, a normally specific imprinting (39). If the mutation is transmitted on the
located thyroid gland and elevated TSH levels and a het- paternal allele, the phenotype is limited to Albright’s hered-
erozygous deletion on chromosome 14q13 encompassing the itary osteodystrophy (39).
TTF1 locus suggested that haploinsufficiency for TTF1 could Unresponsiveness to TSH can also be inherited as an au-
be associated with impaired lung maturation and thyroid tosomal dominant trait, but the molecular defect remains to
function (30). The detection of a similar heterozygous dele- be defined (40).
tion of chromosome 14q12–13.3 in two female siblings with
congenital thyroid dysfunction and recurrent acute respira-
Genetic defects in thyroid hormone synthesis
tory distress gave further support to this concept (31). Very
recently, a few additional patients with hyperthyrotropine- Normal iodide uptake at the basolateral membrane by the
mia, neonatal respiratory distress and ataxia associated with perchlorate-sensitive sodium/iodide symporter NIS is a
missense or frameshift mutations, or chromosomal deletions rate-limiting step in thyroid hormone synthesis (41– 43), and
of the TTF-1 gene have been reported (32, 33). The TSH levels several homozygous or compound heterozygous mutations
were only mildly elevated and the thyroid was normal in size have been identified in individuals with hypothyroidism
and position. The hallmark of this phenotype is the neuro- associated with impaired iodide uptake (for review, see Ref.
logic deficit, which includes ataxia or choreoathetosis, trun- 43). Many of these patients have a diffuse or nodular goiter,2022 Endocrinology, June 2002, 143(6):2019 –2024 Kopp • Perspective
little or no uptake of radioiodine, and a decreased saliva/ early childhood. The metabolic status is variable and, de-
serum radioiodine ratio. pending on the severity of the defect, the patients are hy-
Efflux of iodide at the apical membrane of thyroid follic- pothyroid, subclinically hypothyroid, or euthyroid. The se-
ular cells is at least in part mediated by pendrin (SCL26A4), rum TG levels may be low, normal, or elevated. The
a member of the Solute Carrier Family 26A (44 – 46). Muta- radioiodine uptake is elevated. TG defects are usually trans-
tions in the SCL26A4 gene cause Pendred’s syndrome, an mitted in an autosomal recessive manner; however, an au-
autosomal recessive disorder traditionally defined by the tosomal dominant mode of inheritance has been proposed in
triad of sensorineural congenital deafness, goiter, and a par- one kindred (60).
tially positive perchlorate test. The partial discharge of ra- Molecular analysis of several TG mutations found in pa-
dioiodine after the administration of perchlorate indicates tients with congenital hypothyroidism and in the cog/cog
that the gland has an impaired ability to organify iodide. mouse, which all present with goiters, reveal that at least
Downloaded from https://academic.oup.com/endo/article-abstract/143/6/2019/2989288 by guest on 06 February 2020
Although some patients with Pendred’s syndrome present some of these alterations result in a secretory defect and thus
with congenital hypothyroidism (47), the majority of indi- an endoplasmic reticulum storage disease (61). In contrast to
viduals are clinically and biochemically euthyroid, at least these TG defects associated with goiter development, the
under conditions of normal nutritional iodide intake. Fur- recessive dwarf rdw/rdw rat displays a nongoitrous form of
thermore, the prevalence of goiters may be lower in patients congenital primary hypothyroidism caused by a Tg gene
with pendrin mutations living in iodine-replete regions (48). mutation (62, 63). The identification of a mutation in the Tg
Pds knockout mice are profoundly deaf, but they do not gene as a cause of nongoitrous hypothyroidism in the rdw/
display an enlarged thyroid or abnormal thyroid hormone rdw rat challenges the previously held generalization that
levels (49). It is currently unknown whether they have a nongoitrous congenital hypothyroidism is caused by thyroid
partial organification defect (49). dysgenesis or defects in TSH signaling.
In the follicular lumen, the iodination of tyrosine residues After entering the follicular cell, TG is hydrolyzed, and T4
in TG, and the coupling of iodinated tyrosines to generate T4 and T3 are secreted into the blood at the basolateral mem-
and T3, is dependent on the normal function of the glyco- brane. The iodotyrosines MIT and DIT, which are much more
sylated hemoprotein TPO. TPO defects are among the most abundant in the TG molecule, are deiodinated by an intra-
frequent causes of inborn errors of thyroid hormone syn-
thyroidal dehalogenase and recycled for hormone synthesis.
thesis. Mutations in the TPO gene have been reported in
Several patients with leakage of MIT and DIT from the thy-
numerous families with a partial or total organification de-
roid and urinary secretion of these metabolites have been
fect (50 –52). In a recent survey, total iodide organification
reported (64). The disorder appears to be inherited in an
defects were estimated to occur in approximately 1:66,000
autosomal recessive fashion. Expression of the phenotype,
neonates, and the majority of these infants were homozygous
which may include goiter and hypothyroidism, is thought to
or compound heterozygous for mutations in the TPO gene
be dependent on the nutritional iodide intake. The intrathy-
(52). This observation suggests that most patients with a total
roidal dehalogenase has not been characterized at the mo-
iodide organification defect harbor inactivating mutations in
this gene. lecular level.
The iodination and coupling reactions are dependent on
hydrogen peroxide (H2O2) as an essential cofactor. Recently, Defects in thyroid hormone action
two NADPH oxidases, THOX1 and THOX2 (also referred to
as LNOX or DUOX), that may be part of this system have Resistance to thyroid hormone (RTH) is characterized by
been cloned (53, 54). Sequence alterations in the THOX2 gene, decreased responsiveness to thyroid hormone (65, 66). Bio-
which is more abundantly expressed at the apical membrane chemically, the syndrome is defined by elevated free thyroid
of thyrocytes, were reported in several patients with a total hormones and an inappropriately normal or elevated level of
iodide organification defect, but their functional significance TSH. The clinical spectrum is highly variable and ranges
remains unclear (55). In a family with two affected siblings from isolated biochemical abnormalities to a constellation of
presenting with hypothyroidism, goiter, and iodine organi- features that includes goiter, variable features of hyper- and
fication defects, nearly undetectable thyroid NADPH oxi- hypothyroidism, short stature, delayed bone maturation,
dase activities were measured in tissue slices (56). It has been and attention deficit hyperactivity disorder (65, 67). RTH is
proposed that the cause of the organification defect in these most commonly caused by autosomal dominant mutations
patients is the result of impaired Ca2⫹/NAD(P)H-dependent in TR that exert a dominant negative effect (65, 66). In one
H2O2 generation (56), but the exact molecular defect remains family, RTH was caused by the loss of both TR alleles (68).
to be defined. Defective H2O2 generation has also been More recently, familial cases of RTH without linkage to the
thought to explain the phenotype in some individuals with TR locus have been reported indicating the possibility of
euthyroid goiter and abnormal iodide organification (3). nonallelic heterogeneity (69, 70).
TG, a homodimeric glycoprotein, is a key element in thy- The diagnosis of RTH is important to avoid inappropriate
roid hormone synthesis and storage. It is encoded by a very treatment of the condition (65), and although rare, it is a
large gene spanning more than 300 kb and containing 48 diagnostic consideration when neonatal screening shows
exons (for recent reviews, see Refs. 57 and 58). Mutations in mildly increased TSH levels (71). While asymptomatic pa-
the TG gene have been reported in a number of animal tients do not require intervention, treatment may be required
models and human patients (58, 59). Unless treated with in a subset of patients to ameliorate features of hypo- or
levothyroxine, these patients typically present with goiter in hyperthyroidism (72).Kopp • Perspective Endocrinology, June 2002, 143(6):2019 –2024 2023
Perspective 11. Hayashizaki Y, Hiraoka Y, Tatsumi Y, Hashimoto T, Furuyama J, Miyai K,
Nishijo K, Matsura M, Kohno H, Labbe A, Matsubara K 1990 Deoxyribo-
The isolation and the identification of genes controlling nucleic acid analysis of five families with familial inherited thyroid stimulating
thyroid development and thyroid hormone synthesis con- hormone deficiency. J Clin Endocrinol Metab 71:792–796
12. Pohlenz J, Dumitrescu A, Aumann U, Koch G, Melchior R, Prawitt D,
tinues to provide unique insights into the ontogenesis and Refetoff S 2002 Congenital secondary hypothyroidism caused by exon skip-
physiology of the hypothalamic-pituitary-thyroid axis, as ping due to a homozygous donor splice site mutation in the TSH-subunit
well as a more precise understanding of (congenital) disor- gene. J Clin Endocrinol Metab 87:336 –339
13. Medeiros-Neto G, Heodotou DT, Rajan S, Kommareddi S, de Lacerda L,
ders at the molecular level. It has become apparent that Sandrini R, Boguszewski MCS, Hollenberg AN, Radovick S, Wondisford FE
thyroid dysgenesis is, at least in part, a genetic disorder. 1996 A circulating, biologically inactive thyrotropin caused by a mutation in
the beta subunit gene. J Clin Invest 97:1250 –1256
However, the molecular defects known to date only account 14. Radovick S, Nations M, Du Y, Berg LA, Weintraub BD, Wondisford FE 1992
for a minority of cases of thyroid dysgenesis. It is likely that A mutation in the POU-homeodomain of Pit-1 responsible for combined pi-
a further subset of patients with thyroid dysgenesis have tuitary hormone deficiency. Science 257:1115–1118
Downloaded from https://academic.oup.com/endo/article-abstract/143/6/2019/2989288 by guest on 06 February 2020
15. Wu W, Cogan JD, Pfäffle RW, Dasen JS, Frisch H, O’Connell SM, Flynn SE,
defects in other transacting proteins that remain to be dis- Brown MR, Mullis PE, Parks JS, Phillips JAI, Rosenfeld MG 1998 Mutations
covered. In other instances, thyroid dysgenesis may be a in PROP1 cause familial combined pituitary hormone deficiency. Nat Genet
polygenic disease or have a multifactorial basis. Genetic test- 18:147–149
16. Netchine I, Sobrier ML, Krude H, Schnabel D, Maghnie M, Marcos E, Duriez
ing is currently of limited importance in patients with con- B, Cacheux V, Moers A, Goossens M, Gruters A, Amselem S 2000 Mutations
genital hypothyroidism. However, analyses at the molecular in LHX3 result in a new syndrome revealed by combined pituitary hormone
level may be useful and informative in familial cases and deficiency. Nat Genet 25:182–186
17. Dattani MT, Martinez-Barbera JP, Thomas PQ, Brickman JM, Gupta R,
sporadic patients presenting with additional phenotypic Martensson IL, Toresson H, Fox M, Wales JK, Hindmarsh PC, Krauss S,
characteristics. Beddington RS, Robinson IC 1998 Mutations in the homeobox gene HESX1/
Hesx1 associated with septo-optic dysplasia in human and mouse. Nat Genet
19:125–133
Peter Kopp, M.D. 18. Thomas PQ, Dattani MT, Brickman JM, McNay D, Warne G, Zacharin M,
Division of Endocrinology, Metabolism & Molecular Cameron F, Hurst J, Woods K, Dunger D, Stanhope R, Forrest S, Robinson
IC, Beddington RS 2001 Heterozygous HESX1 mutations associated with
Medicine isolated congenital pituitary hypoplasia and septo-optic dysplasia. Hum Mol
Northwestern University Genet 10:39 – 45
Chicago, Illinois 60611 19. Flück C, Deladoey J, Rutishauser K, Eble A, Marti U, Wu W, Mullis PE 1998
Phenotypic variability in familial combined pituitary hormone deficiency
caused by a PROP1 gene mutation resulting in the substitution of Arg–⬎Cys
Acknowledgments at codon 120 (R120C). J Clin Endocrinol Metab 83:3727–3734
20. Macchia PE, Lapi P, Krude H, Pirro MT, Missero C, Chiovato L, Souabni A,
Received February 14, 2002. Accepted February 14, 2002. Baserga M, Tassi V, Pinchera A, Fenzi G, Grüters A, Busslinger M, DiLauro
Address all correspondence and requests for reprints to: Peter Kopp, R 1998 PAX8 mutations associated with congenital hypothyroidism caused by
M.D., Division of Endocrinology, Metabolism & Molecular Medicine, thyroid agenesis. Nat Genet 19:83– 86
21. Mansouri A, Chowdhury K, Gruss P 1998 Follicular cells of the thyroid gland
Northwestern University, Tarry 15, 303 East Chicago Avenue, Chicago, require Pax8 gene function. Nat Genet 19:87–90
Illinois 60611. E-mail: p-kopp@northwestern.edu. 22. Clifton-Bligh RJ, Wentworth JM, Heinz P, Crisp MS, John R, Lazarus JH,
Because of space constraints, only selected references could be in- Ludgate M, Chatterjee VK 1998 Mutation of the gene encoding human TTF-2
cluded in this article, and numerous publications of interest had to be associated with thyroid agenesis, cleft palate and choanal atresia. Nat Genet
omitted. 19:399 – 401
23. De Felice M, Ovitt C, Biffali E, Rodriguez-Mallon A, Arra C, Anastassiadis
K, Macchia PE, Mattei MG, Mariano A, Scholer H, Macchia V, Di Lauro R
References 1998 A mouse model for hereditary thyroid dysgenesis and cleft palate. Nat
Genet 19:395–398
1. New England congenital hypothyroidism collaborative 1981 Effects of neo-
24. Damante G, DiLauro R 1994 Thyroid-specific gene expression. Biochim Bio-
natal screening for hypothyroidism: prevention of mental retardation by treat-
phys Acta 1218:255–266
ment before clinical manifestation. Lancet 2:1095–1098
25. Vilain C, Rydlewski C, Duprez L, Heinrichs C, Abramowicz M, Malvaux P,
2. Gillam MP, Kopp P 2001 Genetic regulation of thyroid development. Curr
Renneborg B, Parma J, Costagliola S, Vassart G 2001 Autosomal dominant
Opin Pediatr 13:358 –363
3. Gillam MP, Kopp P 2001 Genetic defects in thyroid hormone synthesis. Curr transmission of congenital thyroid hypoplasia due to loss-of-function mutation
Opin Pediatr 13:364 –372 of PAX8. J Clin Endocrinol Metab 86:234 –238
4. Castanet M, Polak M, Bonaiti-Pellie C, Lyonnet S, Czernichow P, Leger J 2001 26. Congdon T, Nguyen LQ, Nogueira CR, Habiby RL, Medeiros-Neto G, Kopp
Nineteen years of national screening for congenital hypothyroidism: familial P 2001 A novel mutation (Q40P) in PAX8 associated with congenital hypo-
cases with thyroid dysgenesis suggest the involvement of genetic factors. J Clin thyroidism and thyroid hypoplasia: evidence for phenotypic variability in
Endocrinol Metab 86:2009 –2014 mother and child. J Clin Endocrinol Metab 86:3962–3967
5. Devos H, Rodd C, Gagne N, Laframboise R, Van Vliet G 1999 A search for 27. Bamforth JS, Hughes IA, Lazarus JH, Weaver CM, Harper PS 1989 Congenital
the possible molecular mechanisms of thyroid dysgenesis: sex ratios and hypothyroidism, spiky hair, and cleft palate. J Med Genet 26:49 –51
associated malformations. J Clin Endocrinol Metab 84:2502–2506 28. Zannini M, Avantaggiato V, Biffali E, Arnone MI, Sato K, Pischetola M,
6. Niimi H, Inomata H, Sasaki N, Nakajima H 1982 Congenital isolated thy- Taylor BA, Phillips SJ, Simeone A, Di Lauro R 1997 TTF-2, a new forkhead
rotrophin releasing hormone deficiency. Arch Dis Child 57:877– 878 protein, shows a temporal expression in the developing thyroid which is
7. Katakami H, Kato Y, Inada M, Imura H 1984 Hypothalamic hypothyroidism consistent with a role in controlling the onset of differentiation. EMBO J
due to isolated thyrotropin-releasing hormone (TRH) deficiency. J Endocrinol 16:185–197
Invest 7:231–233 29. Kimura S, Hara Y, Pineau T, Fernandez-Salguero P, Fox CH, Ward JM,
8. Yamada M, Saga Y, Shibusawa N, Hirato J, Murakami M, Iwasaki T, Hashi- Gonzalez FJ 1996 The T/ebp null mouse: thyroid-specific enhancer-binding
moto K, Satoh T, Wakabayashi K, Taketo MM, Mori M 1997 Tertiary hy- protein is essential for the organogenesis of the thyroid, lung, ventral forebrain,
pothyroidism and hyperglycemia in mice with targeted disruption of the and pituitary. Genes Dev 10:60 – 69
thyrotropin-releasing hormone gene. Proc Natl Acad Sci USA 94:10862–10867 30. Devriendt K, Vanhole C, Matthis G, De Zegher F 1998 Deletion of thyroid
9. Beck-Peccoz P, Amr S, Menezes-Ferreira MM, Faglia G, Weintraub BD 1985 transcription factor-1 gene in an infant with neonatal thyroid dysfunction and
Decreased receptor binding of biologically inactive thyrotropin in central respiratory failure. N Engl J Med 338:1317–1318
hypothyroidism. Effect of treatment with thyrotropin-releasing hormone. 31. Iwatani N, Mabe H, Devriendt K, Kodama M, Miike T 2000 Deletion of
N Engl J Med 312:1085–1090 NKX2.1 gene encoding thyroid transcription factor-1 in two siblings with
10. Collu R, Tang J, Castagné J, Lagacé G, Masson N, Huot C, Deal C, Delvin hypothyroidism and respiratory failure. J Pediatr 137:272–276
E, Faccenda E, Eidne KA, van Vliet G 1997 A novel mechanism for isolated 32. Pohlenz J, Dumitrescu A, Zundel D, Martine U, Schonberger W, Refetoff S,
central hypothyroidism: inactivating mutations in the thyrotropin-releasing Hyperthyrotropinemia, respiratory distress and ataxia associated with a mu-
hormone receptor gene. J Clin Endocrinol Metab 82:1361–1365 tation in the thyroid transcription factor 1 (TTF-1) gene. Program of the 83rd2024 Endocrinology, June 2002, 143(6):2019 –2024 Kopp • Perspective
Annual Meeting of The Endocrine Society, Denver, Colorado, 2001 (Abstract large inbred Amish kindred: power and limits of homozygosity mapping.
OR43-3) J Clin Endocrinol Metab 84:1061–1071
33. Schuetz BR, Krude H, Biebermann H, von Moers A, Schnabel D, Toennies 52. Bakker B, Bikker H, Vulsma T, de Randamie JS, Wiedijk BM, De Vijlder JJ
H, Schwarz S, Neitzel H, Grueters A, Loss of fuction mutations in the NKX2–1 2000 Two decades of screening for congenital hypothyroidism in The Neth-
gene define a new syndrome with CNS, thyroid and lung impairment. Pro- erlands: TPO gene mutations in total iodide organification defects (an update).
gram of the 83rd Annual Meeting of The Endocrine Society, Denver, Colorado, J Clin Endocrinol Metab 85:3708 –3712
2001 (Abstract OR59-3) 53. Dupuy C, Ohayon R, Valent A, Noel-Hudson MS, Deme D, Virion A 1999
34. Sunthornthepvarakul T, Gottschalk ME, Hayashi Y, Refetoff S 1995 Resis- Purification of a novel flavoprotein involved in the thyroid NADPH oxidase.
tance to thyrotropin caused by mutations in the thyrotropin-receptor gene. Cloning of the porcine and human cDNAs. J Biol Chem 274:37265–37269
N Engl J Med 332:155–160 54. De Deken X, Wang D, Many MC, Costagliola S, Libert F, Vassart G, Dumont
35. Abramowicz MJ, Duprez L, Parma J, Vassart G, Heinrichs C 1997 Familial JE, Miot F 2000 Cloning of two human thyroid cDNAs encoding new members
congenital hypotyroidism due to inactivating mutation of the thyrotropin of the NADPH oxidase family. J Biol Chem 275:23227–23233
receptor causing profound hypoplasia of the thyroid gland. J Clin Invest 55. Moreno JC, Bikker H, de Randamie J, Wiedijk BM, van Trotsenburg P,
99:3018 –3024 Kempers MJ, Vulsma T, de Vijlder JJM, Ris-Stalpers C 2000 Mutations in the
36. Refetoff S, Sunthornthepvarakul T, Gottschalk M, Hayashi Y 1996 Resistance ThOX2 gene in patients with congenital hypothyroidism due to iodide or-
Downloaded from https://academic.oup.com/endo/article-abstract/143/6/2019/2989288 by guest on 06 February 2020
to thyrotropin and other abnormabilities of the thyrotropin receptor. Recent ganification defects. Endocr J 47(Suppl):107 (Abstract 008)
Prog Hormone Res 51:97–122 56. Figueiredo MD, Cardoso LC, Ferreira AC, Campos DV, da Cruz Domingos
37. Kopp P 2001 The TSH receptor and its role in thyroid disease. Cell Mol Life M, Corbo R, Nasciutti LE, Vaisman M, Carvalho DP 2001 Goiter and hypo-
Sci 58:1301–1322 thyroidism in two siblings due to impaired Ca⫹2/NAD(P)H-dependent H2O2-
38. Stein SA, Oates EL, Hall CR, Grumbles RM, Fernandez LM, Taylor NA, generating activity. J Clin Endocrinol Metab 86:4843– 4848
Puett D, Jin S 1994 Identification of a point mutation in the thyrotropin 57. Mendive FM, Rivolta CM, Moya CM, Vassart G, Targovnik HM 2001
receptor of the hyt/hyt hypothyroid mouse. Mol Endocrinol 8:129 –138 Genomic organization of the human thyroglobulin gene: the complete intron-
39. Weinstein LS, Yu S, Warner DR, Liu J 2001 Endocrine manifestations of exon structure. Eur J Endocrinol 145:485– 496
stimulatory G protein ␣-subunit mutations and the role of genomic imprinting. 58. van de Graaf SA, Ris-Stalpers C, Pauws E, Mendive FM, Targovnik HM, de
Endocr Rev 22:675–705 Vijlder JJ 2001 Up to date with human thyroglobulin. J Endocrinol 170:307–321
40. Xie J, Pannain S, Pohlenz J, Weiss RE, Moltz K, Morlot M, Asteria C, Persani 59. Medeiros-Neto G, Targovnik HM, Vassart G 1993 Defective thyroglobulin
L, Beck-Peccoz P, Parma J, Vassart G, Refetoff S 1997 Resistance to thyro- synthesis and secretion causing goiter and hypothyroidism. Endocr Rev 14:
tropin (TSH) in three families is not associated with mutations in the TSH 165–183
receptor or TSH. J Clin Endocrinol Metab 82:3933–3940 60. De Vijlder JJM, Baas F, Koch CAM, Kok K, Gons M 1983 Autosomal dom-
inant inheritance of a thyroglobulin abnormality suggests cooperation of sub-
41. Dai G, Levy O, Carrasco N 1996 Cloning and characterization of the thyroid
units in hormone formation. Ann Endocrinol 44:36
iodide transporter. Nature 379:458 – 460
61. Kim PS, Arvan P 1998 Endocrinopathies in the family of endoplasmic retic-
42. Smanik P, Liu Q, Furminger T, Ryu K, Xing S, Mazzaferri E, Jhiang S 1996
ulum (ER) storage diseases: disorders of protein trafficking and the role of ER
Cloning of the human sodium iodide symporter. Biochem Biophys Res Com-
molecular chaperones. Endocr Rev 19:173–202
mun 226:339 –345
62. Hishinuma A, Furudate S, Oh-Ishi M, Nagakubo N, Namatame T, Ieiri T
43. De la Vieja A, Dohan O, Levy O, Carrasco N 2000 Molecular analysis of the
2000 A novel missense mutation (G2320R) in thyroglobulin causes hypothy-
sodium/iodide symporter: impact on thyroid and extrathyroid pathophysi-
roidism in rdw rats. Endocrinology 141:4050 – 4055
ology. Physiol Rev 80:1083–1105
63. Kim PS, Ding M, Menon S, Jung CG, Cheng JM, Miyamoto T, Li B, Furudate
44. Everett LA, Glaser B, Beck JC, Idol JR, Buchs A, Heyman M, Adawi F, Hazani S, Agui T 2000 A missense mutation G2320R in the thyroglobulin gene causes
E, Nassir E, Baxevanis AD, Sheffield VC, Green ED 1997 Pendred syndrome non-goitrous congenital primary hypothyroidism in the WIC-rdw rat. Mol
is caused by mutations in a putative sulphate transporter gene (PDS). Nat Endocrinol 14:1944 –1953
Genet 17:411– 422 64. Medeiros-Neto G, Stanbury JB 1994 The iodotyrosine deiodinase defect. In:
45. Royaux IE, Suzuki K, Mori A, Katoh R, Everett LA, Kohn LD, Green ED 2000 Medeiros-Neto G, Stanbury JB, eds. Inherited disorders of the thyroid system.
Pendrin, the protein encoded by the Pendred syndrome gene (PDS), is an apical Boca Raton, FL: CRC Press; 139 –159
porter of iodide in the thyroid and is regulated by thyroglobulin in FRTL-5 65. Refetoff S, Weiss RE, Usala SJ 1993 The syndromes of resistance to thyroid
cells. Endocrinology 141:839 – 845 hormone. Endocr Rev 14:348 –99
46. Gillam M, Karamanoglu Arseven O, Rutishauser J, Waeber Stephan C, Kopp 66. Weiss RE, Refetoff S 2000 Resistance to thyroid hormone. Rev Endocr Metab
P, Functional characterization of pendrin and two naturally occurring mutants: Disord 1(1–2):97–108
evidence for pendrin-mediated iodide efflux. Proc 73rd Annual Meeting of the 67. Brucker-Davis F, Skarulis MC, Grace MB, Benichou J, Hauser P, Wiggs E,
American Thyroid Association, Washington DC, 2001 (Abstract 196), p 265 Weintraub BD 1995 Genetic and clinical features of 42 kindreds with resistance
47. Gonzalez Trevino O, Karamanoglu Arseven O, Ceballos C, Vives V, Ramirez to thyroid hormone. Ann Int Med 123:572–583
R, Gomez VV, Medeiros-Neto G, Kopp P 2001 Clinical and molecular analysis 68. Takeda K, Sakurai A, DeGroot LJ, Refetoff S 1992 Recessive inheritance of
of three Mexican families with Pendred’s syndrome. Eur J Endocrinol 144:1–9 thyroid hormone resistance caused by complete deletion of the protein-coding
48. Gausden E, Armour JA, Coyle B, Coffey R, Hochberg Z, Pembrey M, Britton region of the thyroid hormone receptor- gene. J Clin Endocrinol Metab
KE, Grossman A, Reardon W, Trembath R 1996 Thyroid peroxidase: evidence 74:49 –55
for disease gene exclusion in Pendred’s syndrome. Clin Endocrinol 44:441– 446 69. Weiss R, Hayashi Y, Nagaya T, Petty K, Murata Y, Tunca H, Seo H, Refetoff
49. Everett LA, Belyantseva IA, Noben-Trauth K, Cantos R, Chen A, Thakkar SI, S 1996 Dominant inheritance of resistance to thyroid hormone not linked to
Hoogstraten-Miller SL, Kachar B, Wu DK, Green ED 2001 Targeted disrup- defects in the thyroid hormone receptor ␣ or  genes may be due to a defective
tion of mouse Pds provides insight about the inner-ear defects encountered in co-factor. J Clin Endocrinol Metab 81:4196 – 4223
Pendred syndrome. Hum Mol Genet 10:153–161 70. Pohlenz J, Weiss RE, Macchia PE, Pannain S, Lau IT, Ho H, Refetoff S 1999
50. Abramowicz MJ, Targovnik HM, Varela V, Cochaux P, Krawiec L, Pisarev Five new families with resistance to thyroid hormone not caused by mutations
MA, Propato FVE, Juvenal G, Chester HA, Vassart G 1992 Identification of in the thyroid hormone receptor  gene. J Clin Endocrinol Metab 84:3919 –3928
a mutation in the coding sequence of the human thyroid peroxidase gene 71. Weiss RE, Balzano S, Scherberg NH, Refetoff S 1990 Neonatal detection of
causing congenital goiter. J Clin Invest 90:1200 –1204 generalized resistance to thyroid hormone. JAMA 264:2245–2250
51. Pannain S, Weiss RE, Jackson CE, Dian D, Beck JC, Sheffield VC, Cox N, 72. Weiss R 1999 Management of patients with resistance to thyroid hormone.
Refetoff S 1999 Two different mutations in the thyroid peroxidase gene of a Thyroid Today 12:1–11You can also read